Translate this page into:
Sarcoidosis presenting as a non-healing leg ulcer: A rare occurrence
Corresponding author: Dr. Biswanath Behera, Department of Dermatology, AIIMS, Sijua, Patrapada, Bhubaneswar, Odisha, India. biswanathbehera61@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dash S, Sethy M, Sarkar N, Mishra J, Ayyanar P, Behera B. Sarcoidosis presenting as a non-healing leg ulcer: A rare occurrence. Indian J Dermatol Venereol Leprol. 2024;90:498-500. doi: 10.25259/IJDVL_97_2023
Dear Editor,
Sarcoidosis is a multisystem granulomatous disease of unknown aetiology that most commonly involves the lungs, eyes, lymph nodes and skin. Cutaneous involvement occurs in 25–30% of patients with systemic sarcoidosis, and isolated cutaneous manifestations affect only 10% of patients.1 We report a case of ulcerative sarcoidosis, a rare morphological variant, presenting as a non-healing leg ulcer.
A 52-year-old diabetic, hypertensive woman presented with a gradually enlarging ulceration of 2 months duration on the medial aspect of the right leg. She denied any constitutional or systemic symptoms. She had previously undergone 3 weeks anti-tubercular therapy without any improvement. Cutaneous examination revealed a solitary ulcerated plaque of size 3 × 3 cm on the medial aspect of the lower third of the right leg, with purulent deposits on the floor, sloping edge, indurated margin and erythema over the surrounding skin. In addition, multiple satellite atrophic papules were also noted [Figure 1]. Other mucocutaneous, general and systemic examinations were within normal limits. Differential diagnoses of erythema induratum of Bazin, venous leg ulcer and ulcerative necrobiosis lipoidica were considered. Histopathology from the ulcer edge revealed multiple non-caseating, naked epithelioid granulomas in the dermis and subcutaneous tissue [Figures 2a and 2b]. Polarised light examination of the haematoxylin and eosin–stained section did not reveal any refractile material, ruling out granuloma formation due to a foreign body. Her serum angiotensin-converting enzyme was elevated (86, reference range: 08–65 U/L). The pulmonary function test did not reveal any abnormality. High-resolution computed tomography of the thorax showed bilateral hilar lymphadenopathy and multiple nodules in the right lung with interlobular septal and pleural thickening. Mantoux and interferon–gamma release assay tests were negative. The rest of the biochemical, hematological and radiological parameters were within normal limits. A diagnosis of ulcerative sarcoidosis was made, and the patient was started on oral prednisolone 1 mg/kg/day and weekly 15 mg methotrexate. On follow-up, the ulcer healed completely within 8 weeks, with atrophy of the involved skin [Figure 3].

- Solitary ulcerated plaque on the right leg with multiple satellite atrophic papules.
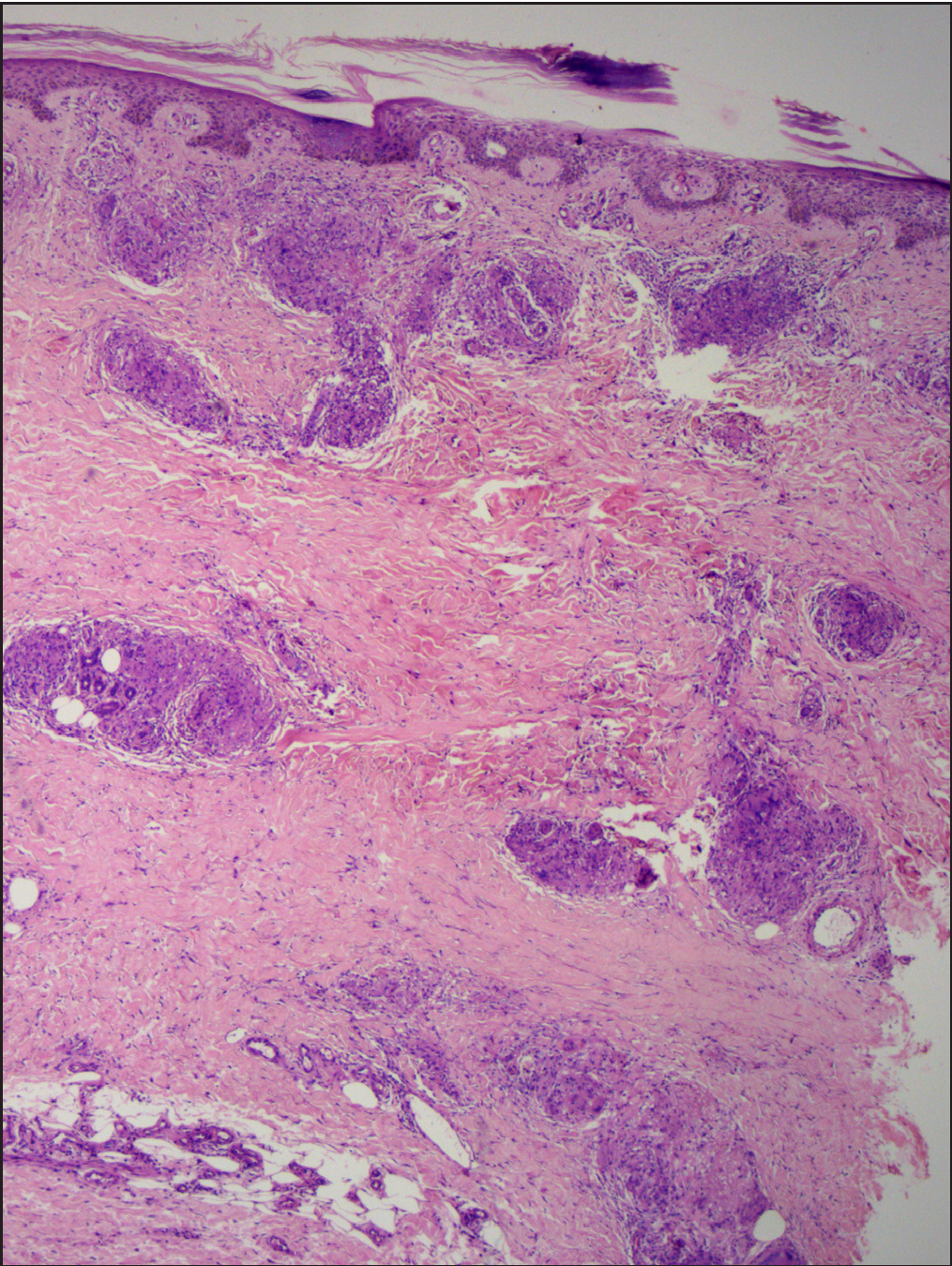
- Histopathology shows multiple non-caseating naked epithelioid granulomas in the dermis and subcutaneous tissue (Haematoxylin & Eosin, 50x)
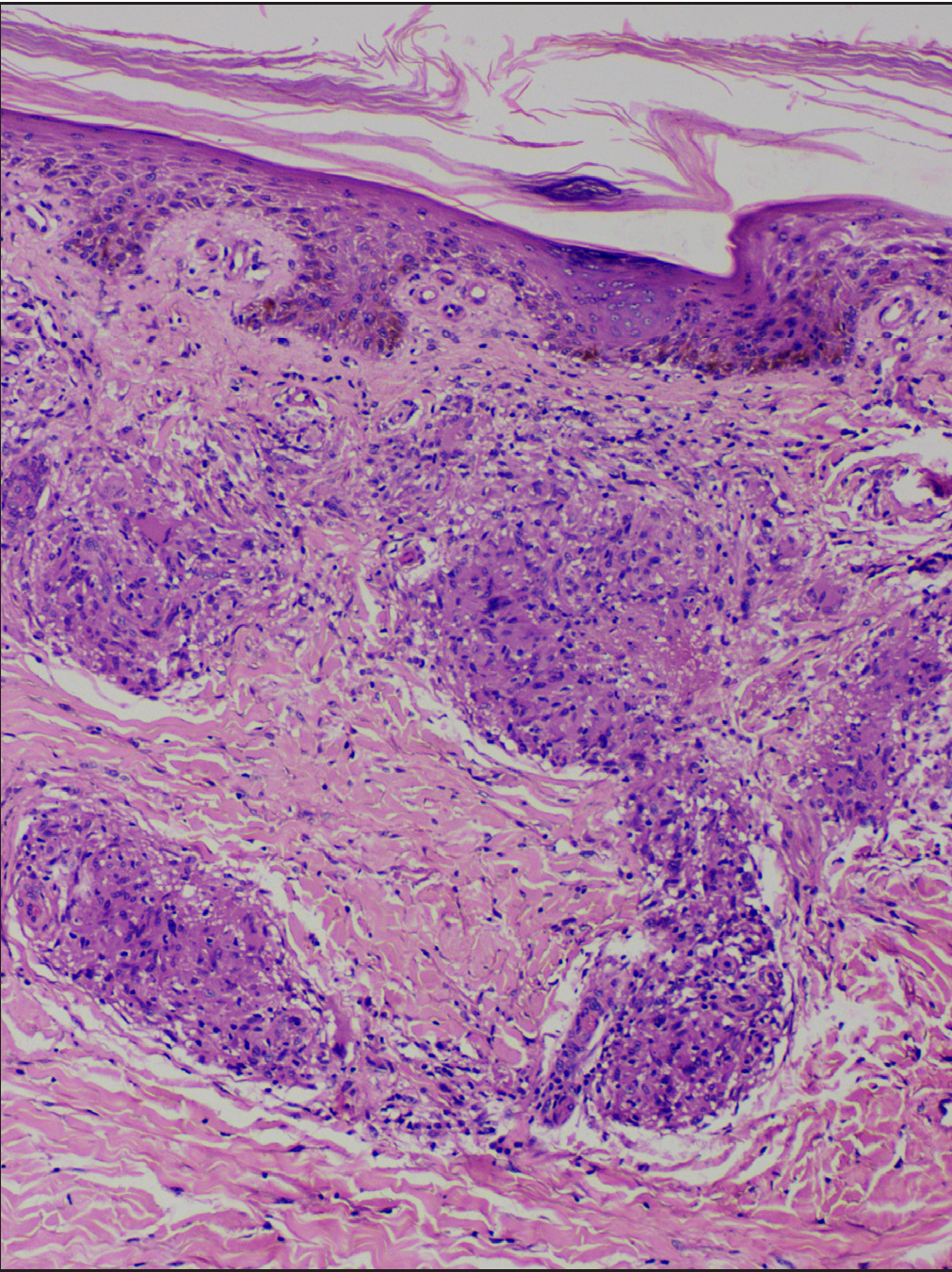
- Naked sarcoid granulomas without any lymphocyte cuffing (Haematoxylin & Eosin, 100x)

- Follow-up at 8 weeks shows healed ulcer with atrophy.
Ulcerative sarcoidosis is a rare, atypical presentation of sarcoidosis, with a predilection for young adults and females of African and Japanese descent.2 Ulcers in sarcoidosis develop within pre-existing lesions, such as papules and nodules, but can also occur de novo.3 The following causes of ulceration in sarcoidosis have been described in the literature: secondary ulceration of specific cutaneous infiltrates with sarcoid granulomas, granulomatous vasculitis or nonspecific.2 The most common location for ulceration is the lower extremities, but it can also occur elsewhere, such as the upper limbs, trunk and face.3 Ulceration can be the earliest manifestation of the disease or can develop during the course of the disease.4,5 In the index case, the leg ulcer was the earliest manifestation of sarcoidosis. Ulcerative lesions are generally associated with systemic involvement. Lung involvement was the most common extracutaneous manifestation found in studies done by Albertini et al. and Ichiki et al., as seen in our case.4,5
Out of numerous causes of non-healing leg ulcers, ulcerative sarcoidosis is a very rare cause. In addition, in India, where tuberculosis is endemic, a diagnosis of ulcerative sarcoidosis can be easily missed unless specifically looked for. Histopathological examination is necessary in all cases of non-healing leg ulcers to reach at an accurate diagnosis.
Non-caseating, naked epithelioid granulomas are the most common histopathological findings seen in biopsies from ulcerative lesions, as seen in our case. Other histopathological findings described in the literature are hyaline degeneration and orceinophilic fibres in the granulomas, mixed inflammatory cell infiltrates with lymphocytes and neutrophils or histiocytes, suppuration with eosinophils and neutrophils in areas of necrosis, solitary sarcoidal granuloma, granulomatous vasculitis, necrotizing granulomas and periarteritis.4
Systemic corticosteroids and methotrexate were found to be effective in treating ulcerative lesions in sarcoidosis, and adalimumab was reported to improve ulcerative lesions that did not respond to corticosteroids.5 Our patient responded well to prednisolone and methotrexate therapy, and the skin lesion completely healed in 8 weeks.
In conclusion, we report an exceptional case of ulcerative sarcoidosis presenting as a non-healing leg ulcer as the sole cutaneous presentation of chronic sarcoidosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cutaneous sarcoidosis—A great masquerader: A report of three interesting cases. Indian J Dermatol. 2011;56:568-72.
- [CrossRef] [PubMed] [Google Scholar]
- Multisystemic sarcoidosis presenting as pretibial leg ulcers. Int J Low Extrem Wounds. 2016;15:263-6.
- [CrossRef] [PubMed] [Google Scholar]
- Leg ulcers revealing systemic sarcoidosis with splenomegaly and thrombocytopenia. Int J Dermatol. 2013;52:1425-7.
- [CrossRef] [PubMed] [Google Scholar]
- Ulcerative sarcoidosis. Case report and review of the literature. Arch Dermatol. 1997;133:215-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ulcerative sarcoidosis: Case report and review of the Japanese literature. Acta Derm Venereol. 2008;88:526-8.
- [CrossRef] [PubMed] [Google Scholar]






