Translate this page into:
Recurrent purpura: A clue to Sjögren's syndrome
Correspondence Address:
Hao Chen
No. 12, Jiangwang Temple Street, Xuanwu District, Nanjing, Jiangsu Province
China
| How to cite this article: Gan L, Chen H, Sun JF. Recurrent purpura: A clue to Sjögren's syndrome. Indian J Dermatol Venereol Leprol 2020;86:335 |
Sir,
As we know, purpura is one of the clinicopathologic entities which presents as the initial manifestation of a variety of disorders. Hence an accurate diagnosis of the cause of purpura is absolutely essential for further management of the condition. Sjögren's syndrome is a chronic, autoimmune disease characterized by inflammation of the lacrimal and salivary glands resulting in dryness of the eyes and mouth. However, it can also present with various extraglandular manifestations including skin lesions. Here we present a difficult to diagnose case of Sjögren's syndrome which presented initially as recurrent purpura.
A man in his 30's presented with multiple episodes of purpura on his lower extremities for the past 8 years. He was once diagnosed as Henoch–Schonlein purpura and pigmentary purpuric dermatosis but there was no improvement with treatment. There was no associated joint pain or raynaud's phenomenon. On examination there were multiple purpuric macules distributed all over the lower extremities [Figure - 1] and [Figure - 2]. Skin biopsy showed a large amount of hemosiderin in the dermis [Figure - 3]. Routine examination of blood and urine as well as coagulation function tests were normal. Liver function test showed total protein, albumin, and globulin to be 87.4, 45, and 42 g/L, respectively. Serum electrophoresis, immunofixation, and immunoglobulin tests showed a polyclonal hypergammaglobulinemia with a high level of IgG. Hence, the diagnosis of hypergammaglobulinemic purpura of Waldenström was considered. Furthermore, a high titer of antinuclear antibody (1:1000 dilution) and positive anti-SSA and anti-SSB antibodies pointed towards an association with Sjögren's syndrome. The final diagnosis was confirmed by the symptoms of dry eye and xerostomia and also positive Schirmer's test, fluorescein corneal staining, and tear break-up time. The patient was started on a daily regimen of 15 mg oral prednisone and 75 mg dipyridamole for 3 months and he showed marked improvement in the symptoms.
 |
| Figure 1: Multiple 3 to 5 mm, bright to dusky red macules distributed diffusely on the lower legs which merge to form reticulate pattern |
 |
| Figure 2: Close up view of the purpuric lesions |
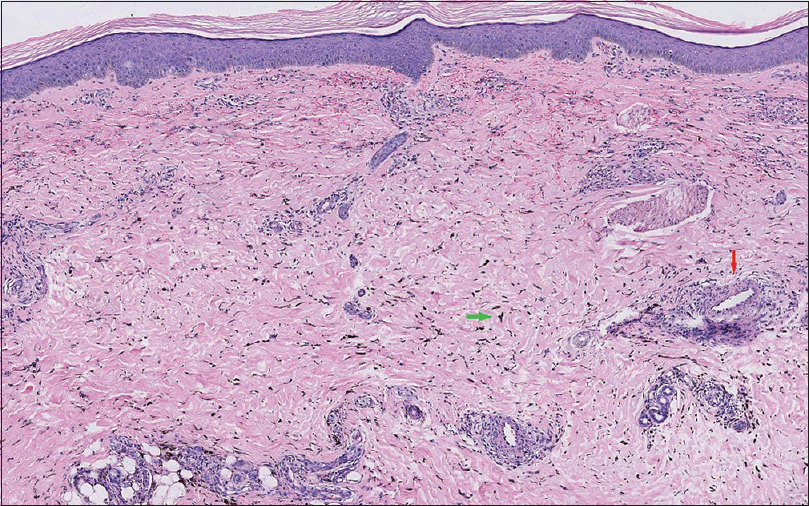 |
| Figure 3: A large amount of hemosiderin (green arrow), swelling of vascular endothelial cells (red arrow), bleeding, along with lymphocytic infiltration in the superficial dermis. (hematoxylin and eosin, 50x) |
Hypergammaglobulinemic purpura of Waldenström is a rare syndrome characterized by recurrent episodes of purpura occurring mainly on legs and dorsa of feet. Histopathological examination can show a range of manifestations includingsimple hemorrhage, mild perivascular lymphocytic infiltrate and leukocytoclastic vasculitis. The pathogenesis of the disease remains incompletely understood. Some argue that small circulating immune complexes may play an important role.[1] When an underlying cause cannot be found out, it is considered as primary hypergammaglobulinemic purpura of Waldenström, even some of them could develop features of autoimmune disease during the course of the disease. The most common association is Sjögren's syndrome and occasionally rheumatoid arthritis, lupus erythematosus, and hematologic malignancy.[2] Hypergammaglobulinemic purpura of Waldenström could have been induced in Sjögren's syndrome by an autoimmune mechanism through the activation of B cells and overproduction of gammaglobulin thereby indicating an association between them. Reduction in the levels of circulating immune complexes following plasmapheresis and intake of mycophenolate mofetil also points towards relation in the immunopathogenesis of both diseases.[3]
Our patient presented with recurrent purpura without overt manifestations of Sjögren's syndrome. In Sjögren's syndrome there are a great number of non-sicca symptoms which might arise before the onset of ocular and oral dryness, including skin lesions, among which vasculitis is common. Also a noteworthy point is that in as many as 66% of patients with Sjögren's syndrome, autoantibodies appear years before the onset of symptoms.[4] In our patient, the positive autoantibodies helped us to trace back the history and perform sicca evaluation, which led us to the final diagnosis. Clinically, purpuric lesions can be roughly categorized based on their extent and distribution pattern. Laboratory tests to look for thrombocytopenia, coagulopathies and vasculitis should be done. Early histopathological examination is of great importance. Routine blood and urine examination must be definitely done. Liver function test and testing for antibodies of hepatitis B, hepatitis C and HIV should be done. Once the serum globulin level is found to be increased, serum protein electrophoresis, immunofixation, and estimation of immunoglobulin levels should be performed to find out the type and amount of the immunoglobulin and to figure out the presence of monoclonal gammaglobulinemia. Antinuclear antibody profile can be done to look for autoimmune diseases. In addition, the presence of purpura should prompt an evaluation for cryoglobulinemia. All these investigations along with the clinical data will help us to rule out cryoglobulinemic purpura, thrombocytopenic purpura, Henoch-Schonlein purpura, pigmentary purpuric dermatosis, monoclonal gammopathy, and lymphoma.
In short, recognition of the special clinicopathologic features of recurrent purpura will help us arrive at an accurate diagnosis even when the patient lacks other typical manifestations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
CAMS Innovation Fund for Medical Sciences (CIFMS-2017-I2M-1-017). Innovation Research on Critical Diseases (2016ZX320014).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Lewin JM, Hunt R, Fischer M, Kamino H, Franks AG Jr. Hypergammaglobulinemic purpura of Waldenström. Dermatol Online J 2012;18:2.
[Google Scholar]
|
| 2. |
Nihei Y, Tanikawa M, Seki M, Suzuki S, Tanikawa A, Ohara K, et al. Acase of atypical inflammatory myositis with hypergammaglobulinemic purpura. J Neurol Sci 2016;367:275-7.
[Google Scholar]
|
| 3. |
Waldman MA, Callen JP. Mycophenolate mofetil treatment of a patient with hyperglobulinemic purpura. J Am Acad Dermatol 2004;51:667-9.
[Google Scholar]
|
| 4. |
Xu X, Zhu T, Wu D, Zhang L. Sjögren's syndrome initially presented as thrombotic thrombocytopenic purpura in a male patient: A case report and literature review. Clin Rheumatol 2018;37:1421-6.
[Google Scholar]
|
Fulltext Views
10,234
PDF downloads
2,420





