Translate this page into:
Scabies surrepticius masquerading as perforating dermatosis
Corresponding author: Dr. Vinod Kumar Arora, Department of Pathology, University College of Medical Sciences and GTB Hospital, Delhi, India. drvinodkumarora@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal A, Singal A, Devanda R, Arora VK. Scabies surrepticius masquerading as perforating dermatosis. Indian J Dermatol Venereol Leprol. 2024;90:523-5. doi: 10.25259/IJDVL_834_2023
Dear Editor,
Scabies is a parasitic infestation caused by the mite Sarcoptes scabiei var hominis.1 The diagnosis is confirmed by identifying the mite, ova, or excreta on microscopic examination. Classically, the patient presents with generalised excoriated, pruritic papules and pathognomonic burrows usually found in the finger-web space and genitalia.1,2 However, scabies rarely presents with an unusual or atypical morphology with no clue to the underlying infestation.3 ‘Scabies surrepticius’ or ‘scabies incognito’ is a term used for such atypical presentations of scabies.1,3 Here, we present a case of scabies that was not clinically suspected but was diagnosed on histopathology.
A 50-year-old immunocompetent man with poorly controlled diabetes was presented to the skin outpatient department with pruritic papular lesions all over the body. Examination revealed multiple, discrete, erythematous, perifollicular papules and nodules with central keratotic plugs and excoriations over the trunk and proximal parts of upper and lower limbs. Few of these lesions had become secondarily infected. A large 4 cm sized abscess was noted over the left anterior axillary fold [Figure 1a]. Perforating lesions were also seen on the lower limbs and genitalia [Figure 1b]. Three clinical differential diagnoses were considered: perforating dermatosis, prurigo nodularis, and papulonecrotic tuberculid with abscess formation.

- Follicular papules and nodules with a central keratotic ulug on the trunk and arms; note a pyogenic abscess in the left axilla.

- Perforating lesions over the lower abdomen and thighs.
Skin biopsies were performed from two sites: one from the chest and the other from the abdomen. Grossly, the skin biopsy from the chest measured 0.6 x 0.5 x 0.2 cm, and the skin biopsy from the abdomen measured 0.5 x 0.4 x 0.3 cm. In both biopsies, the epidermis and dermis with hair follicles were identified without any subcutaneous adipose tissue.
On microscopy, the epidermis showed marked spongiosis, focal parakeratosis, and epidermal bullae with keratinocyte necrosis. The dermis showed perivascular and perifollicular chronic inflammatory infiltrates showing lymphocytes, plasma cells, and occasional neutrophils with no evidence of transepithelial elimination [Figure 2a]. Findings were non-specific and no conclusive diagnosis could be made. Serial sections were advised. Incidentally, superficial corneal burrows were identified as having inflammatory exudate. One of the burrows showed the exoskeleton of a mite, Sarcoptes scabiei [Figure 2b] and thus a final diagnosis of scabies was made. The patient received systemic antibiotics and topical anti-scabies medication (5% permethrin) twice, with a two-week interval between treatments along with oral antihistamine. The skin lesions resolved completely within four weeks.
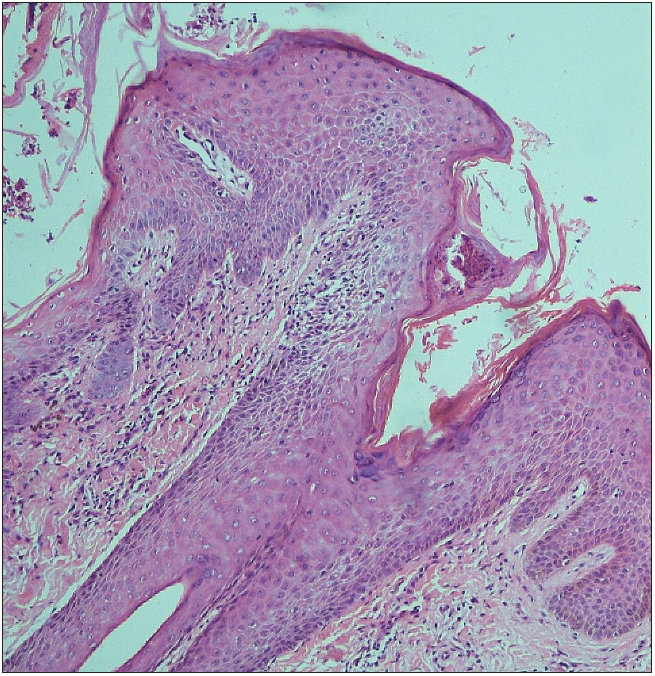
- Epidermal bullae and keratinocyte necrosis (Haematoxylin and eosin; 100x).
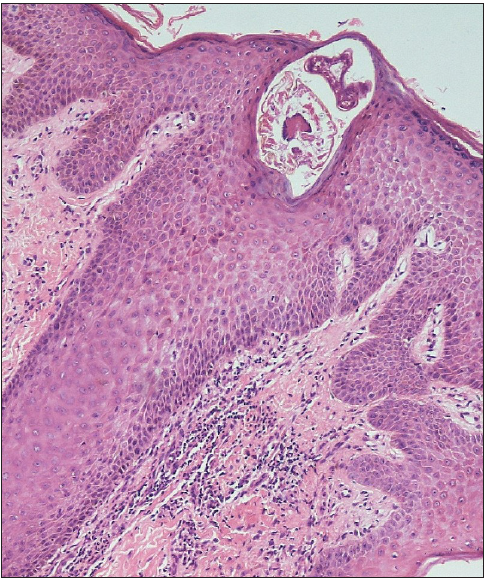
- Mite identified in a subcorneal burrow on serial sections. Note perivascular and perifollicular chronic inflammatory infiltrate in the dermis (Haematoxylin and eosin; 100x).
Scabies is highly contagious, and patients exhibit characteristic burrows overlying interdigital web spaces, wrists, elbows, lower abdomen, axilla, and breasts. However, in our case, the patient presented with perforating papules and nodules.
The diagnosis of scabies is usually made on clinical examination. However, a definitive diagnosis is made by demonstrating the mite, its eggs, or faecal pellets in the skin scrapings. A non-invasive, quick office tool, ‘dermoscopy’, in most cases shows a characteristic jet-plane or hang-glider appearance. A skin biopsy is rarely required. Polymerase chain reaction (PCR) and burrow ink tests are other diagnostic modalities.4 In our case, skin scrapings were not taken as scabies was not suspected clinically owing to its atypical presentation. The skin biopsy, which was performed to establish the diagnosis of perforating dermatoses in an uncontrolled diabetic patient, incidentally, revealed the presence of the mite in serial sections on histopathological examination. Many different variants of scabies have been described, for example, nodular scabies, crusted scabies, and bullous scabies, among others.1,3 Co-existing systemic disorders or infections alter the clinical presentation of scabies.1 Surreptitious scabies, also known as scabies incognito, refers to atypical presentations of scabies that mimic other pruritic dermatoses.1,2,3,5 Unusual manifestations, such as those resembling drug eruptions, Gottron papules, pityriasis rosea, and pruritic bruises associated with child abuse, have been documented in the literature, posing challenges in clinical diagnosis. Table 1 provides a summary of such surrepticius scabies cases.2,3,6,7
| S. No | Case Details | Complaints | Lesion Morphology | Clinical Diagnosis | Confirmatory tests | Final Diagnosis |
|---|---|---|---|---|---|---|
| Cohen et al.1 | 76y/M | Recurrent itchy lesions over chest and abdomen | Red, bullous, pruritic blisters and plaques, Head and neck spared. No burrows | Drug eruption due to linezolid |
HP: CICI with Eo and subepidermal vesicle with Eo. SS: Mite. |
Bullous Scabies |
| Yoshinaga et al.2 | 15y/F | Itchy lesions on upper extremities | Dusky red papules on proximal interphalangeal joints | Gottron papules of dermato- myositis | SS: Mite and eggs | Scabies |
| Werbel et al.3 | 91y/M | Itchy rashes on the body above the waist | Pruritic, excoriated, and erythematous nodules | Acute Folliculitis |
HP: Dermal CICI with Neu. Exoskeleton of mite identified in corneal burrow. |
Incognito and Nodular Scabies |
| Stiff et al.6 | 59y/M | Lesions over the back, buttock, flanks, abdomen, face, forearms, and legs | Scaly papules and annular plaques | Pityriasis rosea | SS: Mites, ova, scybala | Scabies |
| Gunaric et al.7 | 6y/M |
Itchy bruise like lesions since 10 days |
Pruritic bruises | Child Abuse | SS: Mite | Scabies |
| Present case | 50y/M | Raised itchy lesion over the body | Pruritic raised lesions with crusting over the body. No burrows were seen [Figure 1] |
Papulonecrotic tuberculid with Scrofuloderma Prurigo nodularis Perforating dermatoses |
HP: Dermal CICI with Neu. Keratinocyte necrosis in subcorneal burrows along with mites [Figures 2a and 2b] |
Scabies |
HP: Histopathology, SS: Skin Scrapings, CICI: Chronic inflammatory cell infiltrate, Eo: Eosinophils, Neu: Neutrophils
| S.No | Lesion | Morphology | Histopathology |
|---|---|---|---|
| 1. | Perforating Dermatoses5 | Perforating lesions exhibiting transepidermal elimination of substances, e.g., collagen |
Four entities with distinct features:
|
| 3. | Prurigo Nodularis5 | Pruritic, 0.5–3 cm, hyperpigmented, firm nodules having hyperkeratotic or excoriated surface over trunk and extensor surfaces of limbs. | Ortho-hyperkeratosis with focal parakeratosis, hypergranulosis, irregular acanthosis, papillomatosis, and Irregular downward proliferation of the epidermis. Vertically oriented collagen bundles with increased numbers of fibroblasts and capillaries and perivascular chronic inflammatory cells |
| 2. | Papulonecrotic tuberculid5 | Dusky papules and nodules with central necrosis. They leave varioliform scars. | Ulceration, V-shaped areas of necrosis, variable dermal thickness. Palisading histiocytes and chronic inflammatory cells and occasional granulomas. Vasculitis and fibrinoid necrosis in surrounding vessels and follicular necrosis. |
In our patient, three clinical differential diagnoses were considered- perforating dermatoses, prurigo nodularis, and papulonecrotic tuberculid. Their clinical and histological features have been summarised in Table 2.5
In conclusion, the nomenclature “scabies surrepticius” aptly captures its hidden or atypical clinical manifestations, often resembling diverse dermatoses. The incidental diagnosis during the investigation of other medical conditions, as illustrated in the current case, underscores the need for a vigilant approach. Thus, a heightened index of suspicion and comprehensive tissue examinations are imperative to ensure accurate and timely diagnosis, preventing the oversight of this elusive presentation of scabies
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
References
- Scabies masquerading as bullous pemphigoid: Scabies surrepticius. Clin Cosmet Investig Dermatol. 2017;10:317-24.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An adolescent patient with scabies mimicking Gottron papules. Case Rep Dermatol. 2009;2:8-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Scabies presenting as cutaneous nodules or malar erythema: Reports of patients with scabies surrepticius masquerading as prurigo nodularis or systemic lupus erythematosus. Dermatol Online J. 2018;24:8.
- [Google Scholar]
- Epidemiology, diagnosis, and treatment of scabies in a dermatology office. J Am Board Fam Med. 2017;30:78-84.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired perforating collagenosis: A clinico-pathological study of ten. Indian J Pathol Oncol. 2019;6:677-81.
- [Google Scholar]
- Scabies surrepticius: Scabies masquerading as pityriasis rosea. Cureus. 2017;9:e1961.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





