Translate this page into:
Red nodule on the face of a middle-aged woman
Corresponding author: Dr. Guangwen Yin, Department of Dermatology, The First Affiliated Hospital of Zhengzhou University in China, Zhengzhou, China. gwyin67@126.com
-
Received: ,
Accepted: ,
How to cite this article: Ma M, Gu S, Fang J, Yin G. Red nodule on the face of a middle-aged woman. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1608_2024
A 45-year-old woman presented with a red nodule on the right side of her nasal root for 10 days. On examination, we observed a solitary red nodule measuring 2×1×0.3 cm with well-defined margins, firm consistency, without signs of rupture or exudation [Figure 1]. The histopatholgy and immunohistochemistry findings are given in Figure 2a-c and Figure 3a-d.
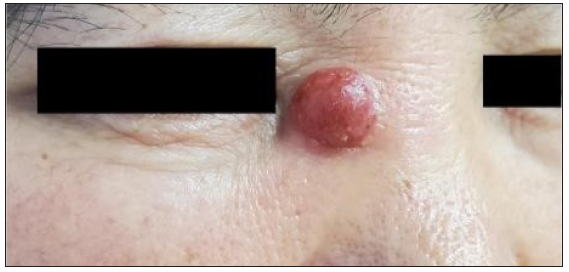
- A solitary, soybean-sized, red nodule to the patient’s right nostril, with clear borders and no signs of rupture or exudation.
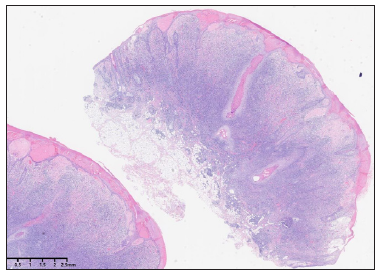
- Histopathological image showing tumour cells diffusely infiltrating the dermis and subcutaneous adipose tissue in focal areas. There is hyperkeratosis of the epidermis. Tumour cells are more densely distributed around the hair follicle appendages and in the reticular layer of the dermis. Destruction of the hair follicle appendage structure can be seen in focal areas, (Haematoxylin and eosin, 10x).
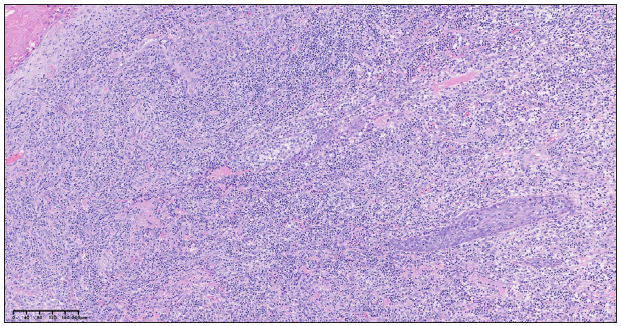
- Small to medium-sized lymphocytes infiltrating the superficial dermis. Focal liquefactive degeneration of the basal layer of the epidermis is evident, as is infiltration of tumour cells (Haematoxylin and eosin, 100x).
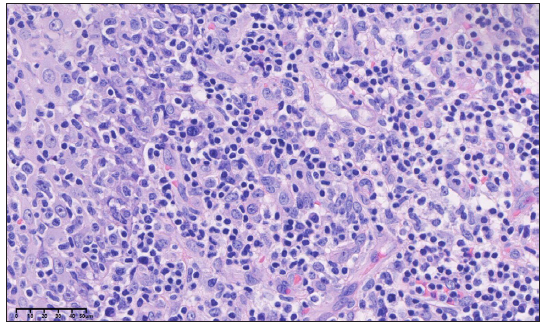
- Small to medium-sized tumour cells with slightly hyperchromatic nuclei. Some nuclei are irregularly shaped, and occasional mitotic figures are evident (red arrow). There are a small number of plasma cells and activated immunoblasts mixed within. Blood vessel endothelial cells are hyperplastic and plump (Haematoxylin and eosin, 400x).
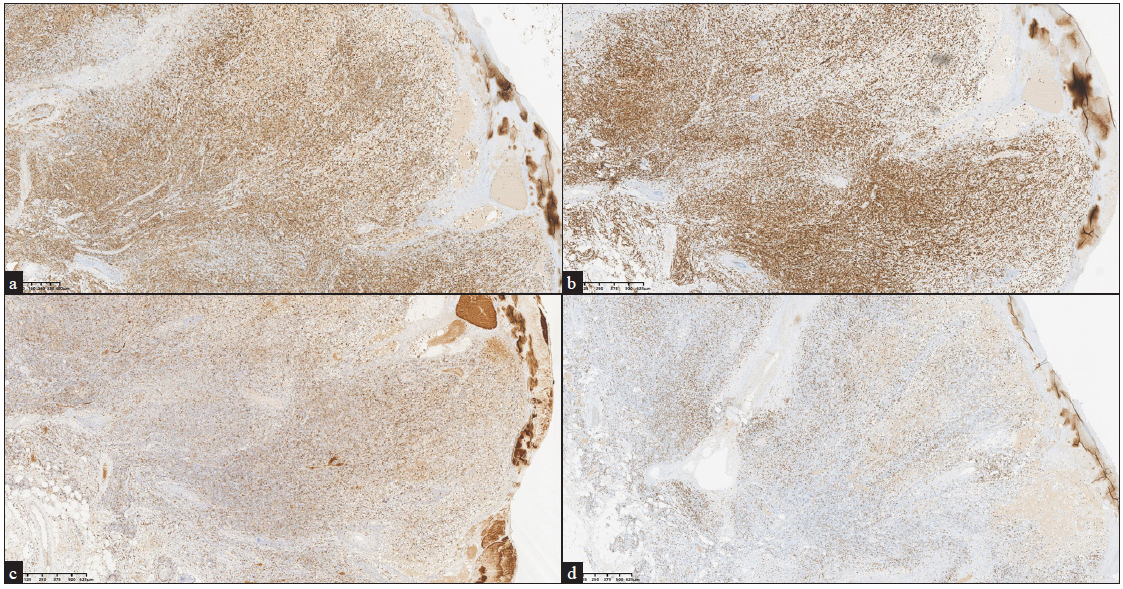
- Immunohistochemistry (IHC) images showing (a) CD4 positivity (40x), (b) CD3 positivity (40x), (c) PD-1 positivity (40x) and (d) weak CD8 positivity (40x)
Question
What is the diagnosis?
Answer
Diagnosis: Primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder
Discussion
Histopathological examination revealed epidermal hyperkeratosis [Figure 2a] and focal liquefactive degeneration of the basal layer. Dermal infiltrate comprised of small to medium-sized lymphocytes, with some migration towards the follicular epithelium [Figure 2b]. The nuclei of lymphocytes were slightly hyperchromatic, and some were even irregularly shaped [Figure 2c]. Immunohistochemical staining was positive for CD4 [Figure 3a], CD3 [Figure 3b], CD5, PD-1 [Figure 3c], and cytokeratin (CK), with weak positivity for CD8 [Figure 3d]. CD30, CD68, and MUM-1 were focally positive, while CD10, CD20, CD21, CD79α, and CXCL-13 were negative. The Ki67 proliferation index was 20% positive. Primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder (CD4+ PCSM-TCLD) is a rare benign lymphoproliferative disease with an estimated annual incidence of < 2 per 10 million. In 2008, the World Health Organisation (WHO) named this disease primary cutaneous CD4+ small/medium T-cell lymphoma based on characteristics such as cell morphology and the immunophenotype of the disease.1 In 2016, due to its indolent course and favourable prognosis the WHO changed the name to primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder (CD4+ PCSM-TCLD) 2. CD4+ PCSM-TCLD occurs in the face, neck, and upper limbs and often presents as a single nodule or plaque without subjective symptoms.
Histopathology and immunohistochemistry examination are gold standards for the diagnosis of CD4+ PCSM-TCLD. The characteristic histologic manifestation is dense, nodular, or diffuse lymphocytic infiltration of the dermis; however, no apparent epidermotropism or folliculotropism is observed. Immunohistochemistry often reveals CD4+, CD3+, CD8-, and CD30- markers. Atypical CD4+ T cells can also express follicular helper T cell markers such as PD1, BCL6, and CXCL13. In CD4+ PCSM-TCLD, the Ki-67 proliferation index of most patients is at a relatively low level (≤5–30%).3 Notably, the immunohistochemistry results in this case included weakly positive detection of CK. CK is a marker of epithelial cells and can be used to distinguish epithelial from non-epithelial tumours. However, a few cases of CK expression in non-epithelial tumours may be positive. This indicates that the origin of a tumour cannot be definitively determined based on CK expression alone. A comprehensive judgment based on clinical manifestations, histopathology, immunohistochemistry results, and other factors is necessary.
The following differential diagnosis may be considered- (1) T-cell pseudolymphoma—The lesions of CD4+ PCSM-TCLD have difficulty in spontaneous remission. Abnormal loss of T-cell antigens is common, and monoclonal T Cell Receptor (TCR) rearrangement can contribute to differentiation; (2) primary cutaneous follicular helper T-cell lymphoma—there are generally multiple skin lesions. Some patients have abnormal blood cell and Lactate Dehydrogenase (LDH) levels. They can express CD10 and require systemic treatment; and (3) mycosis fungoides, which has three stages of manifestations. Epidermotropism can be observed in histopathology.3
The treatment regimens for CD4+ PCSM-TCLD include surgical resection, radiotherapy, and local injection of steroids. Low-dose radiotherapy (4 Gy in two fractions) is preferred for isolated lesions.4 Additionally, some drugs can be used to treat CD4+ PCSM-TCLD, such as methotrexate, doxycycline, and BRAF inhibitors. Furthermore, it has been reported that the following situations often indicate a poor prognosis: (1) Rapid tumour progression and relatively large tumour size (diameter ≥ 5 cm); (2) A high tumour proliferation index (Ki-67); (3) A small number of infiltrating B cells and CD8+ T lymphocytes, as well as low CD4 expression; and (4) Central nervous system involvement.5 In this case, the patient underwent resection of skeletal muscle soft tissue tumour and random flap plasty. No signs of recurrence were observed after one year of follow-up.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Henan Zhongyuan Talents Program (Yucai Series)
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Reference
- The 2008 WHO classification of lymphoid neoplasms and beyond: Evolving concepts and practical applications. Blood. 2011;117:5019-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The 2016 revision of the world health organization classification of lymphoid neoplasms. Blood. 2016;127:2375-90.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary cutaneous CD4+ small/medium t-cell lymphoproliferative disorder-clinical and histopathologic features, differential diagnosis, and treatment. Semin Cutan Med Surg. 2018;37:39-48.
- [CrossRef] [PubMed] [Google Scholar]
- Excellent treatment outcomes from low dose radiation therapy for primary cutaneous CD4+ small/medium t-cell lymphoproliferative disorder. Radiother Oncol. 2023;178:109430.
- [CrossRef] [PubMed] [Google Scholar]
- Primary cutaneous small/medium CD4+ t-cell lymphomas: A heterogeneous group of tumors with different clinicopathologic features and outcome. J Clin Oncol. 2008;26:3364-71.
- [CrossRef] [PubMed] [Google Scholar]





