Translate this page into:
Relevance of patch testing in patients with nummular dermatitis
Correspondence Address:
D S Krupa Shankar
Department of Dermatology, Manipal Hospital, 98 Rustom Bagh, Airport Road, Bangalore - 560 017, Karnataka
India
| How to cite this article: Krupa Shankar D S, Shrestha S. Relevance of patch testing in patients with nummular dermatitis. Indian J Dermatol Venereol Leprol 2005;71:406-408 |
Abstract
Background: A chronic dermatosis like nummular dermatitis may be complicated by contact dermatitis due to an impaired cutaneous barrier. This study is aimed at evaluating secondary contact dermatitis in patients with nummular dermatitis. Methods: Patch testing with the Indian Standard Series was performed in 50 of 78 patients with a clinical diagnosis of nummular eczema. Significant reactions were graded as per ICDRG criteria. Results: Significant reactions were noted in 23 of 50 tested patients. The most frequent sensitizers were colophony, nitrofurazone, neomycin sulfate and nickel sulfate (7.14% each) Reactions to antigens in topical medications, cosmetics and toiletries constituted 64.28% of all the reactions. Conclusions: Patients with nummular dermatitis are at significant risk of developing secondary allergic contact dermatitis, which contributes to the severity and chronicity of their dermatitis. Patch testing has the potential to improve the quality of life in these patients. Hence, patients with chronic recalcitrant nummular dermatitis must be patch tested.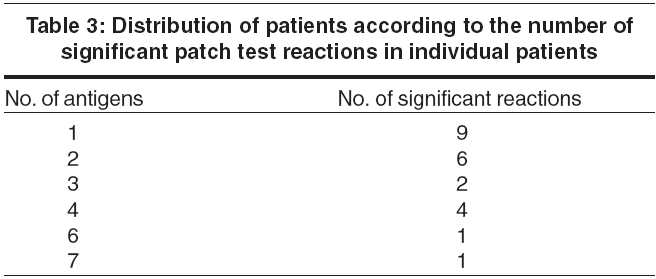
Introduction
Nummular dermatitis, also known as discoid eczema, is a common type of endogenous eczema. It was first described by Rayer in 1845 but the term was introduced by Devergie in 1857.[1] It is characterized by coin shaped or oval plaques with a clearly defined border. The etiology is obscure and a number of factors have been proposed as causative agents. Contact sensitivity to a number of substances is one of the etiological factors.[1] This study aims at finding the incidence of allergic contact dermatitis in patients with nummular eczema.
Methods
Seventy-eight patients with the clinical diagnosis of nummular dermatitis were included in the study, which was conducted from January 2003 to March 2004. Fifty of these patients were patch tested with the Indian Standard Series consisting of 29 antigens.[2] The criteria for patch testing were unremitting nummular dermatitis, anatomical distribution suggestive of allergic contact dermatitis, steadily shorter remissions, or nummular dermatitis worsened by topical treatment. Exclusion criteria for patch testing were extensive intervening areas of erythema, and pregnancy.
Readings were taken on Day 2 (48 hr) and Day 4 (96 hr) and interpreted according to ICDRG criteria.[3] Reactions on Day 4 were taken as significant. The relevance of positive reactions was explained to patients as being relevant to the present dermatitis, due to past exposure, or as significant reactions yet to prove their relevance and a source of caution against future exposure.
Results
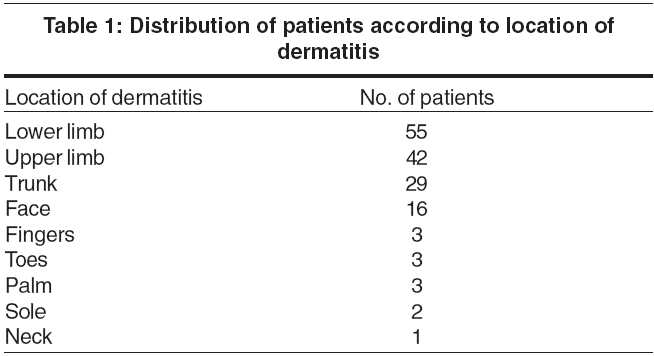
Of the 78 patients who participated in the study, 39 each were male and female. The youngest patient was 2 years old and the oldest was aged 84 years (mean age, 38.04 years). Most patients were in the age group of 21-50 years. Dermatitis was present in almost all the sites, with the lower and upper limbs being the commonest affected sites [Table - 1]. Forty-five patients had involvement of more than one site while 31 patients had only one site involved.
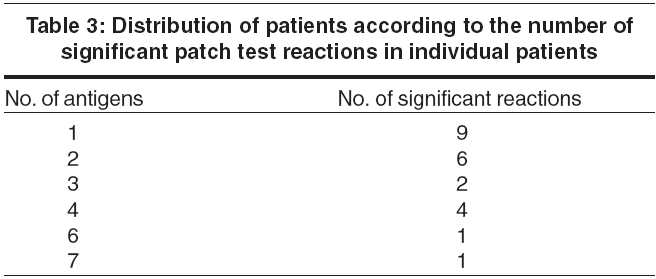
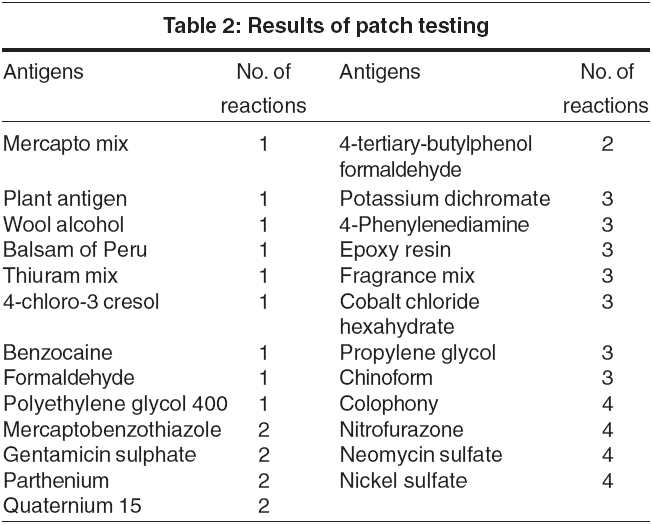
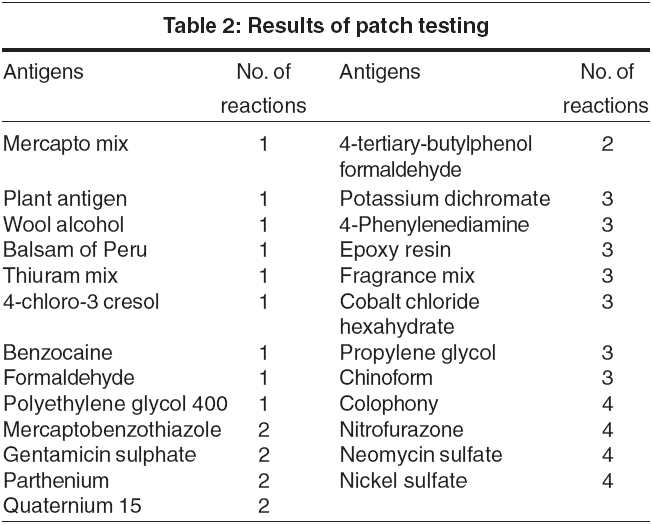
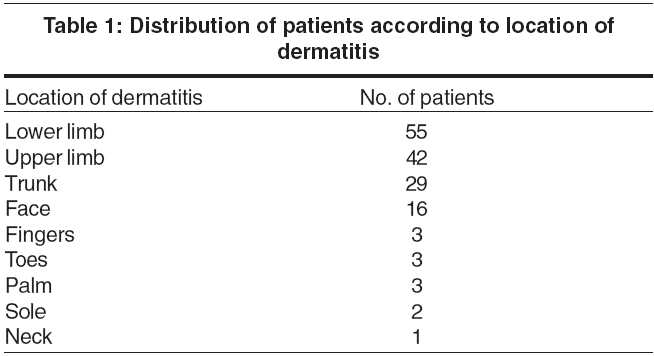
Of the 50 patients who were patch tested, a reaction was seen in 23 patients. In all, 56 reactions were seen, the most common allergens being nickel sulfate, neomycin, nitrofurazone and colophony [Table - 2]. Nine patients reacted to one antigen while 14 patients reacted to more than one [Table - 3]. Reactions to topical medications, cosmetics and toiletries constituted about 64% of the reactions (cosmetic antigens, 17.85%; toiletry antigens; 10.7%; and topical medications, 35.7%).
Discussion
Allergic contact dermatitis has been found to be very common in nummular dermatitis.[14] Oral challenge with metal salts is known to aggravate various types of eczema, including nummular eczema.[4] Ethyl cyanoacrylate-containing glue, as well as ethylenediamine hydrochloride, have been reported to cause a nummular eczema-like eruption.[5],[6] In atopic children, thiomerosal is known to cause nummular eczema.[7] Mercury leaching out of dental amalgams,[8],[9] and depilating creams containing potassium thioglycolate[10] can cause nummular eczema. Hypersensitivity to aloe can also manifest as eczematous lesions of nummular eczema.[11] Xerotic skin permits various aeroallergens to enter and induce nummular eczema.[12]
Shenoi et al found that the common sensitizers in patients with allergic contact dermatitis were gentamicin, potassium dichromate, colophony and fragrance.[13] In a study by Fleming et al, 50% of 48 patients with nummular dermatitis showed positive patch test reactions and 33% of these were considered clinically relevant. The commonest allergens were rubber chemicals, formaldehyde, neomycin, chrome and nickel.[14] Khurana et al found that 50% of 56 patients with nummular dermatitis showed positive reactions on patch testing, the commonest allergens being potassium dichromate, nickel, cobalt chloride and fragrance mix in decreasing order.[15] In our study, two-thirds of patients with nummular dermatitis required patch testing and about half of them showed significant reactions. Two-thirds of these reactions were to antigens in cosmetics, toiletries and medications that would remain in prolonged contact with the skin. The antigens include the following:
l Wool alcohol found in cosmetics, moisturizers
l Balsam of Peru used as fixative and fragrance in perfume, topical medications
l 4-chloro- 3 cresol found in creams, topical antiseptics, shampoos
l Benzocaine, a local anaesthetic which cross reacts with parabens
l Formaldehyde used as a preservative in cosmetics, shampoos, etc.
l Polyethylene glycol 400 found in cosmetics, topical medicaments, detergents, toothpaste, etc.
l Gentamycin sulphate, a medicine
l 4-paraphenylenediamine found in hair dyes which cross react with parabens
l Fragrance mix found in cosmetics, toothpaste, soap, etc.
l Chinoform commonly found in topical pharmaceutical preparations
l Colophony found in transparent soaps and cosmetics
l Nitrofurazone, a topical antibiotic which indicates past exposure
l Neomycin sulphate, a broad spectrum antibiotic in topical creams, powders, ointment, eye & ear drops
l Quaternium 15, a preservative in many cosmetics, topical medicines
l Propylene glycol, used in therapeutics (topical steroids, antibiotic preparations, lubricant jelly, ECG gels, injectables) and cosmetics
Patients with nummular dermatitis are at increased risk of developing secondary contact dermatitis due to impaired barrier function that contributes to the chronicity and severity of dermatitis. Patch testing has the potential to increase the quality of life in these patients. Therefore, it is recommended that patients with chronic, recalcitrant nummular dermatitis be patch tested.
| 1. |
Soter NA. Nummular eczema and lichen simplex chronicus/prurigo nodularis. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's Dermatology in general medicine. 6th ed. New York: Mc Graw-Hill; 2003. p. 1194-6.
[Google Scholar]
|
| 2. |
Narendra G, Srinivas CR. Patch testing with Indian Standard Series. Indian J Dermatol Venereol Leprol 2002;68:281-2.
[Google Scholar]
|
| 3. |
Wilkinson JD, Shaw S. Contact Dermatitis: Allergic. In : Burns Tony, Breathnach Stephen, Cox Neil, Griffiths Christopher, editors. Rook's Textbook of dermatology. 7th ed. Oxford: Blackwell; 2004. p. 20.
[Google Scholar]
|
| 4. |
Veien NK, Hattel T, Justesen O, Norholm A. Oral challenge with metal salts. (II). Various types of eczema. Cont Dermat 1983;9:407-10.
[Google Scholar]
|
| 5. |
Belsito DV. Contact Dermatitis to ethyl-cyanoacrylate containing glue. Cont Dermat 1987;17:234-6.
[Google Scholar]
|
| 6. |
Caraffini S, Lisi P. Nummular dermatitis-like eruption from ethylenediamine hydrochloride in 2 children. Cont Dermat 1987;17:313-4.
[Google Scholar]
|
| 7. |
Patrizi A, Rizzoli L, Vincenzi C, Trevisi P, Tosti A. Sensitization to thiomerosal in atopic children. Cont Dermat 1999;40:94-7.
[Google Scholar]
|
| 8. |
Pigatto PD, Guzzi G, Persichini P. Nummular lichenoid dermatitis from mercury dental amalgam. Cont Dermat 2002;46:355-6.
[Google Scholar]
|
| 9. |
Adachi A, Horikawa T, Takashima T, Ichihashi M. Mercury-induced nummular dermatitis. J Am Acad Dermatol 2000;43:383-5.
[Google Scholar]
|
| 10. |
Le Coz CJ. Contact nummular (discoid) eczema from depilating cream. Cont Dermat 2002;46:111-2.
[Google Scholar]
|
| 11. |
Morrow DM, Rapaport MJ, Strick RA. Hypersensitivity to aloe. Arch Dermatol 1980;116:1064-5.
[Google Scholar]
|
| 12. |
Aoyama H, Tanaka M, Hara M, Tabata N, Tagami H. Nummular eczema: An addition of senile xerosis and unique cutaneous reactivities to environmental aeroallergens. Dermatology 1999;199:135-9.
[Google Scholar]
|
| 13. |
Shenoi DS, Srinivas CR, Balachandran C. Results of patch testing with a standard series of allergens at Manipal. Indian J Dermatol Venereol Leprol 1994;60:133-5.
[Google Scholar]
|
| 14. |
Fleming C, Parry E, Forsyth A, Kemmett D. Patch testing in discoid eczema. Cont Dermat 1997;36:261-4.
[Google Scholar]
|
| 15. |
Khurana S, Jain VK, Aggarwal K, Gupta S. Patch testing in discoid eczema. J Dermatol 2002;29:763-7.
[Google Scholar]
|
Fulltext Views
3,040
PDF downloads
1,537





