Translate this page into:
Retrospective analysis of ultrathin skin grafting over carbon dioxide ablated lesions supplemented with excimer lamp (308 nm) therapy in stable vitiligo
Corresponding author: Dr Sushil S Savant Jr, Department of Dermatology, The Humanitarian Clinic: Skin, Hair and Laser Centre, Mumbai, Maharashtra, India. sushilsavant786@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Savant SS Jr, Savant SS. Retrospective analysis of ultrathin skin grafting over carbon dioxide ablated lesions supplemented with excimer lamp (308 nm) therapy in stable vitiligo. Indian J Dermatol Venereol Leprol. 2024;90:150–7. doi: 10.25259/IJDVL_408_2022
Abstract
Background
Of all the tissue or cellular grafting techniques used in the treatment of vitiligo, melanocyte transplant/transfer through ultrathin skin grafting (UTSG) provides rapid onset of regimentation. The regimentation process is further accelerated with a combination of psoralen and ultraviolet A radiation, or psoralen and ultraviolet A obtained by sunlight or narrowband ultraviolet light B, or excimer laser/lamp (308 nm).
Aims
We assessed the efficacy of carbon dioxide laser ablation followed by melanocyte transplant/transfer through ultrathin skin graft sheet/sheets and further treated by excimer lamp therapy in patients with stable vitiligo.
Methods
One hundred ninety-two patients with stable vitiligo were treated with UTSG following carbon dioxide laser ablation and patients were then put on excimer lamp therapy. Primary efficacy was determined in terms of grades of regimentation and colour match at the end of 1-year.
Results
A total of 192 stable vitiligo patients with a mean age of 32.71 ± 8.55 years were recruited. Of the total 410 lesions, 394 showed excellent regimentation indicating a success rate of 96.1% at 1-year follow-up, whereas 16 (3.9%) lesions present on fingertips and toe tips showed poor or no regimentation at 3-month and 1-year follow-up. With regards to colour match, 394 (96.1%) lesions had achieved excellent colour match, and 16 lesions (3.9%) had poor or no colour match at 1-year follow-up.
Limitations
This was a single-center study with a small sample size.
Conclusion
The effectiveness of carbon dioxide laser ablation followed by melanocyte transfer/transplant through ultra-thin skin graft sheet/sheets when combined with excimer lamp therapy provides favourable cosmetic outcomes with rapid onset of regimentation in stable vitiligo.
Keywords
ultrathin skin grafting
stable vitiligo
excimer lamp
autologous melanocyte transplant
Plain Language Summary
Stable vitiligo can be treated surgically with various tissue or cellular grafting techniques, including ultrathin skin grafting (UTSG). Of all the tissue or cellular grafting techniques used in the treatment of vitiligo, melanocyte transplant/transfer through UTSG provides rapid onset of regimentation. The regimentation process is further accelerated with a combination of psoralen and ultraviolet A radiation, or psoralen and ultraviolet A obtained by sunlight or narrowband ultraviolet light B or excimer laser/lamp (308 nm). With this study, we concluded that autologous melanocyte transplant/transfer technique by UTSG following carbon dioxide laser ablation is one of the advanced techniques in the armamentarium of a dermatosurgeon. With this repigmentation technique, large stable vitiliginous areas can be covered completely in single or multiple sessions. Moreover, during the wound healing process, there is transplant/transfer of melanocytes which ultimately renders excellent cosmesis with an uniform textural and natural-looking colour match. The excimer light aids in faster, better cosmetic outcomes after surgery.
Introduction
Vitiligo is an acquired dyschromia characterised by depigmented or hypo-pigmented macules secondary to the partial or total destruction of melanocytes.1 In India, vitiligo is considered a social stigma and has significant psychological repercussions with cosmetic impairment and influences the quality of life.2 Vitiligo is classified as segmental, nonsegmental (focal, acro-facial, and vulgaris) and universal.3 Usually, vitiligo patients are treated with topical and/or systemic medical lines combined with phototherapy. Many cases of vitiligo are refractory to the medical line of treatment. Stable vitiligo is a term coined for such cases wherein the disease is inactive with no new patches or progression of pre-existing lesions and absence of Koebner’s phenomenon for the past 1 year.4 Stable vitiligo can be treated surgically with various tissue or cellular grafting techniques, including ultrathin skin grafting (UTSG).5–15
In UTSG, ultrathin split-thickness skin graft containing epidermis and the uppermost part of the superficial papillary dermis is harvested either with Silver’s knife or power dermatome. It is then grafted over dermabraded or carbon dioxide laser-ablated vitiliginous lesion and secured either with surgical glue (N-butyl-2-cyanoacrylate) (Adhist and Braun) or pressure dressing to achieve repigmentation through melanocyte transplant/transfer.5,9,10,16–21 The ultrathin skin graft (0.005 inch/0.1 mm) either dries off or is peeled off, or if thick (>0.005 inch/0.1 mm) gets taken up as split thickness skin graft.9,10,16–18 The thinner the grafts better are the results. Postoperatively, repigmentation process is accelerated with a combination of psoralen and ultraviolet A obtained by either radiation lights (PUVA)/sunlight (PUVA sol), or narrowband ultraviolet light B, or excimer laser/lamp (308 nm) to achieve a natural colour match, excellent cosmesis with minimal side effects and complications.5,10,20,21 In this study, we investigate the efficacy of carbon dioxide laser ablation followed by melanocyte transplant/transfer through ultrathin skin grafts (0.005 inch/0.1 mm), supplemented with excimer lamp 308 nm therapy in terms of acceptable cosmetic outcomes in stable vitiligo, which to the best of our knowledge has not yet been reported.
Methods
Study design
This was a retrospective, observational study that included 192 patients afflicted with stable vitiligo referred to the outpatient department of The Humanitarian Clinic: Skin, Hair and Laser Centre, Mumbai, India, from May 2017 to December 2018. Records of patients (age ≥18 years) with segmental, nonsegmental (focal, acral, and residual vulgaris) stable vitiligo for at least one year were analysed. As a protocol, patients with active vitiligo, universal vitiligo, keloidal tendency and pregnant or lactating patients were not studied. This study adhered to the principles outlined in the Declaration of Helsinki and was approved by the local Institutional Ethics Committee (Registration number: ISBEC/NR-23/KM-KM/2022).
Data collection
Information regarding demographic details, clinical characteristics, procedure performed and clinical outcome of the treatment were collected as per predefined proforma.
Technique
The approximate size (width and length) and the number of graft sheets/sheets from the donor area required as per the area of the recipient vitiliginous site (number, size, and shape) to be grafted were calculated. Recipient and donor (thigh-anterior/lateral aspect) areas were surgically prepared, after administering appropriate anaesthesia (general, regional, local, tumescent local and topical have all been used). Ultrathin skin grafts (0.005 inch/0.1 mm) of desired size were harvested in a conventional manner with a power dermatome-Zimmer (Intra Medical Systems Ltd., Mumbai, India) after adjusting its parameter (thickness and width) and stored in a sterile bowl containing normal cold saline. The wound was then dressed with topical antibiotics.
The border was marked on the surrounding normal skin/mucosa extending 2–3 mm beyond the vitiliginous recipient area all along its periphery. The focusing lens of carbon dioxide laser 10,600 nm (Laserbio Optotechl., Mumbai, India) was removed, and parameters were adjusted (power: 6 W for lip and 8–10 W for skin; spot size: 6 mm; mode: continuous wave-vaporising) and the entire marked area was ablated with bubbling effect using free hand technique from one pole to other in rapid, to and fro sweeping movements. The bubbled-out debris was wiped away, and the graft was evenly spread on the ablated area. Leaving a 3–5 mm margin beyond the ablated area, the graft was trimmed as per the shape and size of the recipient area and the edges were secured to the surrounding normal skin/mucosa with surgical glue. It was dressed with a double layer of framycetin or povidine iodine tulle and gauze. In case of oral mucosal involvement, the antibacterial ointment was applied over the grafted lip (lip vitiligo), and was left open without any dressing. The patient was advised to have oral fluids for 3–4 days. After dressing, fingertips, toe tips and joints were immobilised with splints for 10 days.
Postoperative treatment
Antibiotics, analgesics, and anti-inflammatory drugs were prescribed for 8–10 days. Both the dressings were removed after 10–12 days. The donor site healed completely with hyper/hypo pigmentation. The graft either dried or macerated (lip) or, if retained, was peeled off manually, leaving the recipient site erythematous with an achromic area and tiny islands of pigmentation (transferred/transplanted melanocytes). Excimer lamp therapy (Exciplex XeCl lamp 308 nm wavelength, monochromatic non-coherent, spot size 25 cm2, pulse duration 0.5–30 seconds, power density 100 W/cm2, Geomedics Pharma Ltd., India) was started biweekly on non-consecutive days after the erythema subsided (8–10 days). The initial doses administered in different body parts included - 50 mJ/cm2—lips, eyelids, face and neck; 100 mJ/cm2—limbs with hand and feet, trunk, fingertips and toe tips [Table 1]. The treatment for the lips and eyelids was maintained at the same dose throughout the treatment. The dose for face and neck was increased by 10 mJ/cm2 and by 20 mJ/cm2 for limbs with hand and feet, trunk, fingertips, and toe tips from the previous dose; every 4th week if there was no erythema noted or if the erythema noted did not persist after 24 hours [Table 1]. In case the erythema lasted for 48 hours, then the dose was not increased, and if the erythema lasted for >48 hours, the following session was skipped, and the next session was restarted with the initial dose. The maximum cumulative dose that reached fingertips and toe tips after 6 months was 40.8 J/cm2 when the treatment was terminated.
| Vitiligo site | Initial dose (mJ/cm2) | Increment in dose from previous dose (mJ/cm2) (every 4th week) based on posttreatment erythema | ||
|---|---|---|---|---|
| No erythema or erythema up to 24 hours | Erythema 24–48 hours | Erythema >48 hours | ||
| Lips and eyelids | 50 | The dose remained the same throughout the treatment | No change in the dose | Session skipped till erythema |
| Rest of face and neck | 50 | 10% | settled down and restarted | |
| Limbs with hand and feet, trunk, fingertips, and toe tips | 100 | 20% | from the initial first dose | |
Repigmentation and colour-matched grading
Skin regimentation was graded as follows: (1) G 0; absent, no response; (2) G І; <25%, poor response; (3) G II; 25–50%, moderate response; (4) G III; 50–75%, good response; and (5) G IV; >75%, excellent response.
Repigmented skin was colour matched with the normal surrounding skin and graded as “poor”, “moderate”, “good”, or “excellent”.
Follow-up
All observations were taken by a single dermatologist using clinical images and subjective assessment scores of repigmentation. Patients were evaluated at baseline and at 3, 6 months, and 1 year for grades of repigmentation and colour match. Adverse events, if any, to the treatment procedure were noted.
Statistical analysis
Quantitative data are presented as mean ± standard deviation, and qualitative data are reported as frequency and percentages. Data were statistically analysed using the Statistical Package for Social Sciences software, version 21.0 (IBM Corp., Armonk, New York, United States of America).
Results
Demographic characteristics of patients with stable vitiligo
A total of 192 stable vitiligo patients with 410 lesions were recruited. The mean age of the study sample was 32.71 ± 8.55 years (range: 18–35) with a female [119 (62%)] patients] predominance. The mean age of onset of the disease was 23.57 ± 6.69 years. Family history of vitiligo was reported in 58 (30.2%) patients, and 160 (83.3%) patients had a history of drug (psoralens, steroids topically and orally) given with phototherapy for 1 year to the stable lesion. Nonsegmental vitiligo (69.8%) was observed in the majority of the study population, of which more than half of the patients (61.5%) had focal vitiligo. Face and neck [164 (40%) patients] were the most frequently involved site, whereas acrofacial [four (4.9%) patients] involvement was less common [Table 2].
| Characteristics | Total patients (N = 192) |
|---|---|
| Age, mean ± standard deviation (range), years | 32.71 ± 8.55 (18–35) |
| Gender | |
| Females | 119 (62) |
| Males | 73 (38) |
| Age of onset, mean ± standard deviation, years | 23.57 ± 6.69 |
| Duration of disease (range), years | 9.13 ± 7.24 (5–12) |
| Family history, n (%) | 58 (30.2) |
| History of drug with phototherapy, n (%) | 160 (83.3) |
| No. of lesions, n (%) (n = 410) | |
| 1 | 78 (19) |
| 2 | 124 (30.2) |
| 3 | 108 (26.3) |
| 4 | 55 (13.4) |
| 5 | 25 (6.1) |
| 6 | 20 (4.9) |
| Types of vitiligo, n (%) | |
| Segmental | 58 (30.2) |
| Nonsegmental | 134 (69.8) |
| Focal (including lips) | 118 (61.4) |
| Acrofacial (including lips, fingertips and toe tips) | 4 (2.1) |
| Vulgaris (residual) | 12 (6.3) |
| Site of patches, n (%) (N = 410) | |
| Face and neck | 164 (40) |
| Trunk | 124 (30.2) |
| Limbs with hands and feet | 102 (24.9) |
| Acrofacial | 20 (4.9) |
| Lips | 4 (1) |
| Fingertips and toetips | 16 (3.9) |
Assessment of the treatment outcomes
Repigmentation grade, colour match and site response are outlined in [Table 3]. Out of 4,10,394 lesions present on lips and eyelid, the rest of the face and neck, trunk and limbs with hands and feet showed excellent repigmentation indicating a success rate of 96.1% at 1-year follow-up [Figures 1–3]. On the other hand, 16 (3.9%) lesions present on fingertips and toe tips showed poor or no repigmentation at 3-month and 1-year follow-up. A total of 394 (96.1%) patients lesions achieved excellent colour match, and 16 (3.9%) patients lesions had a poor colour match at 1-year follow-up. The number of bi-weekly sessions of excimer lamp therapy required as per site of involvement were as follows - lips and eyelids 6–8 (3–4 weeks), rest of face and neck 12–16 (6–8 weeks), trunk and limbs with hand and feet 24–32 (12–16 weeks), fingertips and toe tips 48 (24 weeks—after which it was terminated as they showed poor or no response).
| Outcome | Total lesions (N = 410) | ||
|---|---|---|---|
| At 3 months n (%) | At 6 months n (%) | At 1 year n (%) | |
| Repigmentation grade | |||
| Grade I (poor) | 20 (4.9) | 16 (3.9) S1 | 16 (3.9) S1 |
| Grade II (moderate) | – | – | – |
| Grade III (good) | 46 (11.2) | – | – |
| Grade IV (excellent) | 344 (83.9) | 394 (96.1) S2 | 394 (96.1) S2 |
| Colour match | |||
| Poor | 20 (4.9) | 16 (3.9) S1 | 16 (3.9) S1 |
| Moderate | – | – | – |
| Good | 46 (11.2) | – | – |
| Excellent | 344 (83.9) | 394 (96.1) S2 | 394 (96.1) S2 |
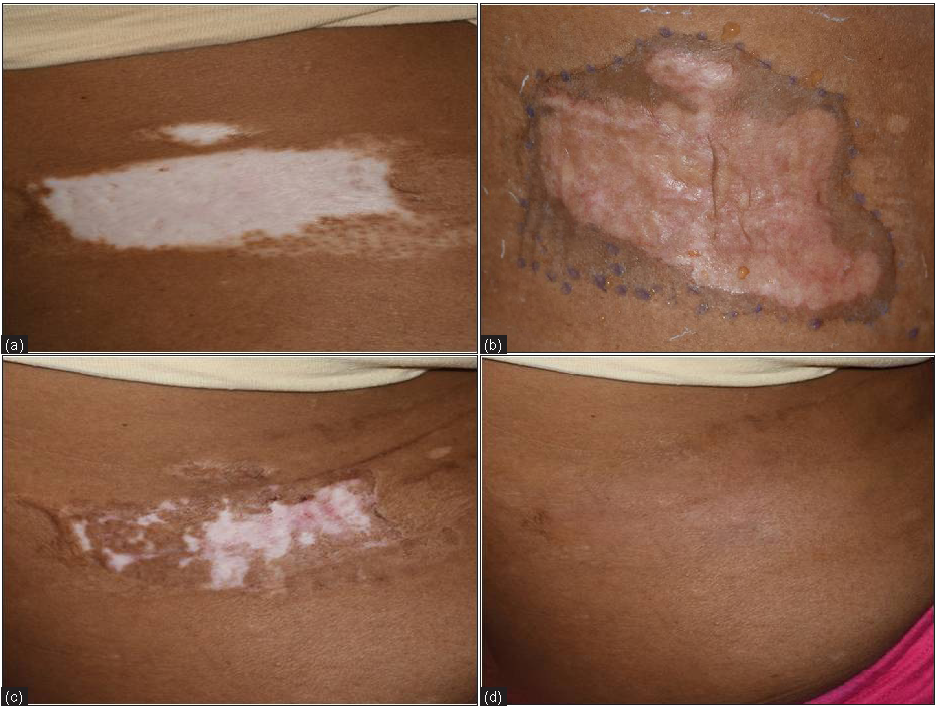
- (a) Ultrathin skin grafting (UTSG) non-segmental (focal) on lower back – before, (b) Fixation of graft with surgical glue, (c) Early spread of pigmentation after excimer lamp 308 nm therapy for 1 month, (d) Complete re-pigmentation after excimer lamp 308 nm therapy for 2 months

- (a) Segmental vitiligo on face -before ultrathin skin grafting, (b) fixation of graft with surgical glue, (c) drying of graft and crusting, (d) complete pigmentation after excimer lamp 308 nm therapy for 1½ months
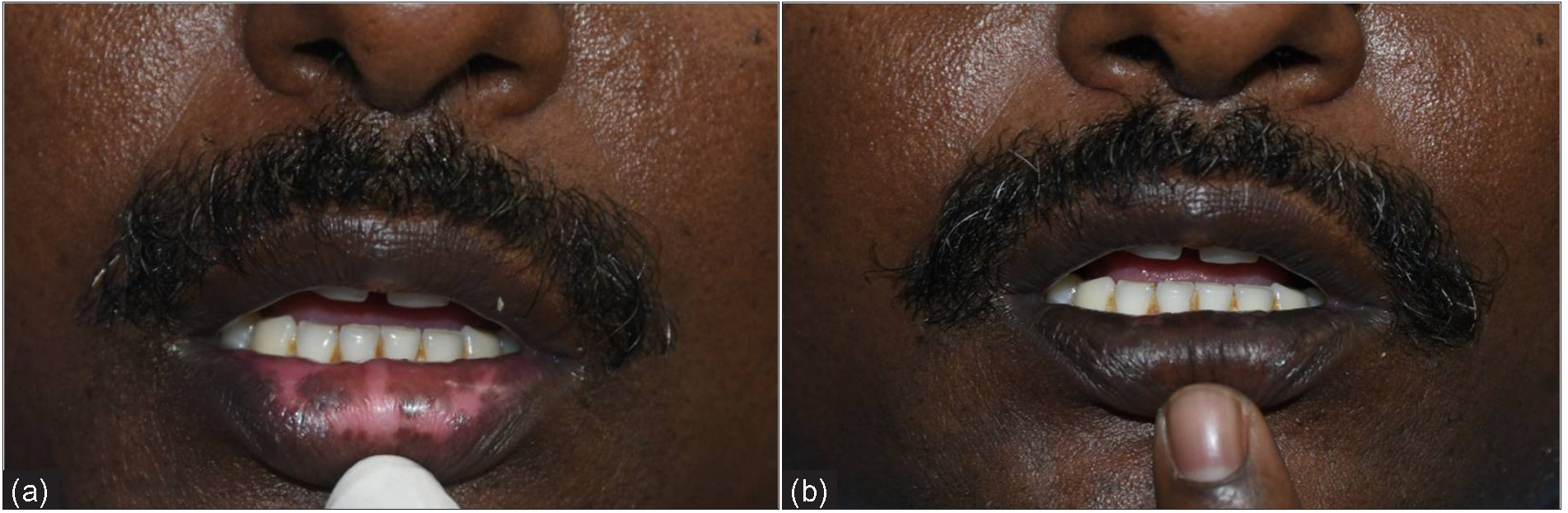
- (a) Non-segmental Acrofacial vitiligo involving the lower lips prior to ultrathin skin grafting before, (b) Complete repigmentation after excimer lamp 308 nm therapy for 1 month
Side effects/complications
Complications related to the surgical procedure were lack of pigment transfer, thick grafts, upside-down grafts, and graft displacement as detailed in [Table 4]. Complications of excimer lamp therapy included severe erythema over nonsegmental (focal vitiligo) lesions in two patients (after four sessions in one and after six sessions in another). Both these patients developed transient hyperpigmentation despite terminating the excimer lamp therapy, which subsided over the next 4–6 months with a good colour match. Two patients developed blisters (one with segmental vitiligo on the trunk, another with nonsegmental residual vulgaris on the arm) after 12 and 16 sessions, respectively. Excimer lamp therapy was withdrawn and they healed with transient hyperpigmentation, which eventually subsided over the next 4–6 months with a good colour match.
| Side effects/complications | Total patients (N = 192) |
|---|---|
| Side effects | n (%) |
| Pain | 32 (16.7) |
| Erythema | 16 (8.3) |
| Itching | 11 (3.2) |
| Ulceration | 17 (5) |
| Reversible transient hypo and hyperpigmentation of the donor site | 124 (64.6) |
| Complications of surgical procedure | n (%) |
| Poor or no pigment transfer^ | 4 (2.1) |
| Thick grafts* | 10 (5.2) |
| Upside-down graft# | 2 (1) |
| Graft displacement** | 2 (1) |
| Complications of excimer lamp (308 nm) therapy | n (%) |
| Severe erythema | 2 (1) |
| Blister | 2 (1) |
Discussion
Stable vitiligo can be treated with various surgical modalities, including ultrathin skin grafting.5–15 In this study, ultrathin (0.005 inch/0.1 mm) skin grafts were used for repigmentation. These grafts were thinner than those used by Kahn et al.9,16–18 (0.006 inch/0.1524 mm) and Acikel et al.19 (0.2–0.3 mm). Grafts used by them were taken up as seen in routine course, whereas, in this study, grafts were not taken up as their dermal component was very thin for vascular linkage with the recipient bed; instead, they dried and fell off or were peeled leaving behind tiny islands of pigmentation (transplanted/transferred melanocytes). This was one of the most important findings of this study. This has also not been reported by any of the other studies on UTSG.9,16–21 The ultrathin graft acts as a biological dressing providing protection, support, growth factors, melanocytes and keratinocytes.5,10 The large numbers of melanocytes directly migrate from the graft, get entrapped in the dermabraded or laser-ablated wound and multiply to re-pigment the vitiliginous lesion of any size, shape and site with natural colour match and excellent cosmesis. It does not require laboratory equipment and chemicals or facility of state-of-the-art laboratory set up, etc.5,8,11–14 However, it can cover the vitiliginous area only in a 1:1 ratio and this procedure requires surgical expertise.5,10 Another advantage of the ultrathin skin graft used in this study was that no peri-lesional halo occurred postoperatively as it contained minimal dermal elastin fibres, which are mainly responsible for contraction.22
De-epithelialization of the vitiliginous area was carried out either by dermabrasion9,16,17,20,21 or carbon dioxide laser18,19 in earlier reported studies. We preferred carbon dioxide laser ablation over dermabrasion as it is less time-consuming, with no aerosolization or blood splatter, the operative field is completely visible and bloodless, and it achieves precise de-epithelialization with minimal collateral thermal damage even on the irregular shapes and surfaces.23,24 Oh et al.25 obtained epidermal-dermal split with a bubbling effect in a single pass using an ultra-pulse carbon dioxide laser. In this study, using the freehand technique, the epidermal-dermal/mucosal split with a bubbling effect was achieved with a completely defocused beam of uniform intensity, and a high tissue temperature was reached (100°C boiling point) to cause its ablation.24 In addition, surgical glue was used to secure and immobilise the grafts since it can retain them even over mobile areas and is also anti-microbial.10,22,26
Phototherapy [PUVA/PUVA sol, narrow-band ultraviolet B, excimer laser/lamp (308 nm)] has been successfully used to accelerate pigmentation after various vitiligo surgeries.5,20,21,27,28 The excimer laser/lamp brings clinical improvement in vitiligo through suppression of the mediating ‘T’ cells and by stimulation, migration, and proliferation of melanocytes.29,30 After UTSG we used excimer lamp therapy instead of other phototherapies, since its administration is restricted to a localised area thus rendering it less phototoxic/photocarcinogenic. Also, there is no oral consumption of psoralen.27,28 In a study of 40 cases with 84 sites, Majid and Imran20 reported >90% repigmentation in 83% of patients at various body sites to achieve good to excellent cosmetic match using UTSG supplemented with narrow-band ultraviolet B therapy. Kahn and Cohen,9 in a series of 17 patients, achieved 95–100% repigmentation in 88% of the patients, and the rest 12% had 50–75% over a period of 6 months to one year. The colour match was nearly perfect in most of the patients. Pinjala et al.21 reported repigmentation in 100% of the cases, with excellent in 33.3%, good in 41.7% and average in 25% in a study of 12 cases of vitiligo using UTSG. Seven patients (58.33%) required further treatment with PUVA to accelerate pigmentation. In a study of 7 patients with 13 sites using thin skin graft (0.2–0.3 mm) after carbon dioxide laser ablation, Acikel et al.19 demonstrated 100% repigmentation with good to excellent colour match in all patients over a period of 6–18 months. The above studies show that UTSG following either dermabrasion or carbon dioxide laser ablation, alone or with phototherapy (PUVA, narrow-band ultraviolet B), achieves nearly 100% repigmentation with a good colour match. In our study of 192 patients (410 lesions) achieved excellent repigmentation with uniform colour match and good cosmesis was achieved in 188 patients (97.1%) at 394 lesions (96.1%). Majid I and Imran20 reported peri-lesional halo in 14 lesions, graft displacement in two patients and hypertrophic scarring at the donor site in two patients. There was no scarring reported at donor sites in other studies.9,18,19,21 In our study, there was neither perilesional halo nor scarring at the donor site, as discussed earlier. Nonetheless, in 16 (3.9%) lesions located on the acral region (fingertips, toe tips), there was poor or no repigmentation as these areas are difficult to treat. Acral areas show poor response due to various factors such as absence of hair follicles, thick epidermis, trauma (friction) and inability to achieve adequate depth during dermabrasion/ carbon dioxide laser ablation.22 In 10 patients, the grafts did not dry and fall off as they must have been thick (>0.005 inch/0.1 mm). They were taken up as split thickness skin graft to merge well with surrounding skin. In two patients, there was graft displacement over malleolar areas which could be attributed to shearing trauma or improper immobilisation of the ankle joint. These areas healed with moderate pigmentation and achieved complete repigmentation after excimer lamp therapy. In two patients, there was no melanocyte transplant/transfer as grafts were placed upside down. Nevertheless, they achieved excellent repigmentation following re-grafting. Complications observed during excimer lamp therapy were hyperpigmentation following severe erythema in two patients and blister formation in two patients. This could be due to excessive dosage. All four patients improved completely on the termination of excimer lamp therapy. In this study, through melanocyte transplant/transfer in addition to complete repigmentation, uniform textural and natural colour match with excellent cosmesis and relatively fewer side effects were achieved. Ultrathin skin grafting procedure is safe, simple, less time-consuming and can cover vitiliginous areas of any size, shape, and site (except fingertips and toe tips) in one or more sessions. UTSG when supplemented with excimer lamp therapy, accelerates the rate of repigmentation.
Limitations
The limitations of this study are that it is a single-centre and small-sized. Hence large-scale randomised studies are warranted.
Conclusion
Autologous melanocyte transplant/transfer technique by ultrathin skin grafting following carbon dioxide laser ablation is one of the advanced techniques in the armamentarium of a dermatosurgeon. With this repigmentation technique, large stable vitiliginous areas can be covered completely in single or multiple sessions. Moreover, there is a transplant/transfer of melanocytes during the wound healing process, which ultimately renders excellent cosmesis with a uniform textural and natural-looking colour match. Postsurgical addition of excimer lamp therapy aids in faster and better cosmetic outcomes.
Declaration of patient consent
Institutional Review Board permission was obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Surgical treatment of vitiligo; why, when and how. J Eur Acad Dermatol Venereol. 2003;17:518-20.
- [CrossRef] [PubMed] [Google Scholar]
- Psychiatric morbidity in vitiligo: Prevalence and correlates in India. J Eur Acad Dermatol Venereol. 2002;16:573-78.
- [CrossRef] [PubMed] [Google Scholar]
- Revised classification/nomenclature of vitiligo and related issues: The Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma Res. 2012;25:E1-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- IADVL dermatosurgery task force. Standard guidelines of care for vitiligo surgery. Indian J Dermatol Venereol Leprol. 2008;74:S37-S45.
- [PubMed] [Google Scholar]
- Surgical therapy of vitiligo: Current status. Indian J Dermatol Venereol Leprol. 2005;71:307-10.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous miniaturepunch skin grafting in stable vitiligo. Indian J Dermatol Venereol Leprol. 1992;58:310-15.
- [Google Scholar]
- Autologous thin thiersch’s grafts in vitiligo: Experience of 8000 cases, 50000 grafts (1959–98) with modified technique in 198 cases in the year 1997–98. Indian J Dermatol Venereol Leprol. 1999;65:117-21.
- [PubMed] [Google Scholar]
- Modified technique of suction blistering for epidermal grafting in vitiligo. Int J Dermatol. 1999;38:306-309.
- [CrossRef] [PubMed] [Google Scholar]
- Repigmentation in vitiligo patients. Melanocyte transfer via ultra-thin grafts. Dermatol Surg. 1998;24:365-67.
- [PubMed] [Google Scholar]
- Ultrathin Skin Grafting (UTSG): Melanocyte transplant/transfer. Textbook of dermatosurgery and cosmetology principles and practice Vol vol 45. (3rd ed). Mumbai, India: Bhalani Publishing House; 2018. p. :585-95.
- Long-term follow-up of leucoderma patients treated with transplants of autologous cultured melanocytes, ultrathin epidermal sheets and basal cell layer suspension. Br J Dermatol. 2002;147:893-904.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191-94.
- [CrossRef] [PubMed] [Google Scholar]
- Transplantation of in vitro-cultured epidermis bearing melanocytes for repigmenting vitiligo. J Am Acad Dermatol. 1989;21:257-64.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of autologous cultured melanocytes delivered on poly (DL-lactic acid) film: A prospective, open-label, randomized, multicenter study. Dermatol Surg. 2012;38:1981-90.
- [CrossRef] [PubMed] [Google Scholar]
- Keratinocyte-Melanocyte graft technique followed by PUVA therapy for stable vitiligo. Indian J Dermatol Venereol Leprol. 2008;74:622-4.
- [CrossRef] [PubMed] [Google Scholar]
- Vitiligo: Treatment by dermabrasion and epithelial sheet grafting. J Am Acad Dermatol. 1995;33:646-8.
- [CrossRef] [PubMed] [Google Scholar]
- Repigmentation in vitiligo patients. Melanocyte transfer via ultra-thin grafts. Dermatol Surg. 1999;25:669-70.
- [PubMed] [Google Scholar]
- Grafting following short-pulse carbon dioxide laser de-epithelialization. Dermatol Surg. 1996;22:965-7.
- [CrossRef] [PubMed] [Google Scholar]
- Carbon dioxide laser resurfacing and thin skin grafting in the treatment of “stable and recalcitrant” vitiligo. Plast Reconstr Surg. 2003;111:1291-8.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrathin split-thickness skin grafting followed by narrowband UVB therapy for stable vitiligo: An effective and cosmetically satisfying treatment option. Indian J Dermatol Venereol Leprol. 2012;78:159-64.
- [CrossRef] [PubMed] [Google Scholar]
- Ultra thin epidermal skin grafting for stable vitiligo: a cost effective and cosmetically satisfying treatment option. J Evol Med Dent Sci. 2015;43:7436-41.
- [Google Scholar]
- Tissue grafts in vitiligo surgery - past, present, and future. Indian J Dermatol. 2009;54:150-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparison of recipient site preparations in epidermal grafting for vitiligo: Suction blister and CO2 laser. J Eur Acad Dermatol Venereol. 2009;23:1448-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Carbon Dioxide (CO2) and Erbium: YAG. Lasers: Textbook of Dermatosurgery and Cosmetology Principles and Practice Vol vol 63. (3rd ed). Mumbai, India: Bhalani Publishing House; 2018. p. :62:743-65.
- Treatment of vitiligo with suction epidermal grafting by the use of an Ultrapulse CO2 laser with a computerized pattern generator. Dermatol Surg. 2001;27:565-8.
- [CrossRef] [PubMed] [Google Scholar]
- Use of octyl-2-cyanoacrylate for skin closure in facial plastic surgery. Plast Reconstr Surg. 1998;102:2209-19.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of split-skin grafting in combination with excimer laser for stable vitiligo. Dermatol Surg. 2010;36:499-505.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized comparison of excimer laser versus narrow-band ultraviolet B phototherapy after punch grafting in stable vitiligo patients. J Eur Acad Dermatol Venereol. 2012;26:690-95.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of a 308-nm excimer laser in treatment of vitiligo: A review. Lasers Med Sci. 2013;28:1035-1041.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of vitiligo with the 308-nm xenon chloride laser. Arch Dermatol. 2002;138:1619-20.
- [PubMed] [Google Scholar]






