Translate this page into:
Recurrent solitary sclerotic fibroma (storiform collagenoma) on the foot: An unusual clinical presentation
Corresponding author: Maurizio Romagnuolo, Dermatology Unit, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy. maurizio.romagnuolo@unimi.it
-
Received: ,
Accepted: ,
How to cite this article: Romagnuolo M, Moltrasio C, Alberti-Violetti S, Riva D, Barberi F, Di Benedetto A, et al. Recurrent solitary sclerotic fibroma (storiform collagenoma) on the foot: An unusual clinical presentation. Indian J Dermatol Venereol Leprol. 2024;90:223–6. doi: 10.25259/IJDVL_762_2022
Dear Editor,
Sclerotic fibroma is a rare soft-tissue tumour with less than 100 cases described in the literature. It could be associated with the spectrum of PTEN hamartoma tumour syndrome cutaneous manifestations or presents as an acquired, solitary lesion.1 Even though it represents a benign neoplasm, local recurrence has been described in rare cases.1 Here we report a case of a recurrent solitary sclerotic fibroma.
A 54-year-old Indian woman was referred to our dermatology department for evaluation of a lesion on the left foot which was excised six years before (histological documentation was not available), but then recurred and enlarged during the last year. The patient was in good general health.
Clinical examination revealed an erythematous, irregularly shaped, woody-at-palpation nodule of 4 × 3 cm, adherent to the epidermis on the medial surface of the left foot. Similar papular lesions were visible near the nodule [Figures 1a and b]. The patient stated that the lesions were growing slowly and were painful on palpation. A recent magnetic resonance imaging of the left foot showed a hypointense unique lesion located in the dermis, with no connection to the deeper muscular-tendinous fascia with an asymmetrical growth. No other cutaneous findings were present. Personal and family history of PTEN hamartoma syndrome was negative. Clinical differential diagnosis included atypical fibroxanthoma and dermatofibrosarcoma protuberans. A 4 mm punch biopsy of the nodule for histopathological examination was performed.
The resected biopsy specimen was formalin-fixed, paraffin-embedded, and then processed for haematoxylin and eosin staining.
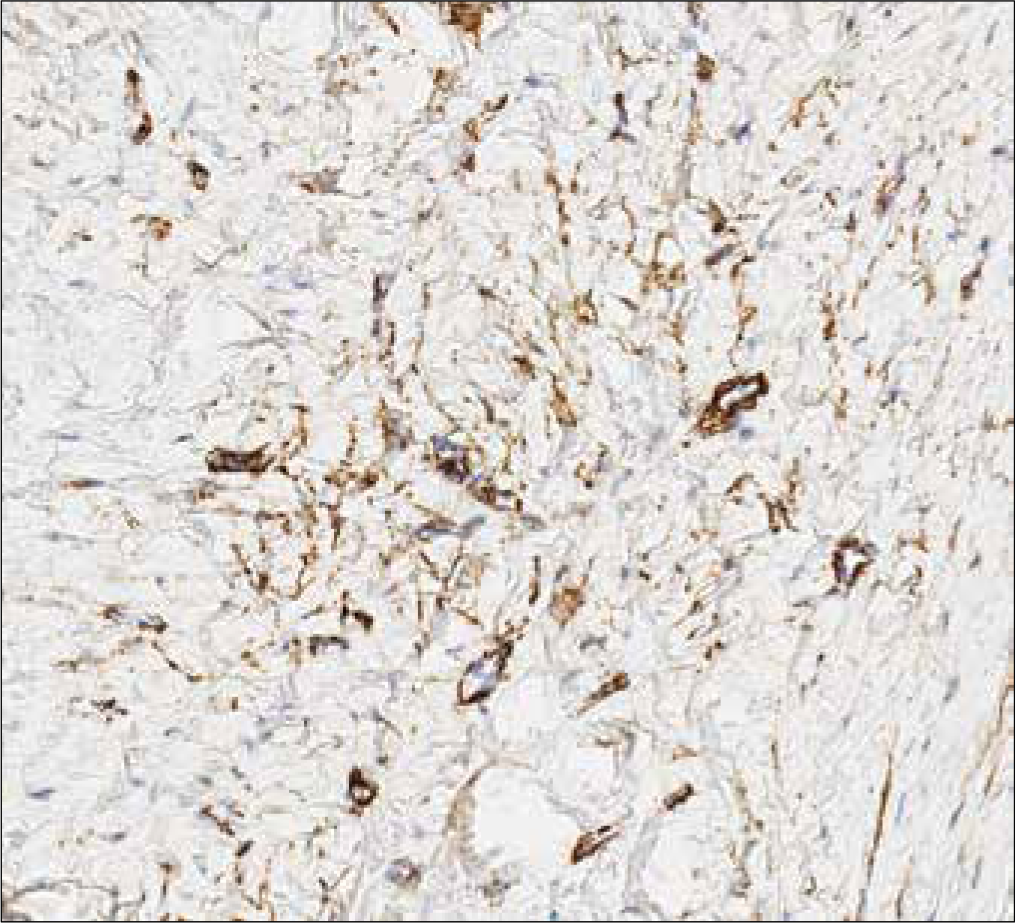
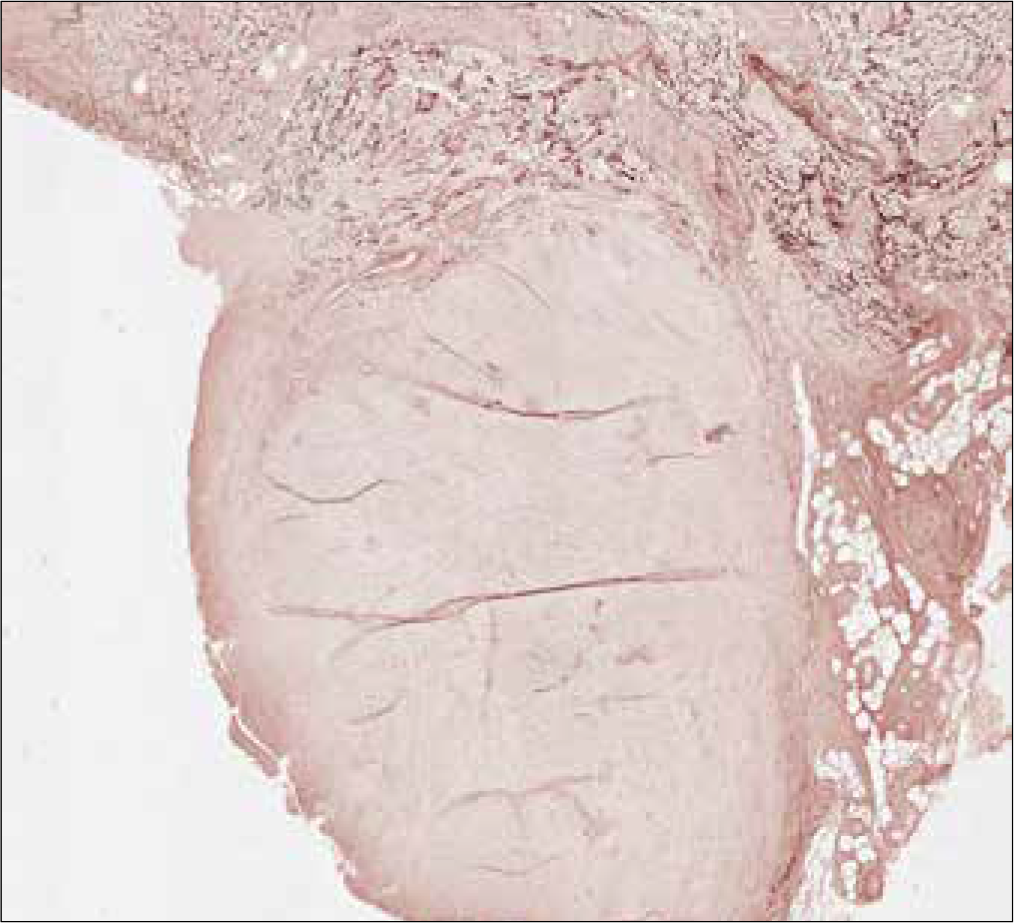
Histopathology revealed a well-circumscribed, non-encapsulated, dermal lesion. The epidermis was uninvolved with a spared subepidermal “grenz zone” [Figure 2a]. The lesion was composed of hyalinized thick collagen bundles arranged in a storiform pattern and separated by a slit-like cleft [Figure 2b], and cytologically by monomorphous spindle elements without mitotic figures; no significant atypia was observed [Figure 2b]. Immunohistochemical analysis showed negative staining for S100, CD99 and CD68, whereas few spindle cells were faintly positive for CD34 [Figures 2c and d], factor XIII and smooth muscle actin [Figure 2e]. Elastic fibres were significantly reduced within the lesion compared to the surrounding dermis [Figure 2f].

- A multilobulated lesion on the medial surface of the left foot of the patient composed of an erythematous-to-brown nodule of 4 × 3 cm and three papulo-nodular lesions

- Details of the lesion showing the bigger nodule with a scaly surface and the neighbouring smaller lesions embedded in the epidermis
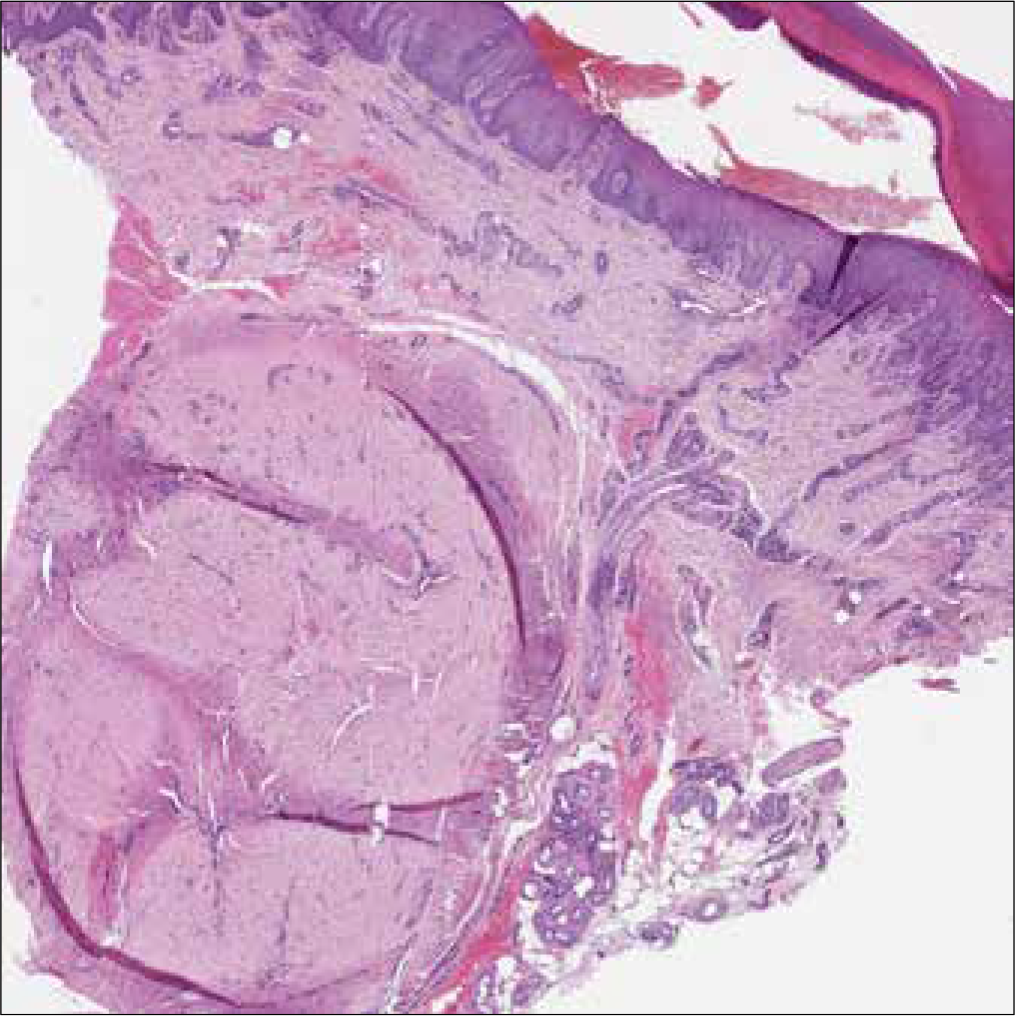
- A well-demarcated, non-encapsulated, hypocellular dermal lesion with an uninvolved epidermis (H&E staining, 100×)
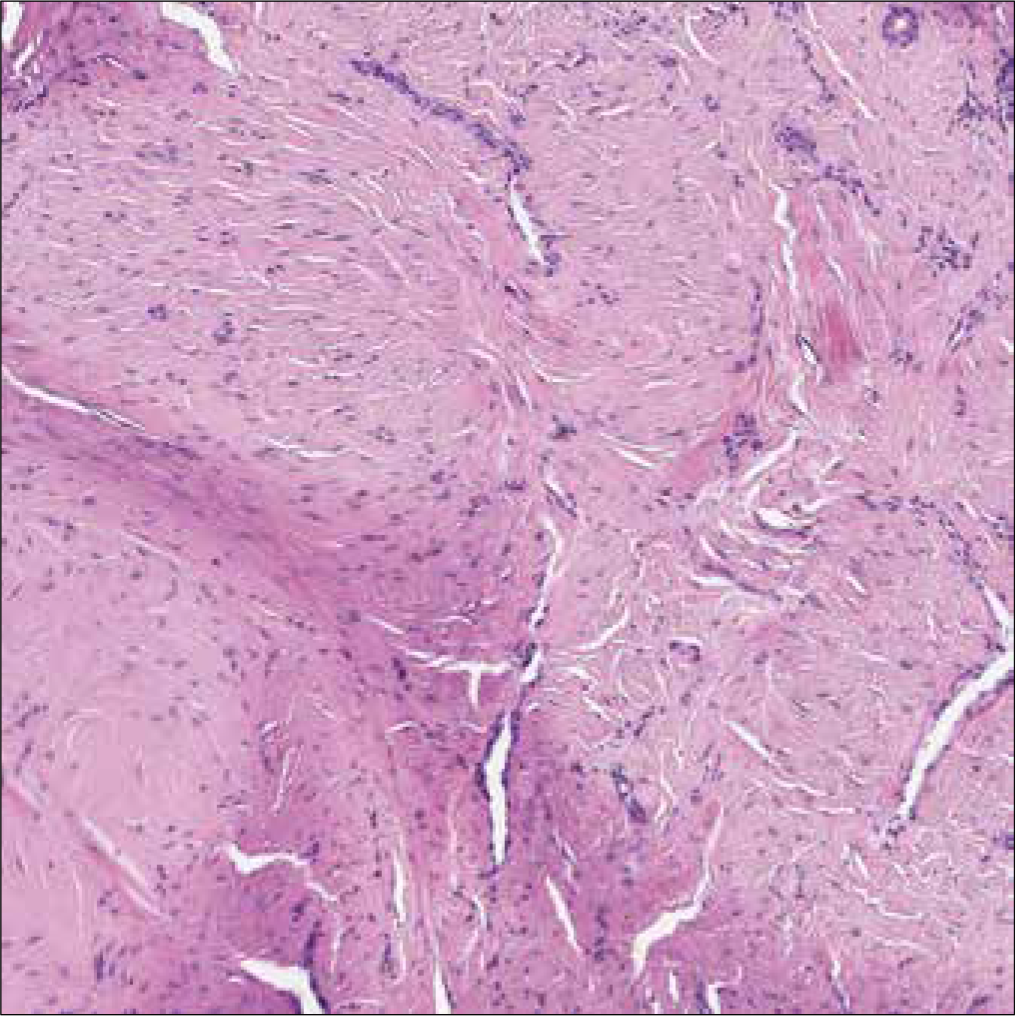
- Histopathology showing hyalinized collagen bundles arranged in a storiform pattern and separated by a prominent cleft (H&E staining, 400×)
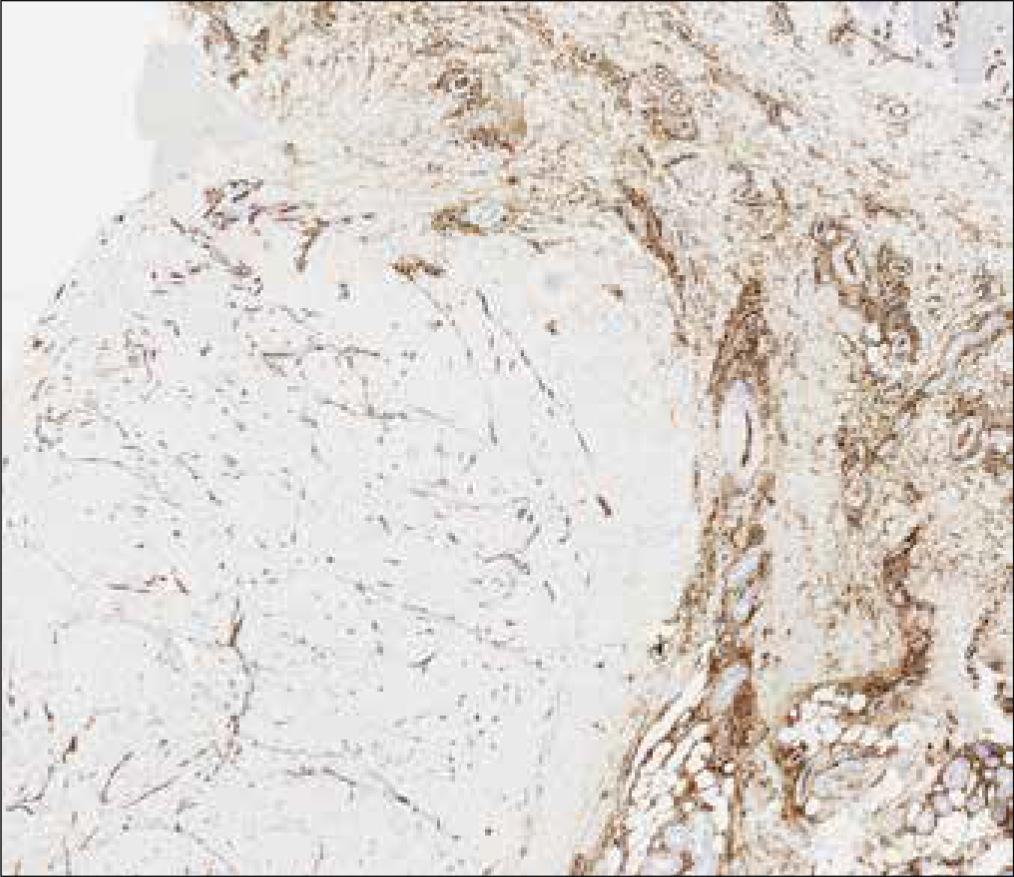
- Scattered CD34 positive spindle cells located at the periphery of the lesion together with strongly positive endothelial cells (CD34 staining, 100×)
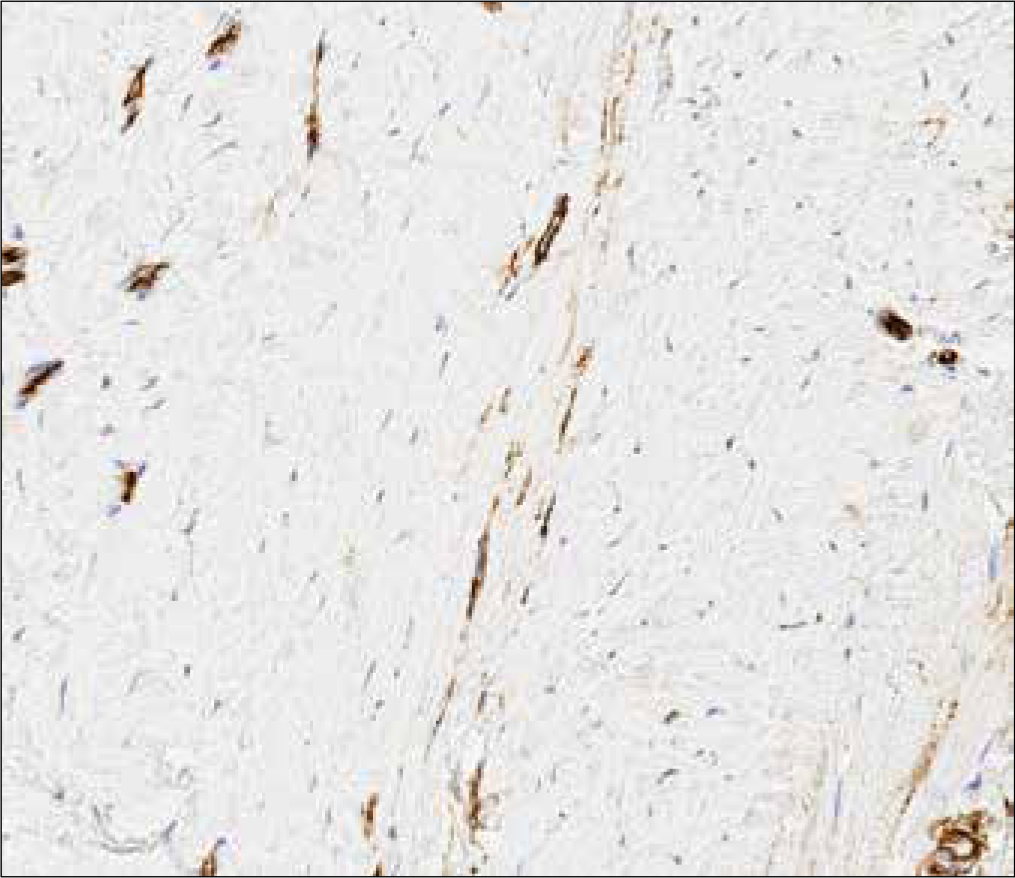
- Spindle elements faintly positive for CD34 (CD34 staining, 600×)
- Spindle elements positive for smooth muscle actin (SMA staining, 600×)
- Orcein staining showing the absence of elastic fibres within the tumour (orcein staining, 100×)
Histopathological differential diagnoses included sclerotic dermatofibroma, tendon sheath fibroma, long-standing neurofibroma and sclerotic lipoma. The absence of conventional histological features of dermatofibroma together with the absence of CD68 expression ruled out the diagnosis of a sclerotic dermatofibroma. Similarly, the lack of mature adipocytes through the lesion led to the exclusion of a sclerotic lipoma. The superficial location of the lesion and the absence of contiguity with the tendon were inconsistent with the diagnosis of a tendon sheath fibroma.
Finally, neurofibroma was excluded due to S100 negativity.
The immunohistochemical and morphological features were consistent with a lesion composed of sclerotic collagen bundles with scattered fibroblast expressing smooth muscle actin, factor XIII (and CD34 with lower intensity). Therefore, ruling out the other entities, a diagnosis of the solitary sclerotic fibroma (storiform collagenoma) was made.
The patient was referred to plastic surgery for wide excision of the lesion.
Sclerotic fibroma (SF), also known as storiform collagenoma, is a rare benign cutaneous tumour of mesenchymal origin. It was first described as a hallmark of PTEN hamartoma syndrome,2 but isolated, non-syndromic cases have been also reported.1 Histopathological features are represented by hyalinized collagen bundles arranged in a “plywood-like” or whorled pattern separated by a cleft and the presence of dilated blood vessels at the periphery of the lesion.3
Clinical presentation is heterogeneous: multiple SF represents a hallmark of PTEN hamartoma tumour syndrome – an inherited cancer predisposition syndrome due to PTEN mutations characterized by multiple cutaneous hamartomas and an increased risk of solid organ malignancies, mainly involving head and neck region.2 In its solitary form, sclerotic fibroma usually presents as a pink or flesh-coloured dome-shaped, firm nodule, with no sex predilection and different anatomical regions affected, including uncommon locations such as mucosae, acral sites and nail bed.1 Dermoscopically, solitary sclerotic fibroma has been shown to present a homogeneous whitish background and arborizing vessels.4 A literature search showed two other cases of recurrent solitary sclerotic fibromas: the first by McCalmont5 in a 46-year-old man who had a recurrence of the neoplasm on the left cheek, 30 months after local excision, and the second by Cohen et al.6 in a 20-year-old woman, seven years after a shave biopsy for a lesion located on the nose. In our case, though histopathological evidence was lacking to conclusively diagnose the initial lesion as sclerotic fibroma, history was consistent with the excision of a similar lesion.
Differently from the previous reports, in our patient the tumour did not affect the head and neck region—as it was unusually located on the foot, recurred after 5 years despite a local excision, and grew considerably reaching 4 cm in diameter.
Whether SF represents a reaction pattern, an end stage of a pre-existing fibrohistiocytic tumour (e.g. dermatofibroma) or an actively growing neoplasm was a matter of debate.1 However, the presence of actively collagen-producing spindle cells and the evidence of a type I procollagen synthesis,3 together with the recurrence potential of SF favour the primary neoplasm hypothesis.
Our report, adding probably a new recurrent SF case in the literature enlightens its potential to re-occur if not completely excised, and strengthens the hypothesis that it is a primary actively growing tumour.
Solitary sclerotic fibroma, although rare, requires a thorough clinical examination to exclude PTEN hamartoma syndrome. A complete local excision should be considered to minimize the possibility of a recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Circumscribed storiform collagenoma, an unusual tumor. Dermatol Online J. 2020;26:13030/qt3cm905c1.
- [PubMed] [Google Scholar]
- Multiple sclerotic fibromas of the skin: An important clue for the diagnosis of Cowden syndrome. BMJ Case Rep. 2017;2017:bcr2017221695.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Solitary sclerotic fibroma of the skin: Morphological characterization of the ‘plywood-like pattern’. J Cutan Pathol. 2008;35 Suppl 1:74-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of a solitary storiform collagenoma. Dermatol Pract Concept. 2018;8:120-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sclerotic fibroma: A fossil no longer. J Cutan Pathol. 1994;21:82-5.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent sclerotic fibroma of the skin. Am J Dermatopathol. 1999;21:571-4.
- [CrossRef] [PubMed] [Google Scholar]






