Translate this page into:
Scarification practice and scar complications among the Nigerian Yorubas
Correspondence Address:
Olaitan Peter Babatunde
Burns and Plastic Surgery Unit, Department of Surgery, Ladoke Akintola University of Technology Teaching Hospital,Osogbo-3141
Nigeria
| How to cite this article: Babatunde OP, Oyeronke AE. Scarification practice and scar complications among the Nigerian Yorubas. Indian J Dermatol Venereol Leprol 2010;76:571-572 |
Sir,
Scarification involves cutting or making an incision into the skin and then allowing the wound to heal, leaving a permanent scar. The incision is usually accompanied by rubbing of some herbal concoction, which is expected to mix with the blood and serve the purpose for which the scarification is made. The wound often heals leaving tiny hyperpigmented marks. Many ailments and diseases are claimed to be cured through this practice. Several complications, including keloids and hypertrophic scars have been observed following these procedures in Black Africans.
A set of semi-structured questionnaires were administered to 143 adult Nigerians to study the practice and scar complications of scarification in Nigerians.
Respondents included 44 (30.8%) males and 99 (69.2%) females with a mean age of 21.4 years.
Majority 104 (72.7%) of the respondents had tertiary education, whereas only 6 (4.2%) had no formal education at all. One hundred and seventeen (81.8%) of the respondents knew about scarification. Seventy-three (51.0%) had scarification at one time or another. Consent was given by only 20 (14.0%) before they were given scarifications. Scarifications were given by native/traditional doctors in 23 (16.1%), 25 (17.5%) by subjects′ fathers, 12 (8.4%) by mothers, and 9 (6.3%) by uncles.
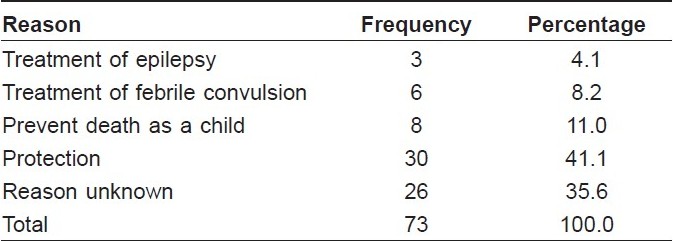
A razor blade was the most commonly used instrument for scarification in 60 (42.0%) of the respondents, whereas knife was used in 13 (9.1%) of them. Thirty-three (23.1%) of the respondents used a single instrument, whereas 30 (21.0%) had shared the instruments with 2 or more others. Religion and education did not appear to affect the scarification practice. The reasons given for scarifications included protection from evil, 30 (41.1%), treatment of febrile convulsion, 6 (8.2%), and treatment of epilepsy, 3 (4.1%) [Table - 1].
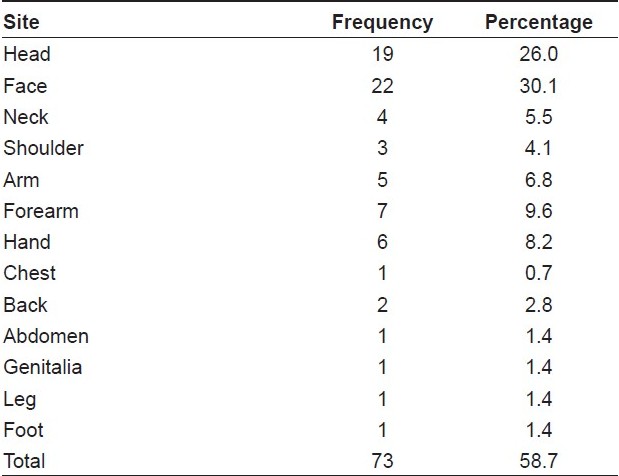
Only 15 (10.5%) would still accept scarification/tribal marks if offered again. The face was the commonest site of scarification in 22 (30.1%) followed by the head, 19 (26.0%), the forearm. 7 (9.6%), and the hand, 6 (8.2%). Others are as shown in [Table - 2].
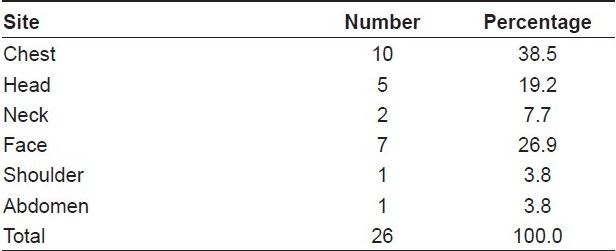
Twenty-six (35.6%) of the respondents who had scarifications, had the scarification marks becoming hypertrophied/keloidal. The marks on the chest gave most of this problem with 10 (13.7%), head 5 (6.8%), neck 2 (2.7%), face 7 (9.6%), whereas the shoulder and abdomen have 1 (1.4%) hypertrophic scar/keloids each [Table - 3].
Tribal scarification is common in West Africa. [1] Ritual scarification is the culturally sanctioned process of incising the skin to achieve patterned scars. Scarification was practiced widely by traditional societies, but increasingly becoming uncommon. [2] This practice is deleterious, diversionary, and causes complications.
Our current study showed that nonsterile razor blades and knives were commonly used, which were often shared with 2 or more people. It has also been observed that scarification results in hypertrophic or atrophic scars.
Scars are a natural part of the dermal healing process and consist of networks of fibrous collagen tissue, laid down in response to injury to the dermis. [3] Hypertrophic scars and keloids are 2 forms of excessive cutaneous scarring that occur in predisposed individuals. [4] This pathology has been observed to be commoner in Blacks and any injury could bring it up.
Cutaneous scarification has also been observed to be associated with sarcoidosis [1] and Hepatitis B infections.
People with a family history of keloids and abnormal scars as well as those who are predisposed to developing abnormal scars should therefore be educated to avoid scarification.
Although negative psychosocial impacts of keloids on the Yorubas from Nigeria have been found to be low, [5] efforts should be made to discourage this practice in these people who are predisposed to abnormal scarring. Education including public enlightenment campaign should effectively check the practice.
| 1. |
Alabi GO, George AO. Cutaneous sarcoidosis and tribal scarifications in West Africa. Int J Dermatol 1989;28:29-31.
[Google Scholar]
|
| 2. |
Mammen L, Norton SA. Facial scarification and tattooing on Santa Catalina Island (Solomon Islands). Cutis 1997;60:197-8.
[Google Scholar]
|
| 3. |
Jalali M, Bayat A. Current use of steroids in management of abnormal raised skin scars. Surgeon 2007;5:175-80.
[Google Scholar]
|
| 4. |
Iannello S, Milazzo P, Bordonaro F, Belfiore BF. Low-dose enalapril in the treatment of surgical cutaneous hypertrophic scar and keloid-two case reports and literature review. Med Gen Med 2006;8:60.
[Google Scholar]
|
| 5. |
Olaitan PB. Keloids: Assessment of effects and psychosocial impacts on subjects in a black African population. Indian J Dermatol Venereol Leprol 2009;76:32-6.
[Google Scholar]
|
Fulltext Views
4,794
PDF downloads
1,652





