Translate this page into:
Scalp metastases as the first sign of disease recurrence in a patient with jejunal adenocarcinoma
Corresponding author: Dr. Ajay Gupta, Department of Medical Oncology, Indraprastha Apollo Hospital, New Delhi, Jasola, Delhi, India. ajayajaygupta2002@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta A, Zaidi S, Prabhu M, Kashyap V. Scalp metastases as the first sign of disease recurrence in a patient with jejunal adenocarcinoma. Indian J Dermatol Venereol Leprol. 2025;91:S38-S40. doi: 10.25259/IJDVL_428_2023
Dear Editor,
Skin metastases may be the first indication of a clinically silent visceral malignancy, usually signifying widespread systemic disease.1 Scalp metastases are rare and there is no description of scalp metastases from a primary jejunal adenocarcinoma.2,3 We present the details of one such case [Figures 1a–1c].

- Scalp lesion pre-treatment, 4 × 3 cms flesh nodular lesion.

- Scalp lesion recurrence 4 months post-radiation.

- Scalp lesion resolved post-chemotherapy.
The patient, a 65-year-old lady, symptomatic for 3 months with progressive anorexia, loss of weight and vomiting, presented in August 2015 with small bowel obstruction. A contrast-enhanced computed tomography (CECT) scan of the chest and abdomen revealed small bowel obstruction due to a proximal jejunal mass along with metastases to the peritoneum, left adrenal gland and lung. Resection anastomoses revealed a 3 × 3 cm jejunal adenocarcinoma with omental deposits. Three weeks later, she was started on capecitabine and oxaliplatin (CAPOX) chemotherapy for eight cycles. She was in a state of sustained partial remission for over 3 years and CECT imaging done in January 2019 revealed no disease progression.
In December 2019, she developed a red, erythematous scaly scalp lesion, 1 × 1 cm in size, initially mistaken for psoriasis. By March 2020, the lesion grew into a 4 × 3 cm nodule which was red, fleshy, and tender to touch [Figure 1a]. The biopsy from the skin nodule in the scalp showed infiltration of the dermis by a carcinoma composed of discrete as well as fused malignant glands enclosing necrotic cell debris and separated by a small amount of desmoplastic stroma. The glands were lined by atypical columnar epithelium showing moderate delicate cytoplasm with minimal mucin and stratified oval nuclei showing mild pleomorphism and small nucleolus. The tumour did not involve the epidermis. The biopsy findings were consistent with a diagnosis of metastatic jejunal adenocarcinoma [Figures 2a and 2b].
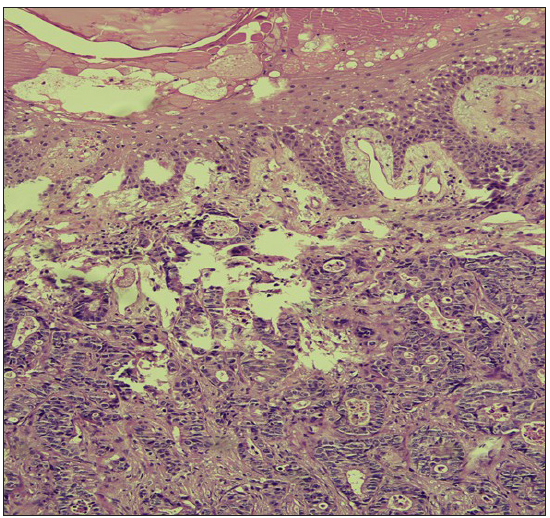
- The dermis shows infiltration by a metastatic carcinoma showing well-formed malignant glands. The epidermis is not involved in the tumour. (Haematoxylin and eosin, 10x).
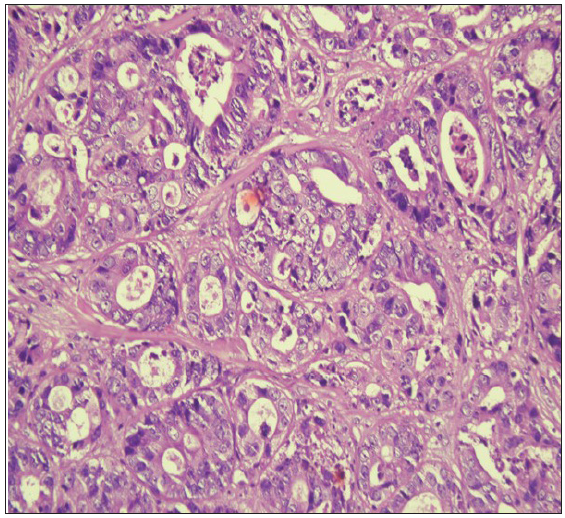
- The malignant glands under higher magnification show a lining of atypical columnar epithelium showing nuclear stratification and mild nuclear pleomorphism. (Haematoxylin and eosin, 20x).
18F-fluorodeoxyglucose (FDG)-positron emission tomography (PET) [Figure 3a] showed active irregular heterogeneously enhancing soft tissue lesions in the scalp at the right high parietal (3.7 × 4.0 cm, SUVmax 9.1) and right supra auricular region (1.6 × 1.0 cm, SUVmax 11.4), with lesions in jejunum, left adrenals, peritoneum and lungs.
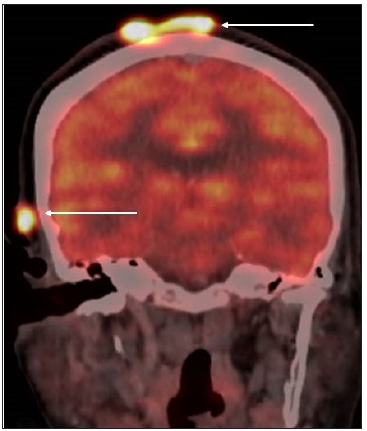
- 18F-fluorodeoxyglucose (FDG)-positron emission tomography (PET) Scan images showing metabolically active irregular heterogeneously enhancing soft tissue lesions in the scalp at the right high parietal (measuring 3.7 × 4.0 cm, Standardized Uptake Value (SUV) max 9.1) and, right s3upra-auricular region (measuring 1.6 × 1.0 cm, SUV max 11.4) as indicated by the white arrows.
She underwent palliative radiation to the scalp lesion in March 2020, resulting in its regression. In August 2020, she came with severe breathlessness due to lung metastases. The scalp lesion was 2 cm in size [Figure 1b]. She was started on chemotherapy with CAPOX and bevacizumab. After completion of 8 cycles of chemotherapy in February 2021, the scalp lesion disappeared clinically [Figure 1c] and on PET CT [Figure 3b]. The patient showed marked symptomatic improvement and was placed on maintenance capecitabine. The disease remained in control till September 2021 when it started progressing with widespread lung metastases. The patient declined further treatment and died in December 2021.
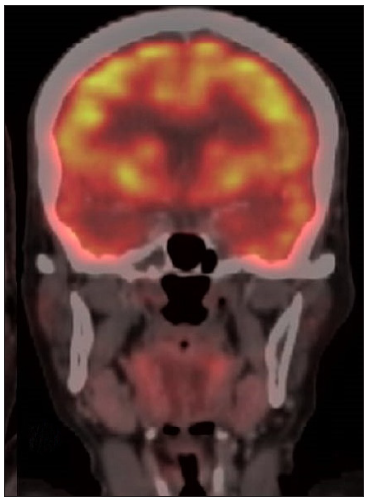
- 18F-fluorodeoxyglucose (FDG)-positron emission tomography (PET) Scan images showing follow-up PET/CT post-chemotherapy show interval resolution of the scalp lesions.
Skin metastases are uncommonly encountered in 0.7–9% of patients with cancer.1 Most commonly associated malignancies are those of the breast, lung, pancreas, gall bladder, stomach, nasal sinuses, larynx, uterus, large intestine, kidneys, melanomas and haematolymphoid malignancies.1,2 Detection requires a high index of clinical suspicion. The average interval between diagnosis of malignancy and skin metastasis is 33 months and the average survival following this is 7.5 months though survival has improved now with better treatments.1,2
The scalp has a rich vascular supply and can be a site of solitary cutaneous metastases.2 They can appear as inflammatory papules, indurated plaques or nodules. Many visceral malignancies, namely, carcinomas of the lung, breast, thyroid, colon, kidney, adrenal glands and larynx, metastasis to the scalp.1,2 Primary cutaneous appendage tumours of the scalp need to be excluded.1,2
Small bowel adenocarcinomas account for 2–3% of primary gastrointestinal malignancies, duodenum (48–73.6%), jejunum (13.2–31%) and ileum (13.2–21%).3 Scalp metastases from a jejunal adenocarcinoma have not been described and this is the first description of such a case. We could find only two reports of associated cutaneous metastases one in the leg and the other in the neck with this tumour.2,3
In conclusion, the appearance of new skin and scalp lesions in a person with a history of visceral malignancy could be the first sign of new metastases, disease recurrence or progression as in our case. It should be investigated keeping a high index of suspicion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Cutaneous metastasis: A clinical, pathological, and immunohistochemical appraisal. J Cutan Pathol. 2004;31:419-30.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous metastasis: A study of 138 cases diagnosed by fine-needle aspiration cytology. Acta Cytol. 2017;61:47-54.
- [CrossRef] [PubMed] [Google Scholar]
- Jejunal adenocarcinoma with cutaneous metastasis. Dermatol Online J. 2015;21:13030.
- [PubMed] [Google Scholar]





