Translate this page into:
Response to topical halcinonide following fractional carbon dioxide laser pretreatment in a pretibial myxedema patient
2 Department of Endocrinology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
Correspondence Address:
Xuqin Zheng
Department of Endocrinology, The First Affiliated Hospital of Nanjing Medical University, Nanjing 210029
China
| How to cite this article: Xu Y, Ma R, Cai Y, Zheng X. Response to topical halcinonide following fractional carbon dioxide laser pretreatment in a pretibial myxedema patient. Indian J Dermatol Venereol Leprol 2018;84:763 |
Sir,
Pretibial myxedema is a characteristic manifestation of Graves' disease. The treatment of pretibial myxedema remains challenging. Here, we report the response to topical 0.025% halcinonide solution in combination with pretreatment with fractional carbon dioxide laser in a patient with pretibial myxedema.
A 73-year-old male Chinese patient was referred to our department for refractory localized pretibial myxedema on both feet. The patient was diagnosed with Graves' disease 11 years ago and radioactive iodine ((131) I) was used 10 years ago. Four years before this presentation, he was diagnosed with hypothyroidism and prescribed levothyroxine sodium tablets for daily use. During the past year, pretibial myxedema developed gradually on both pretibia and feet, making it difficult for him to wear shoes and walk. Before our therapy, laboratory tests revealed that the level of thyroid function was in the normal range and the level of thyroid-stimulating hormone receptor antibody was very high (thyroid-stimulating hormone receptor antibody >40 IU/L). Subcutaneous injection of methylprednisolone every month resulted in improvements in the pretibial region after three treatments, but injection into the skin of the feet was difficult due to the obvious hyperplasia. Daily topical application of 0.025% halcinonide solution and wrapping with plastic film for 2 h for 1 month yielded no obvious improvement.
Therefore, we employed a fractional carbon dioxide laser to enhance the topical absorption of steroids. The patient's feet were divided into four parts as shown in [Figure - 1]. Half of the right foot (area A) served as the control without any treatment. The other half of the right foot (area B) was treated with fractional carbon dioxide laser only. Half of the left foot (area C) was treated with a topical 0.025% halcinonide solution once a day while the other half of the left foot (area D) was treated with a fractional carbon dioxide laser every 2 weeks and 0.025% halcinonide solution once a day.
 |
| Figure 1: Clinical therapeutic protocol for this case. The patient's two feet were divided into four parts. Half of the right foot (area A) served as the negative control and did not receive any treatment; the other side of the right foot (area B) was treated with fractional carbon dioxide laser only. Half of the left foot (area C) was treated with topical 0.025% halcinonide solution once a day, while the other half of the left foot (area D) was treated with fractional carbon dioxide laser every 2 weeks in addition to the daily topical application of 0.025% halcinonide solution |
For area B and D, the skin was irradiated with a fractional carbon dioxide laser (AcuPulse®, Lumenis Ltd., Santa Clara, CA, USA) with fluences ranging from 20 to 30 mJ/cm2, the same spot density (10%) and no overlapping of spots during therapy. The variations in fluence were dependent on the thickness of the skin with thicker skin requiring higher fluence until the patient felt slight pain.
After a 6-week period of three treatments, the skin of area D showed obvious improvement compared to the other areas. Area D exhibited thinned skin, finer skin texture and fewer nodules and the boundary between area C and area D was very clear [Figure - 2]a. Dermoscopy (DermLite® DL1, 3Gen Inc., San Juan Capistrano, CA, USA) revealed more scales and white clods on a pink background on the skin of area C [Figure - 2]b which correspond to hyperkeratosis at the periphery of the papules and papillary dermal deposition of mucin, respectively, while more pink background with less scales and white clods were observed on the skin of area D [Figure - 2]c.[1]
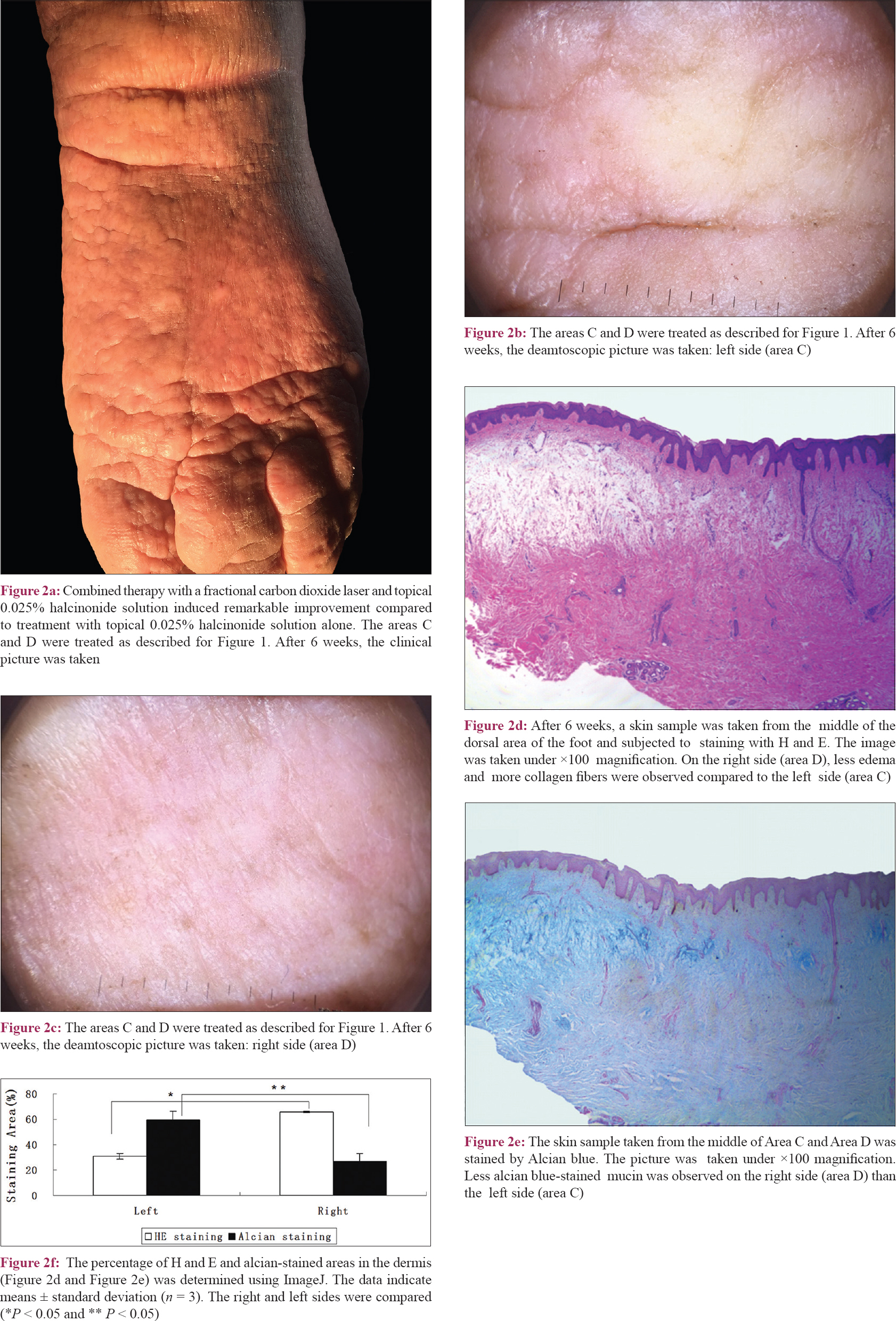 |
| Figure 2: |
Histological results confirmed these observations [Figure - 2]d, [Figure - 2]e, [Figure - 2]f. On the right side (area D), less edema, less alcian blue-stained mucin and more collagen fibers were observed compared to the left side (area C), demonstrating improvement of pretibial myxedema. These observations were further confirmed by quantitative assessment of the percentage of collagen density (the pink-purple-stained area in [Figure - 2]d; area C: 30.9% ±2.5% vs. area D: 65.9% ± 0.4%, *P = 0.0008) and mucin deposition (the dark blue-stained area in [Figure - 2]e; area C: 59.2% ±7.0% vs. area D: 26.9% ± 6.4%, **P = 0.023) using ImageJ software (http://rsbweb.nih.gov/ij/).
During the following 22 weeks, all four areas were treated with the combined therapy protocol as area D. The fluences of laser were gradually decreased to 12.5–15 mJ/cm2 to avoid pain. After a total of 28 weeks, the thickness and roughness of the skin were improved and specifically, the nodules and plaques around the ankles diminished [Figure - 3]a and [Figure - 3]b. The patient was more comfortable wearing shoes and walking, and he refused further treatment.
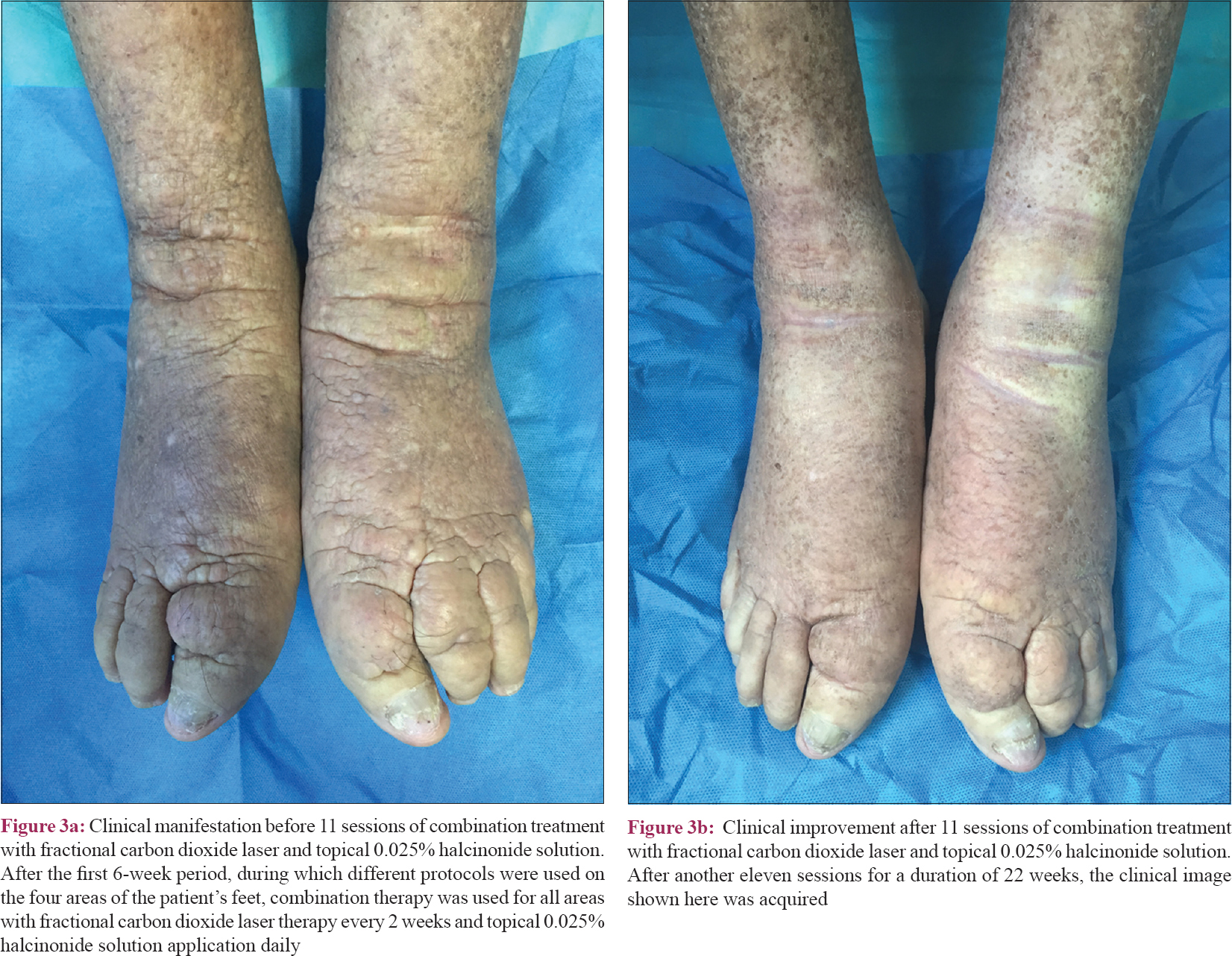 |
| Figure 3: |
Besides systemic management of Graves' disease, the most widely used treatments for pretibial myxedema are glucocorticoids. Topical glucocorticoids were reported to be useful in some cases but did not work in our patient.[2] Moreover, subcutaneous injection of steroids was too difficult due to the obvious hyperplasia. Hence, we chose fractional carbon dioxide laser to enhance transdermal delivery which had been reported to be effective in enhancing absorption of lots of topical substances including glucocorticoids.[3] As expected, the combined therapy was revealed as a promising treatment modality for pretibial myxedema. However, randomized, blinded, controlled clinical studies with more samples and a longer follow-up period are needed for further confirmation.
Financial support and sponsorship
This study was supported by the Chinese National Natural Science Foundation (81301384), Jiangsu Province Natural Science Foundation (BK20131029) and the Priority Academic Program Development of Jiangsu Higher Education Institutions (No. JX10231801).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Rojanametin K, Masaru T. Dermoscopy of pretibial myxedema. J Am Acad Dermatol 2015;73:e195-6.
[Google Scholar]
|
| 2. |
Kriss JP, Pleshakov V, Rosenblum A, Sharp G. Therapy with occlusive dressings of pretibial myxedema with fluocinolone acetonide. J Clin Endocrinol Metab 1967;27:595-604.
[Google Scholar]
|
| 3. |
Yu J, Bachhav YG, Summer S, Heinrich A, Bragagna T, Böhler C, et al. Using controlled laser-microporation to increase transdermal delivery of prednisone. J Control Release 2010;148:e71-3.
[Google Scholar]
|
Fulltext Views
2,446
PDF downloads
2,464





