Translate this page into:
Scalp paracoccidioidomycosis: A rare and exuberant manifestation
Corresponding author: Dr. Anna Carolina Miola, Department of Dermatology and Radiotherapy, Av. Prof. Mário Rubens Guimarães Montenegro, w/n, Rubião Junior District, CEP 18.618-687, Botucatu, São Paulo, Brazil. anna.c.miola@unesp.br
-
Received: ,
Accepted: ,
How to cite this article: Camillo MC, Andrade MI, Soares CT, Nakandakari S, Miola AC. Scalp paracoccidioidomycosis: A rare and exuberant manifestation. Indian J Dermatol Venereol Leprol 2021;87:246-8.
Sir,
Paracoccidioidomycosis, a granulomatous infectious disease, is caused by the dimorphic species Paracoccidioides brasiliensis, P. lutzii (Pb01) complex and Pb01-like. According to epidemiological studies, approximately 50% of the inhabitants of Brazil, Venezuela, Colombia and Argentina have already been exposed to P. brasiliensis, which infects humans through inhalation.1 However, only a small proportion develops clinical manifestations. Cases are divided into paracoccidioidomycosis infection (without signs and symptoms) and paracoccidioidomycosis disease, which is subdivided into acute, subacute, chronic and associated with immunosuppression. The chronic form is more common in adults and the most affected organs are the lungs, respiratory tract and skin.2 The scalp is rarely affected and may be similar to some skin tumors and other infectious diseases such as tuberculosis. This case presents an exuberant chronic paracoccidioidomycosis on the scalp and its incidence is an alert to include it as a differential diagnosis of lesions on the scalp, specifically in endemic areas.
A 59-year-old man presented with lesions on the scalp of 6 months duration. On physical examination, we observed multiple plaques with central atrophic scarring on the scalp. Numerous papules with pin point hemorrhages were seen infiltrating the edges of the plaques [Figure 1]. Potassium hydroxide mount revealed budding yeast cells. A histopathological examination revealed well-formed non-caseating granulomas and periodic acid-Schiff staining with diastase and silver-methenamine stain showed multiple budding yeast cells in a wheel-like configuration [Figures 2a and b]. A chest X-ray was performed which showed slight pulmonary interstitial infiltrates. Human immunodeficiency virus enzyme-linked immunosorbent assay was negative. The culture of the lesion was positive for P. brasiliensis. With the confirmed diagnosis of paracoccidioidomycosis, we initiated the treatment with oral itraconazole 200 mg twice daily. A progressive improvement was noticed in 30 days [Figure 3] and complete healing occurred after 3 months. The treatment was maintained for 12 months.

- Multiple plaques with central atrophic scarring and numerous papules with pin point hemorrhages infiltrating the edges on the scalp
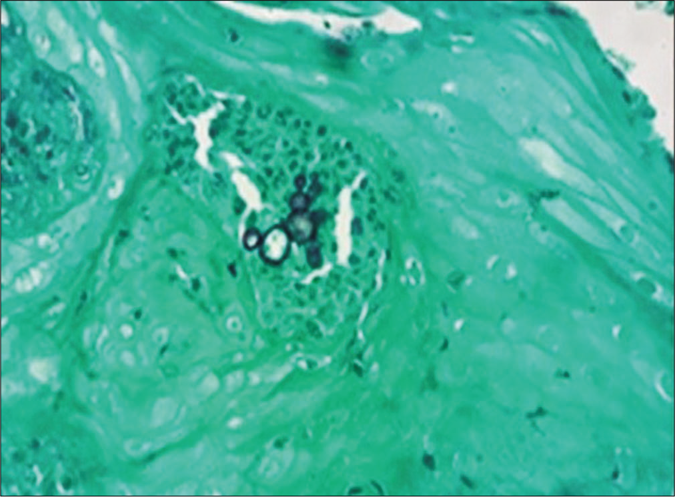
- Multiple Budding yeast cells (silver-methenamine, x400)
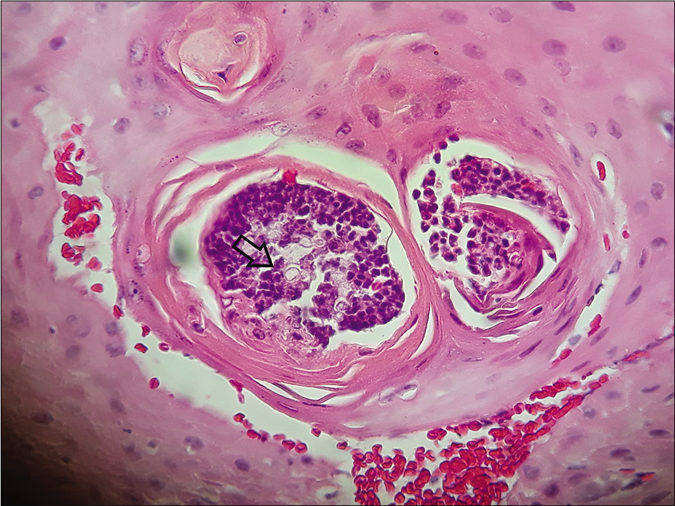
- Multiple budding yeast cells (arrow) (hematoxylin and eosin, x400)
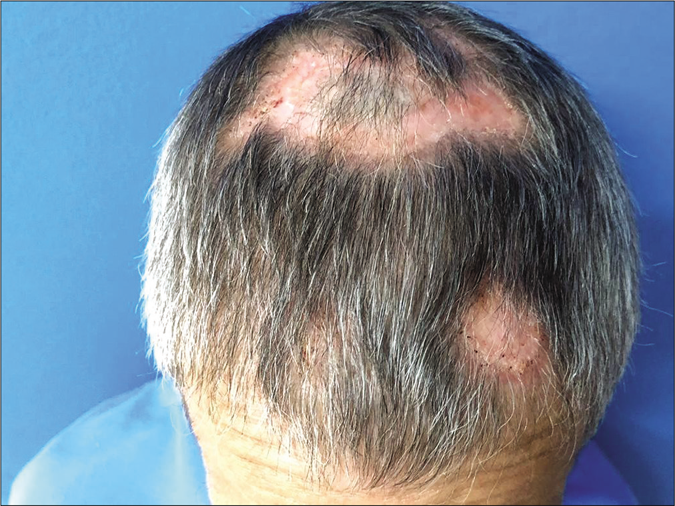
- Clinical improvement of the lesions after 1 month of treatment
Regarding skin lesions, there are two polarized clinical expressions, which may be described as hyperergic and anergic. On the hyperergic pole, sarcoid-like lesions which may evolve to ulcers are mostly seen. There are also verrucous lesions, which are generally observed in patients with a more balanced host-parasite equilibrium.1 Besides the skin, mucous membranes may be affected in paracoccidioidomycosis patients, with superficial ulcers characterized by microgranulation, pinpoint hemorrhages and infiltrated borders.2
The most commonly affected area in chronic paracoccidioidomycosis is head with almost 50% involving the orofacial region.3
It is important to differentiate paracoccidioidomycosis on the scalp from squamous cell carcinoma, amelanotic melanoma and metastatic lesions, which are more common in this area.4 In this case, the epidemiological aspects were significant enough to add paracoccidioidomycosis in the differential diagnosis. In addition, the presence of hemorrhagic stippling on the periphery of lesions evoked the moriform appearance commonly described in chronic paracoccidioidomycosis. A biopsy is important to exclude the neoplastic conditions mentioned above, which are treated as oncological emergencies. Besides malignancies, other infections like cutaneous tuberculosis, syphilis, leishmaniasis and blastomycosis should be considered and a tissue culture is regarded as a reliable diagnostic tool. When cultured, paracoccidioidomycosis has to be differentiated from blastomycosis, a fungal infection similar to paracoccidioidomycosis, through gemulation: Blastomyces has simple budding and Paracoccidioides has multiple budding (wheel-like configuration). Furthermore, a biopsy may present the same structures and differentiate blastomycosis from paracoccidioidomycosis.
The magnitude of the skin lesion is also relevant because it reveals the intensity of the Th1 immune response, which is the main resistance mechanism against P. brasiliensis. The well-formed granulomas in the dermis, good response to treatment and mild lung involvement were helpful to emphasize this hypothesis in our case.5
Paracoccidioidomycosis is a disease of great importance for dermatologists, especially in endemic areas, as an early diagnosis and treatment can reduce scars and functional sequelae.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Paracoccidioidomycosis: Current Perspectives from Brazil. Open Microbiol J. 2017;11:224-82.
- [CrossRef] [PubMed] [Google Scholar]
- Paracoccidioidomycosis: Epidemiological, clinical, diagnostic and treatment up dating. An Bras Dermatol. 2013;88:700-11.
- [CrossRef] [PubMed] [Google Scholar]
- Head and neck manifestations of paracoccidioidomycosis: An epidemiological study of 36 cases in Brazil. Mycopathologia. 2012;173:139-44.
- [CrossRef] [PubMed] [Google Scholar]
- Paracoccidioidomycosis and cryptococcosis with localized skin manifestations: Report of two cases in the elderly. An Bras Dermatol. 2016;91:243-4.
- [CrossRef] [PubMed] [Google Scholar]





