Translate this page into:
Rosai-dorfman syndrome
Correspondence Address:
Najeeba Riyaz
Arakkal, Chalappuram, Calicut-673 002, Kerala
India
| How to cite this article: Riyaz N, Khader A, Sarita S. Rosai-dorfman syndrome. Indian J Dermatol Venereol Leprol 2005;71:342-344 |
Abstract
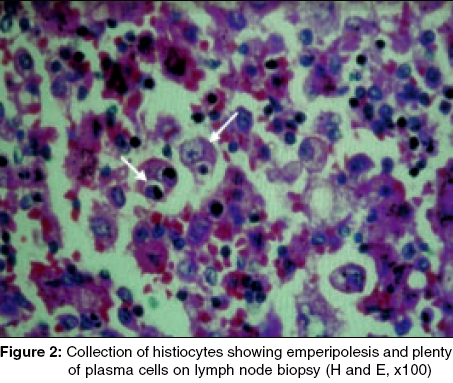
Rosai-Dorfman syndrome is characterized by sinus histiocytosis with massive lymphadenopathy. A 25-year-old woman presented with multiple erythematous and yellowish papules on the forehead, cheeks, chin and thigh. She had massive generalized, firm, non-tender and non-matted lymphadenopathy and mild hepatomegaly. Her hemogram was normal. A skin biopsy showed collections of histiocytes with emperipolesis and plenty of plasma cells. A lymph node biopsy showed partial loss of architecture, dilated sinuses filled with histiocytes, which showed lymphocytophagocytosis, anisonucleosis and a clear cytoplasm. She was referred to an oncologist for further management.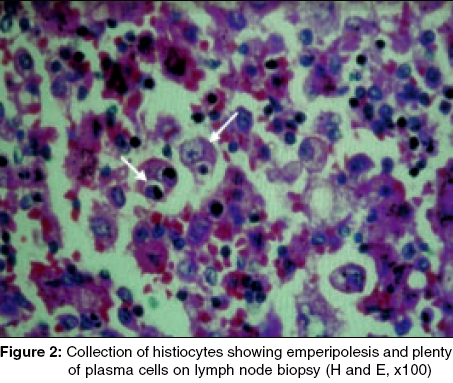 |
 |
 |
 |
Introduction
Sinus histiocytosis with massive lymphadenopathy (SHML) was first reported by Rosai and Dorfman in 1969 as a histopathological entity consisting of cervical lymphadenopathy, which showed marked dilatation of the lymph node sinuses containing histiocytes.[1] SHML is a rare self-limited pseudolymphomatous disorder of unknown etiology usually presenting with cervical lymphadenopathy, fever, elevated ESR and hematological abnormalities.[2] Subsequently, other lymph nodes are involved as well as extra-nodal sites like the skin and mucosae,[3] spinal cord,[4] pancreas,[5] etc. In 1978, Thawerani et al emphasized the cutaneous manifestations Rosai-Dorfman syndrome. We report a case of Rosai-Dorfman syndrome with cutaneous lesions.[6]
Case Report
A 25-year-old woman was seen with a history of multiple swellings in the neck associated with a febrile illness of 4 years′ duration. The swellings had gradually increased in size and number, and other swellings had developed in the axillae and groins. Asymptomatic skin lesions had started developing on the face and left thigh since 1 year.
On examination, she was moderately built and nourished and had mild pallor. The cervical, axillary and inguinal lymph nodes were grossly enlarged, 2-3 cm in size, firm, nontender and non-matted in a bilaterally symmetrical pattern. Mild hepatomegaly was present.
Dermatological examination showed multiple erythematous, skin colored and yellowish, infiltrated, discrete and confluent papules on the forehead, cheeks and chin [Figure - 1], with erythematous and pigmented papulonodules on the left thigh.
Her hemoglobin was 11 g/dl; total count, 10,900 cells/cmm; ESR, 14 mm/hr; total proteins, 8.8 g/dl; albumin, 2.9 g/dl; and globulins, 5.9 g/dl. The serum lipid profile and chest X-ray were within normal limits.
A skin biopsy showed collections of histiocytes in the dermis. The histiocytes showed emperipolesis (i.e. intact lymphocytes within the cells) [Figure - 2] and plenty of plasma cells.
The cervical lymph node biopsy showed partial loss of architecture, dilated sinuses filled with histiocytes, lymphocytes and plasma cells. The histiocytes showed lymphocytophagocytosis, anisonucleosis and a clear cytoplasm.
With the classical features of massive lymphadenopathy and evidence of sinus histiocytosis and the histopathological features of lymph node and skin lesions, a diagnosis of SHML (Rosai-Dorfman syndrome) was made.
Since the patient was asymptomatic and there is no specific treatment for the cutaneous lesions of SHML, she was referred to an oncologist for further management.
Discussion
SHML, though a benign disorder, can sometimes behave in an aggressive manner, leading to significant morbidity and mortality. It can affect any age group, but 80% of patients are in the first or second decade. There is no sexual predilection. Its etiology still remains obscure, but two hypotheses have been proposed: a disturbance in cell mediated immunity, and a focus of infection due to Epstein-Barr virus, Klebsiella, Brucella or human herpesvirus-6.
Massive cervical lymphadenopathy is the hallmark of this condition. The axillary, inguinal and mediastinal nodes may be affected. The cutaneous manifestations, which develop in about 10% of patients, are asymptomatic xanthoma-like, yellowish or reddish-brown papules, nodules and plaques which may ulcerate.[6] Involvement of extra-nodal sites like the nasal cavity, paranasal sinuses, eyelids, orbit, skeletal system, salivary glands and central nervous system have been reported. [2],[3],[4], Fever, elevated ESR, neutrophilia, polyclonal gammopathy are other common associations.
The histopathology is very characteristic, a dermal infiltrate composed predominantly of histiocytes with large vesicular nuclei and abundant pale cytoplasm, and emperipolesis of histiocytes. Emperipolesis means lymphocytophagocytosis, which differs from phagocytosis in that lymphocytes taken up are not attacked by enzymes and appear intact within the histiocytes. In lymph nodes, the sinuses are dilated and crowded with histiocytes, which show abundant foamy cytoplasm and display emperipolesis. The S100 stain is helpful in identifying the histiocytes of SHML, particularly at extranodal sites and in affected lymph nodes, where the morphological features are somewhat unusual. The distinctive histiocytes of SHML that exhibit emperipolesis, their association with numerous plasma cells and the distension of lymph node sinuses or lymphatics in extra-nodal sites by these cells help distinguish SHML from a variety of benign and malignant disorders in which phagocytosis of cells may be a prominent feature. The latter include melanoma and cancer metastatic to lymph nodes, since malignant cells have the propensity to phagocytose hematopoietic cells. Langerhans cell histiocytosis may manifest primarily in the lymph node, with distension of sinuses by Langerhans cells that have their own distinctive morphologic features. Their nuclei are smaller than those of SHML cells and are frequently irregular and folded with a central groove. Lymphophagocytosis or emperipolesis is not a feature of Langerhans cells, but erythrophagocytosis by sinus histiocytes accompanying these Langerhans cells in addition to the presence of microabscesses, usually eosinophilic, within distended sinuses may be a prominent feature.[7] Histiocytes are S-100 positive, CD1a-negative and do not contain Birbeck granules. However, these marker studies could not be done in our patient because they were not available.
There is no specific treatment for the Rosai-Dorfman syndrome. Treatment is required when the condition is organ threatening or life threatening. The treatment modes include corticosteroids, chemotherapy with a combination of vinca alkaloids and alkylating agents, low dose interferon, radiation therapy and surgery.[4]
| 1. |
Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy: a pseudolymphocutaneous benign disorder: analysis of 34 cases. Cancer 1972;30:1174-88.
[Google Scholar]
|
| 2. |
Innocenzi D, Silipo V, Giombini S, Ruco L, Bosman C, Calviero S. Sinus histiocytes with massive lymphadenopathy- Rosai-Dorfman syndrome: case report with nodal and diffuse mucocutaneous involvement. J Cutan Pathol 1998;25:563-7.
[Google Scholar]
|
| 3. |
Sanchez R, Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. An analysis of 113 cases with special emphasis on its extranodal manifestations. Lab Invest 1977;36:21-2.
[Google Scholar]
|
| 4. |
Bhaskar V, Swamy K, Reddy BK, Supe SS, Kumar RV. Sinus histiocytosis with nodal and extranodal involvement. A case report. J Indian Med Assoc 2003;101:28-30.
[Google Scholar]
|
| 5. |
Wright DH, Richards DB. Sinus histiocytosis with massive lymphadenopathy Rosai-Dorfman syndrome: Report of a case with widespread nodal and extranodal dissemination. Histopathology 1981;5:697-709.
[Google Scholar]
|
| 6. |
Pennys NS, Ahn YS, McKinney EC, McCleod T, Byrne G Jr, Byrnes J, et al . Sinus histiocytosis with massive lymphadenopathy. A case with unusual skin involvement and a therapeutic response to vinblastine loaded platelets. Cancer 1982;49:1994-8.
[Google Scholar]
|
| 7. |
Warnke RA, Weiss LM, Chan JK, Cleary M, Dorfman RM. Chronic histiocytic and dendritic cell proliferation. In: Tumors of lymph nodes and spleen. Washington DC: Armed Forces Institute of Pathology; 1994. p. 358-60.
[Google Scholar]
|
Fulltext Views
4,956
PDF downloads
2,237





