Translate this page into:
Rosacea fulminans
Correspondence Address:
Hong Yi Koh
National Skin Centre(s) Pte Ltd., 1 Mandalay Road, Singapore 308205, Republic of Singapore
| How to cite this article: Koh HY, Ng SK, Tan WP. Rosacea fulminans. Indian J Dermatol Venereol Leprol 2014;80:272-274 |
Sir,
Rosacea fulminans is an intensely inflammatory facial eruption that affects young women. It can be mistaken for cutaneous infections and inappropriately treated with surgery or short courses of antibiotics. Accurate diagnosis and treatment reduces the potential for scarring.
A 32-year-old woman presented with a painful facial eruption which started 2 years ago as a carbuncle. The first culture from pus grew Enterobacter but the rash responded only partially to incision and drainage and various antibiotics including cephalexin, cloxacillin, co-amoxiclav and ciprofloxacin. The patient was then suspected to have nodulocystic acne vulgaris and isotretinoin at 15 mg daily initially led to resolution, but she relapsed after 7 months of treatment. She was afebrile and had no relevant medical or drug history. Physical examination showed erythema, edema and multiple pustules over most of the face [Figure - 1]. The total white cell count was 10.9 × 10 9 /L with neutrophilia (81.3%). Erythrocyte sedimentation rate was 59 mm/h. Repeat cultures for bacteria, fungi and mycobacteria were negative and serum antinuclear antibody was non-reactive. Skin biopsy from a pustule on an erythematous, edematous plaque on the cheek showed a folliculo-centric infiltrate of neutrophils within the upper to mid-dermis with a ruptured hair follicle, upper dermal edema and superficial and mid-dermal perivascular lymphocytic infiltrate [Figure - 2]. Rosacea fulminans was diagnosed and she was treated with doxycycline 100 mg twice a day, topical metronidazole gel and 2 weeks of indomethacin. The facial erythema and edema improved with cessation of new pustule formation. After 5 months of doxycycline and topical metronidazole, she achieved complete resolution [Figure - 3].
 |
| Figure 1: Erythematous, edematous plaques with pustules and crusts over the whole face |
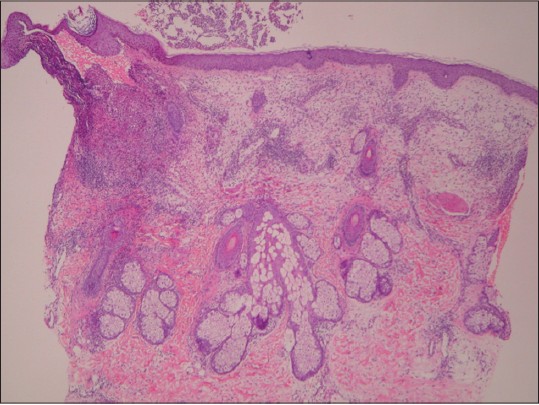 |
| Figure 2: Folliculocentric infi ltrate of neutrophils in the upper to mid-dermis with ruptured hair follicle, upper dermal edema and superfi cial and mid-dermal perivascular lymphocytic infi ltrate |
 |
| Figure 3: Complete resolution with mild scarring after 5 months of treatment with doxycycline, non-steroidal anti-infl ammatory drugs and topical metronidazole |
Rosacea fulminans (synonym: pyoderma faciale) is a rare, inflammatory dermatosis that predominantly afflicts women in the 2 nd to 3 rd decades of life. A recent review found about 60 published articles since 1978. [1] It presents as an acute facial eruption of coalescing nodules, pustules and draining sinuses with pronounced erythema and edema. Men are uncommonly affected and extra-facial involvement is rare. [1],[2] A history of seborrhea or sudden increase in oiliness prior to eruption may be elicited. Notwithstanding the fulminant nature of the outbreak, systemic symptoms are uncommon. The etiopathogenesis of rosacea fulminans remains unknown. Plewig et al. in their study classified it as a severe form of rosacea on morphologic and histologic grounds and a history of flushing in their patients, though this classification is not universally accepted. [3],[4] Recently, Kim et al. reported a case of male rosacea fulminans associated with ocular rosacea and a history of papulo-pustular rosacea. [2] Most patients, however, have no prior history of rosacea and the disease usually does not recur after resolution. Significant associations have been reported with inflammatory bowel disease and pregnancy. Less common associations include rheumatoid arthritis, thyroid and liver diseases, oral contraceptive pills, pegylated interferon alpha-2b and ribavirin therapy and high dose vitamins B6 and B12. [3],[5] Some patients recall major emotional experiences before onset of disease. [5]
Histological examination shows extensive dermal and perifollicular inflammatory infiltrates of neutrophils, lymphocytes, histiocytes and occasional eosinophils, giant cells and granulomas. Cultures are either sterile or grow skin commensals, e.g., Staphylococcus epidermidis, Staphylococcus aureus, Corynebacterium or Propionibacterium species. Gram-negative organisms are rarely isolated.
The differential diagnosis includes acne fulminans which generally afflicts adolescent men with a history of acne vulgaris. Acne fulminans has more comedones, hemorrhagic ulcerations, a more extensive distribution on neck and trunk and prominent systemic symptoms including fever, arthralgia, myalgia and osteolytic bone changes. Gram-negative folliculitis usually presents as a flare of follicular pustules after prolonged antibiotic therapy for acne vulgaris. Other considerations include Sweet′s syndrome, halogenoderma, androluteoma and granulomatous infections.
Systemic prednisolone (0.5-1.0 mg/kg/day) is rapidly effective for rosacea fulminans though relapses are common when it is tapered. Isotretinoin may be started concurrently at low dose, or later after inflammation has abated, to maintain remission. A dose of 0.5-1.0 mg/kg/day over 6-12 months is generally required. Oral tetracycline, erythromycin, dapsone and azithromycin have also been used successfully, the latter often employed in pregnancy where alternatives are limited. Topical therapies include compresses, topical steroids and topical antibiotics. While most reports cite isotretinoin as the most effective treatment, our patient relapsed while on the drug and responded instead to a combination of doxycycline, non-steroidal anti-inflammatory agents and topical metronidazole. Most patients achieve remission within 1 year and relapses are uncommon. Scarring is a significant sequelae. [5]
| 1. |
Ribeiro LB, Ramos-e-Silva M. Rosacea fulminans. Cutis 2013;92:29-32.
[Google Scholar]
|
| 2. |
Kim TG, Noh SM, Do JE, Lee MG, Oh SH. Rosacea fulminans with ocular involvement. Br J Dermatol 2010;163:877-9.
[Google Scholar]
|
| 3. |
Plewig G, Jansen T, Kligman AM. Pyoderma faciale. A review and report of 20 additional cases: Is it rosacea? Arch Dermatol 1992;128:1611-7.
[Google Scholar]
|
| 4. |
Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol 2002;46:584-7.
[Google Scholar]
|
| 5. |
Massa MC, Su WP. Pyoderma faciale: A clinical study of twenty-nine patients. J Am Acad Dermatol 1982;6:84-91.
[Google Scholar]
|
Fulltext Views
12,027
PDF downloads
4,191





