Translate this page into:
Scleredema of Buschke associated with lichen sclerosus: Three cases
2 Clinic of Dermatology, Ss. Cyril and Methodius University, Skopje, Republic of Macedonia
3 Dermatology Clinic, AOU Cagliari, Cagliari, Italy
Correspondence Address:
Michela Venturi
“Mario Aresu” Department of Medical Science, Section of Dermatology, University of Cagliari, Via Ospedale 51, 09124, Cagliari
Italy
| How to cite this article: Venturi M, Damevska K, Ferreli C, Pinna AL, Atzori L, Gocev G, Rongioletti F. Scleredema of Buschke associated with lichen sclerosus: Three cases. Indian J Dermatol Venereol Leprol 2020;86:272-277 |
Abstract
Scleredema adultorum of Buschke is a rare fibromucinous, scleroderma-like connective tissue disease most commonly found in a post-infectious setting or linked to hematological disorders or diabetes. Lichen sclerosus et atrophicus is an autoimmune condition only in 2.5% of cases localized exclusively at an extragenital site, occurring in up to 34% of patients in association with other autoimmune diseases such as vitiligo, thyroid disorders, alopecia areata, lichen planus, morphea, pernicious anemia and systemic lupus erythematosus. In particular, a stronger link with an autoimmune background in lichen sclerosus et atrophicus has been observed in women who showed higher prevalence for autoimmune conditions and circulating autoantibodies. Literature reveals a genetic susceptibility linked to specific HLA types. We report three patients who developed lichen sclerosus et atrophicus superimposed on skin involved by scleredema adultorum of Buschke. Although the association of lichen sclerosus et atrophicus with scleredema adultorum of Buschke could be coincidental, both diseases could be considered part of the spectrum of sclerodermoid disorders with common underlying pathogenetic mechanisms; which could explain the sequential or simultaneous occurrence of both lesions in our patients.
Introduction
Scleredema adultorum of Buschke is a rare fibromucinous connective tissue disease belonging to the group of primary mucinoses and scleroderma-like disorders.[1] It can be classified in a diabetic (accounting for 25–50% of cases) and a nondiabetic type, that includes an idiopathic, a post-infective, a monoclonal gammopathy-associated type and one described in association with some anecdotal miscellaneous conditions.[1]
In addition, scleredema adultorum of Buschke was reported with other dermatosis such as necrobiosis lipoidica in a diabetic patient,[2] acquired immune deficiency syndrome-related lipodystrophy[3] and eosinophilic fasciitis.[4]
Lichen sclerosus et atrophicus is a sclerosing chronic inflammatory dermatosis of the genital area and less commonly localized in extragenital sites.[5]
We were unable to find any previous reports of lichen sclerosus et atrophicus in association with scleredema adultorum of Buschke.
Case Reports
Case 1
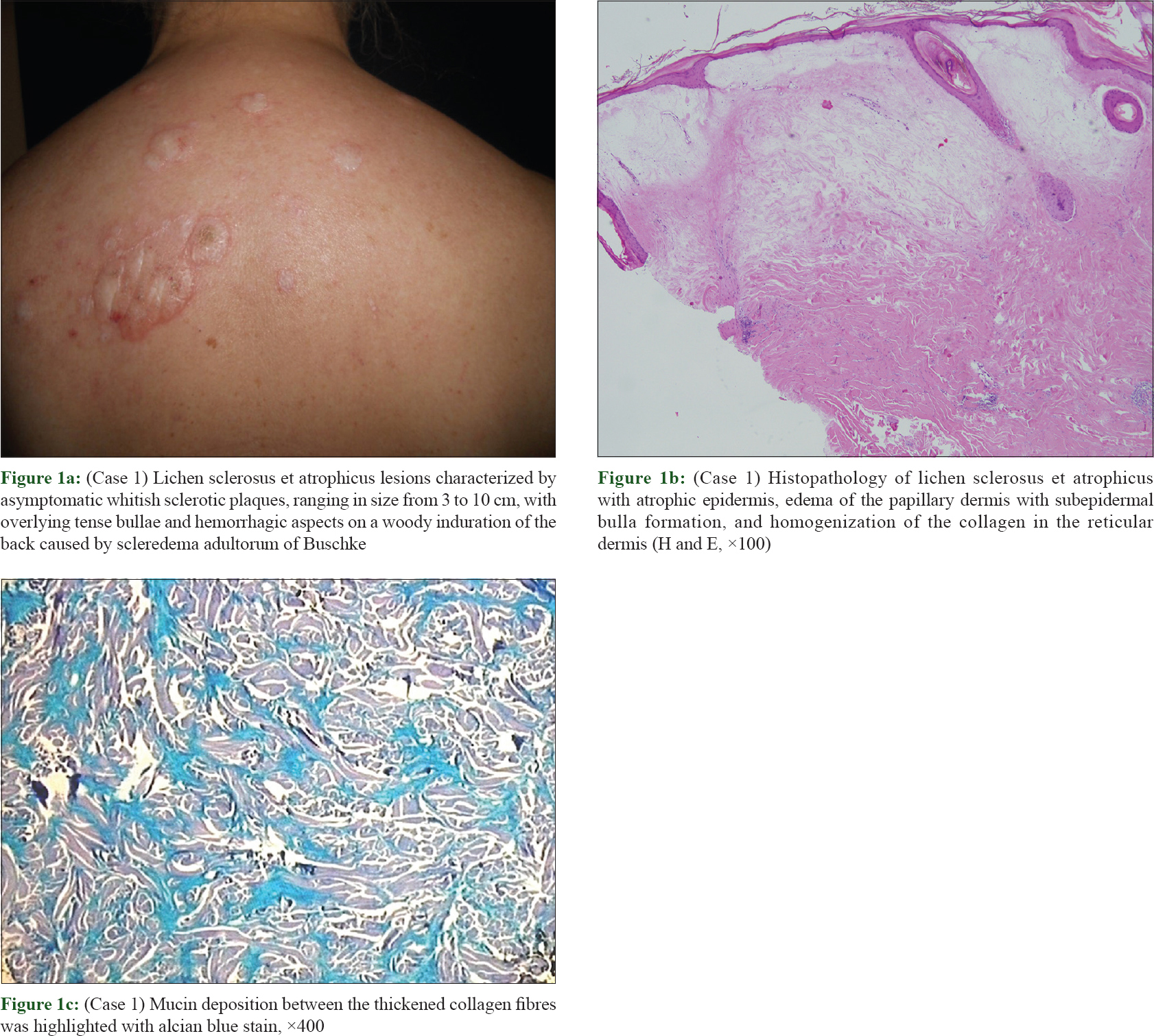
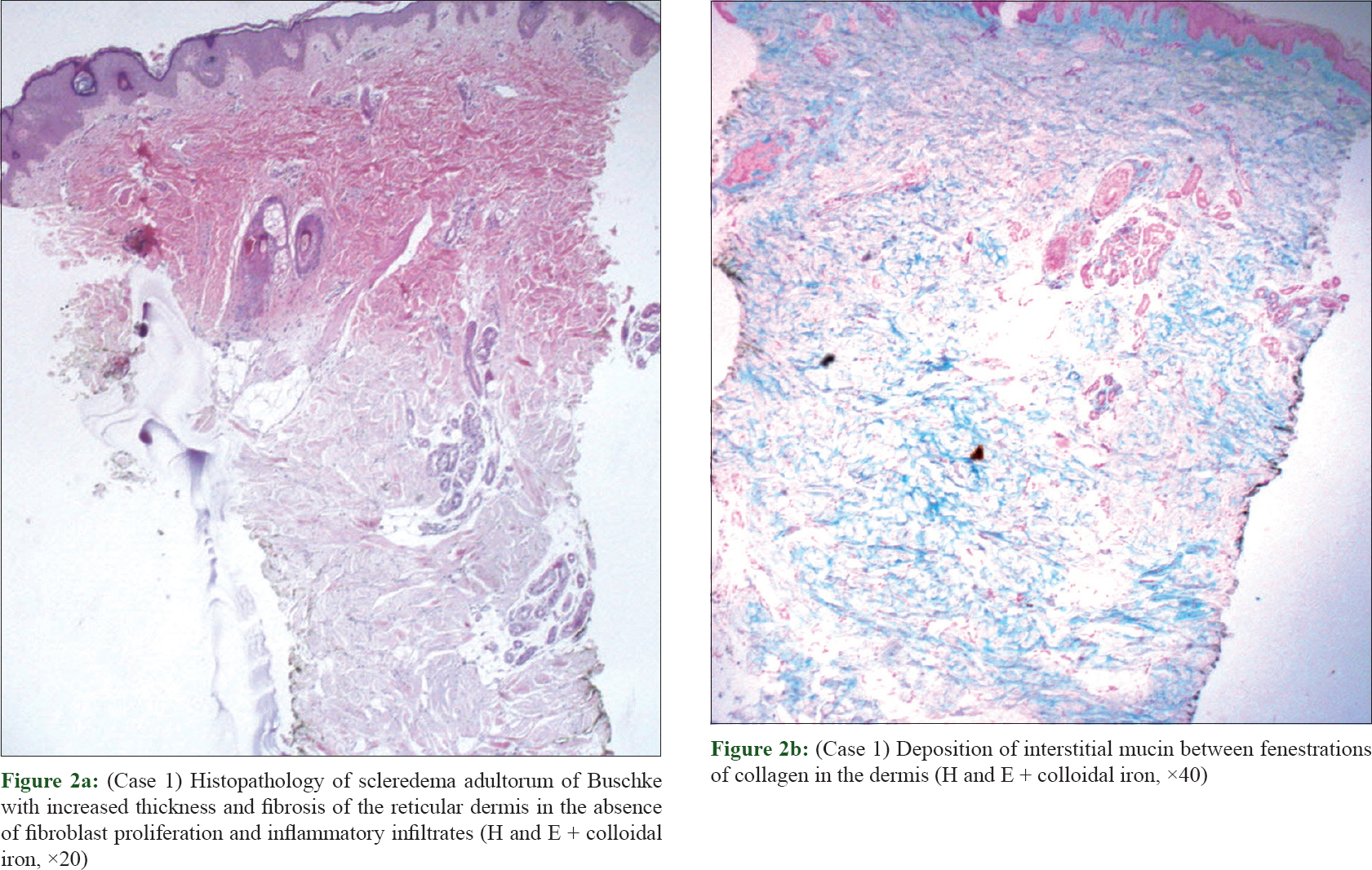
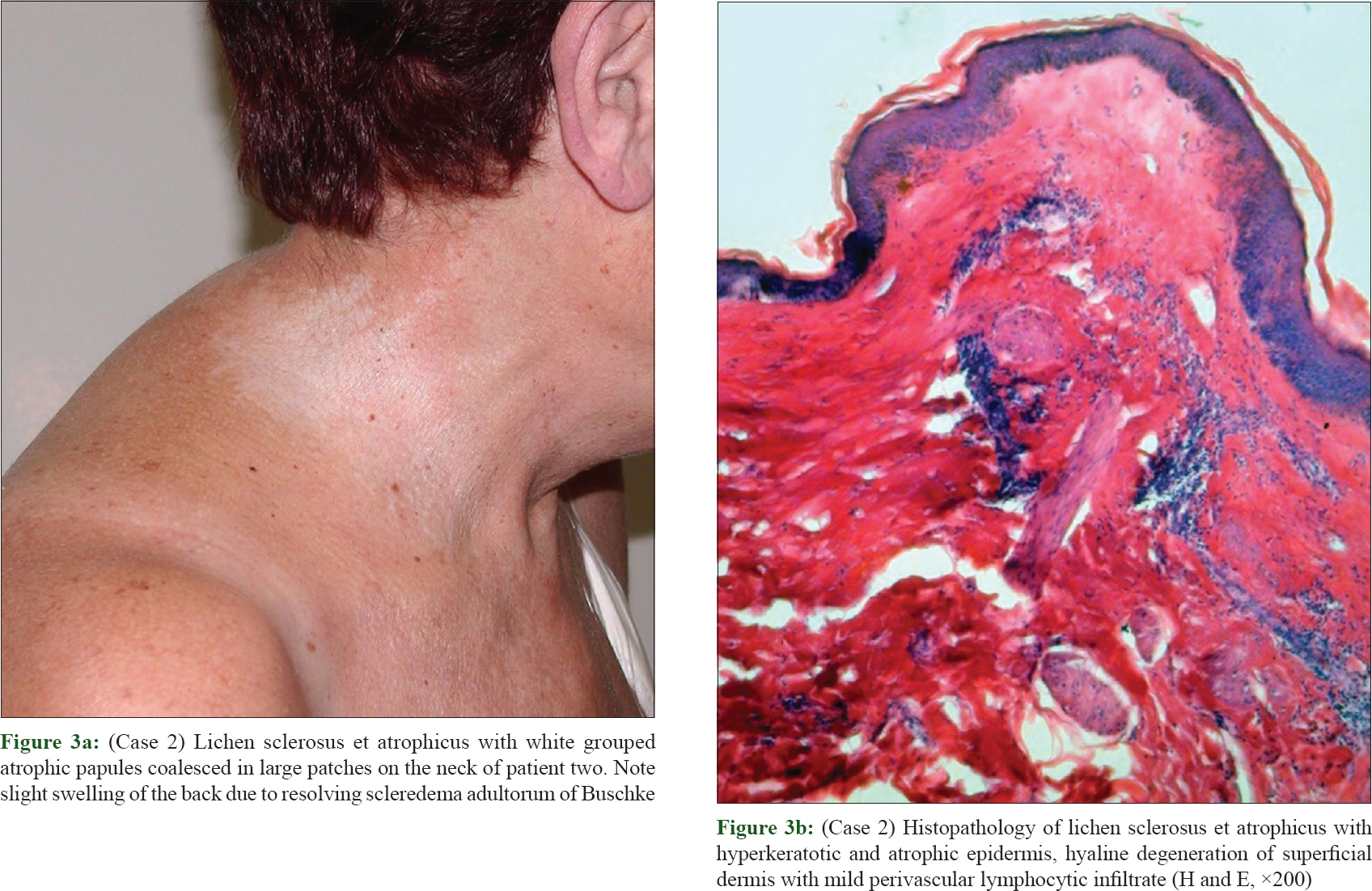
A 59-year-old woman presented with an 11-month history of asymptomatic whitish plaques with altered texture of the affected skin ranging in size from 3 to 10 cm, with overlying tense bullae, sometimes hemorrhagic, on her back [Figure - 1]a in the context of scleredema adultorum of Buschke lesions. Indeed, her torso and neck were also characterized by tightening, thickening and hardening of skin for 4 years previously diagnosed as scleredema adultorum of Buschke (supported by a histopathological evaluation reports with an increased thickness of the dermis with deposition of interstitial mucin, stained positively with colloidal iron, between fenestrations of collagen in the absence of inflammatory infiltrate [Figure - 2]a, [Figure - 2]b and [Table - 1]).
 |
| Figure 1: |
 |
| Figure 2: |
Her medical history was also relevant for a diabetes type II with metabolic syndrome for many years.
Serologic analysis were notable for positive antinuclear antibody titer 1:80 (not significant) and positive antithyroid autoantibodies. A biopsy specimen showed orthohyperkeratosis, epidermal atrophy, follicular hyperkeratosis, marked edema in the papillary dermis with subepidermal bulla formation and a slight underlying perivascular lymphocytic infiltrate with homogenization of the collagen throughout the reticular dermis [Figure - 1]b. Mucin deposition between the thickened collagen fibres was highlighted with alcian blue stain [Figure - 1]c. Direct immunofluorescence was negative. This picture was consistent with scleredema adultorum of Buschke with an overlying bullous lichen sclerosus et atrophicus, excluding an eczema or a bullosis diabeticorum because of the clinical and peculiar pathological features.
Topical clobetasol propionate 0.05% gave poor results and the addition of tacrolimus ointment resulted in a slight improvement.
Case 2 and case 3
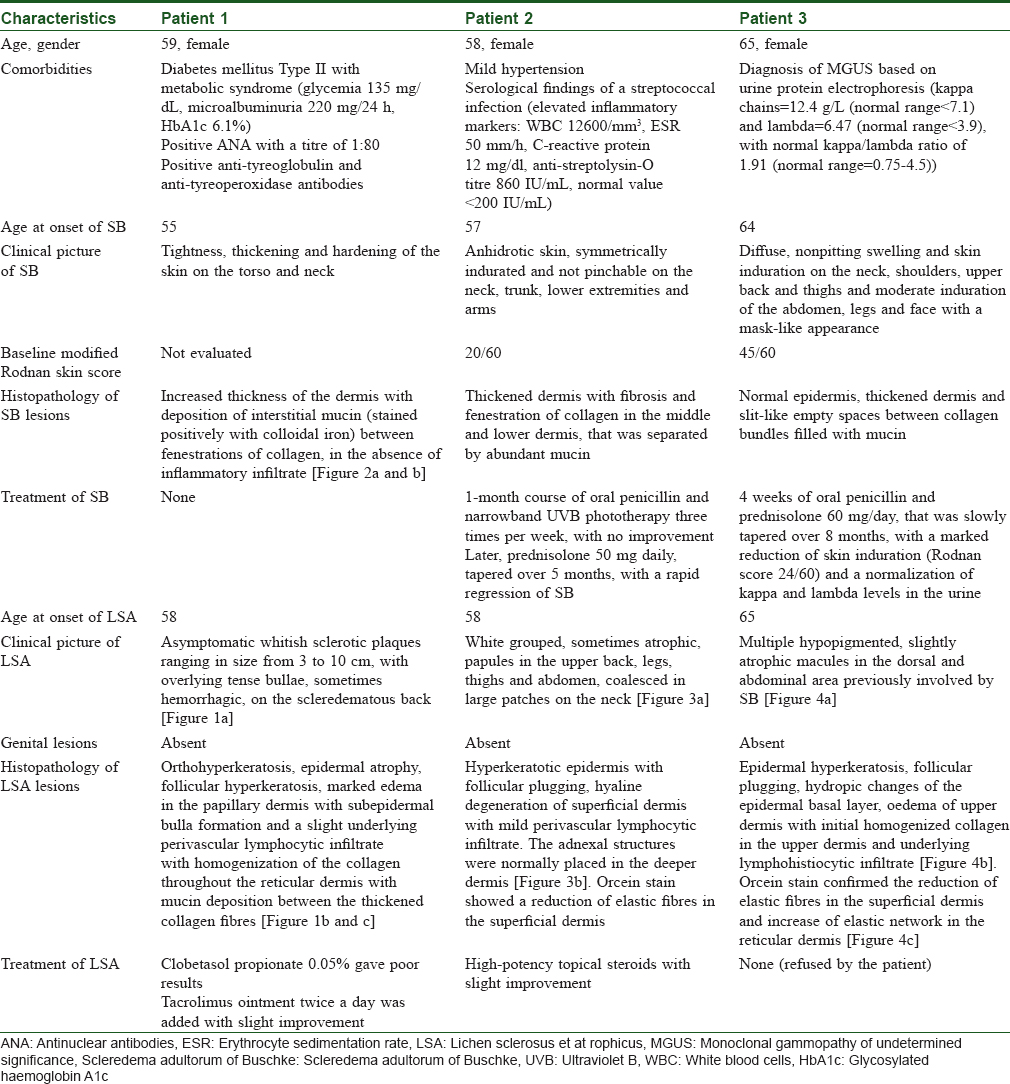
A 58 -year-old female, diagnosed with a post-streptococcal Scleredema adultorum of Buschke of the neck, shoulders, trunk, lower extremities and arms, developed six months later (during the regression of the skin thickening) white grouped, sometimes atrophic, papules onher upper back, involving also the legs, thighs and abdomen, coalesced in large patches on the neck, pathologically consistent with lichen sclerosus et atrophicus [Figure - 3]a, [Figure - 3]b and [Table - 1].
 |
| Figure 3: |
A 65-year-old woman, with a previous diagnosis of scleredema adultorum of Buschke of the neck, face, shoulders, upper back, abdomen and lower limbs associated with a monoclonal gammopathy of undetermined significance, presented with multiple hypopigmented, slightly atrophic macules in the dorsal area previously involved by scleredema adultorum of Buschke, finally recognized as lichen sclerosus et atrophicus at the histopathological examination [Figure - 4]a, [Figure - 4]b, [Figure - 4]c and [Table - 1].
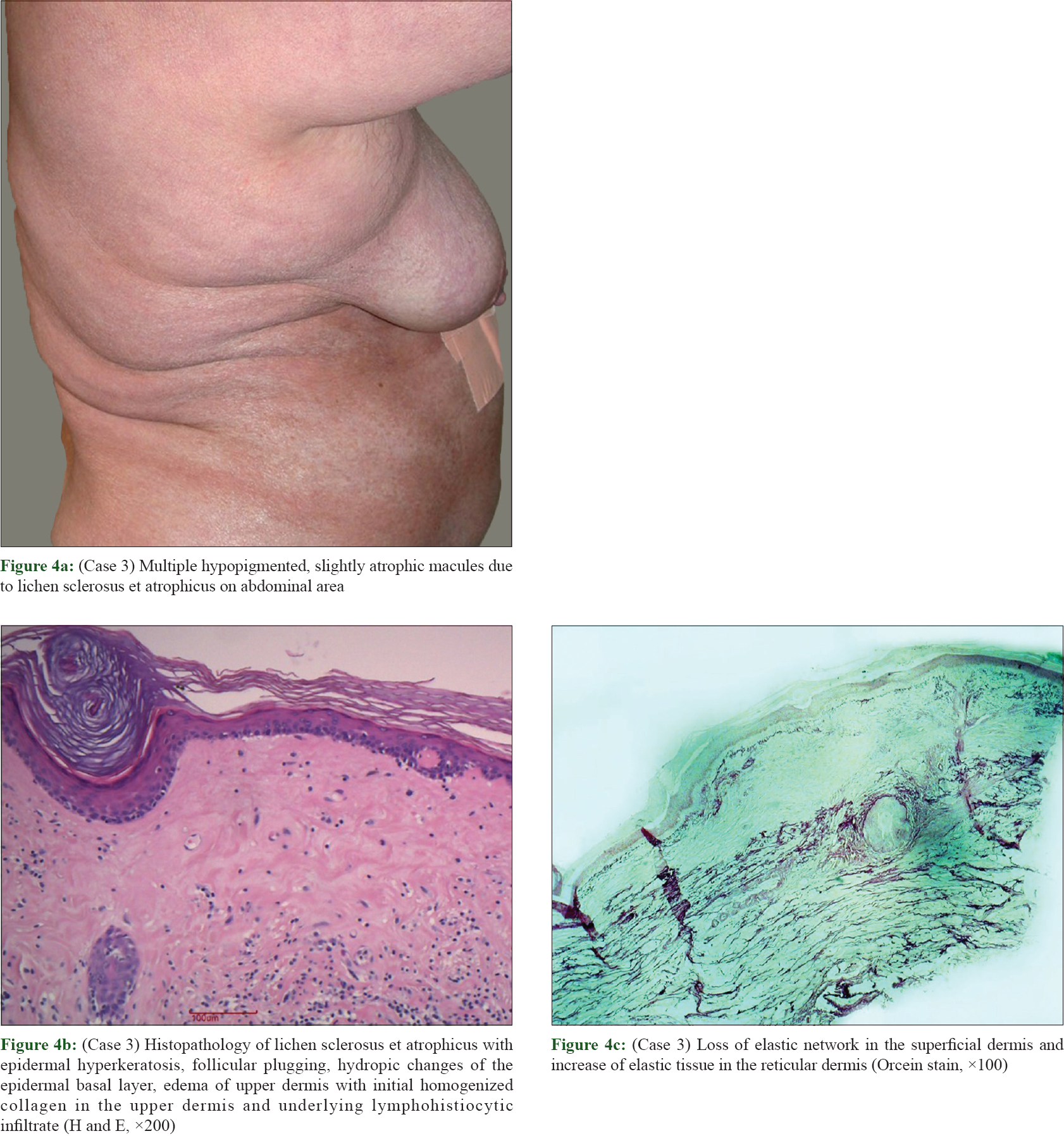 |
| Figure 4: |
Discussion
The pathogenesis of scleredema adultorum of Buschke and lichen sclerosus et atrophicus is not well understood. In scleredema adultorum of Buschke, an increased synthesis of type I collagen by dysfunctional fibroblasts has been demonstrated in the affected skin.[1] In diabetic scleredema adultorum of Buschke, the accumulation of collagen may be due to irreversible nonenzymatic glycosylation of collagen and resistance to degradation by collagenase.[6] An autoimmune basis has been also proposed for bulla formation in lichen sclerosus et atrophicus, although this may also be related to vacuolar degeneration of basal layer leading to instability of basement membrane zone, or linked to papillary dermal edema disrupting the collagen fibres.[5]
Moreover, in lichen sclerosus et atrophicus, an alteration in the expression of both connective tissue growth factors and extracellular matrix proteins (e.g., increased glycosaminoglycans as hyaluron acid) has been demonstrated with the presence of autoantibodies against the extracellular matrix protein 1 (ECM-1) itself, involving molecules such as perlecan, type IV collagen, dystroglycan, fibroblast growth factor 7 and fibroblast-growth-factor-binding protein.[5] Hence, an immunoreactivity against the same molecules could probably be involved in the pathogenesis of scleredema adultorum of Buschke, in which the activation of fibroblasts is a typical finding, producing increased amount of collagen and mucin.
Our patients [Table - 1], all women, the first with diabetes and an antithyroid autoantibody profile, the second with a possible post streptococcal immunological antigen cross-reaction and the third with a monoclonal gammopathy of undetermined significance, reinforce the hypothesis of a common underlying disorder of the immune system.
Diabetes is another potential common feature because lichen sclerosus et atrophicus has been associated with glucose intolerance or diabetes mellitus.[7]
Furthermore, lichen sclerosus et atrophicus has been found in combination with other sclerodermiform diseases such as sclerodermatous chronic graft-versus-host disease[8] or bullous morphea.[9] Nevertheless, these conditions have been also considered different clinical manifestations of the spectrum of a single disease, labelled as lichen sclerosus et atrophicus-like variant of bullous morphoea (due mainly to local trauma and inflammation) which is different from the bullous lymphangiectatic form of morphoea linked to dermal scarring.[9] Hence, a plausible explanation for the coexistence of lichen sclerosus et atrophicus features and morphea could be that lichen sclerosus et atrophicus superficial changes are due to a lymphatic obstruction related to the underlying sclerodermatous dermal process.[9] The same pathogenetic mechanism of dermal sclerosis with lymphatic compression could also play a role in the development of lichen sclerosus et atrophicus superimposed on previous underlying dermal modifications of scleredema adultorum of Buschke in our cases.
Finally, the occurrence of lichen sclerosus et atrophicus in the site of regressed scleredema adultorum of Buschke, as in our case 3, could be due to an isotopic reaction that has been demonstrated for lichen sclerosus et atrophicus at the site of a herpes zoster scar.[10] Anyway, this common localization could involve a Koebner phenomenon as well that has been reported either for scleredema adultorum of Buschke and for lichen sclerosus et atrophicus and in its bullous form.[1] Koebnerization for lichen sclerosus et atrophicus has been described in skin already scarred or damaged because of UV radiation, ionizing radiation, burns, varicose veins, vulvo-vaginitis, pellagra, vaccines, repeated pressure, friction from clothing, trauma and surgical scars.[7]
In conclusion, our cases highlight the new association of two sclerodermiform skin conditions such as scleredema adultorum of Buschke and lichen sclerosus et atrophicus with its bullous variant. These findings could be purely coincidental, but their occurrence at the same site and in close time relationship make us wonder if the two diseases could be a part of the spectrum of a single disorder and whether there could be some common underlying pathogenetic mechanisms directing the coexistence of both disorders.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Rongioletti F, Kaiser F, Cinotti E, Metze D, Battistella M, Calzavara-Pinton PG, et al. Scleredema. A multicentre study of characteristics, comorbidities, course and therapy in 44 patients. J Eur Acad Dermatol Venereol 2015;29:2399-404.
[Google Scholar]
|
| 2. |
Dumke AK, Tittelbach J, Elsner P. Scleredema adultorum Buschke and exulcerated necrobiosis lipoidica in diabetes mellitus type 1. Dtsch Med Wochenschr 2014;139:2184-7.
[Google Scholar]
|
| 3. |
Yachoui R, Traisak P, Jagga S. Scleredema in a patient with AIDS-related lipodystrophy syndrome. Case Rep Endocrinol 2013;2013:943798.
[Google Scholar]
|
| 4. |
Mylona E, Golfinopoulou S, Skarmea A, Katsikas G, Skrepetou K, Nakos G, et al. Post-radiation scleredema adultorum and diffuse eosinophilic fasciitis in the same patient. Scand J Rheumatol 2011;40:240-1.
[Google Scholar]
|
| 5. |
Sauder MB, Linzon-Smith J, Beecker J. Extragenital bullous lichen sclerosus. J Am Acad Dermatol 2014;71:981-4.
[Google Scholar]
|
| 6. |
Martín C, Requena L, Manrique K, Manzarbeitia FD, Rovira A. Scleredema diabeticorum in a patient with type 2 diabetes mellitus. Case Rep Endocrinol 2011;2011:560273.
[Google Scholar]
|
| 7. |
Monteagudo B, Cabanillas M, Bellido D, Suárez-Amor O, Ramírez-Santos A, de la Cruz A. Lichen sclerosus atrophicus at an insulin injection site: An unusual koebner phenomenon. Actas Dermosifiliogr 2010;101:563-5.
[Google Scholar]
|
| 8. |
Kung EF, Soltani K, Petronic-Rosic V. Clinicopathologic challenge. Sclerodermoid graft-versus-host disease (GVHD) with lichensclerosus-like lesions. Int J Dermatol 2008;47:655-7.
[Google Scholar]
|
| 9. |
Venturi M, Pinna AL, Pilloni L, Atzori L, Ferreli C, Rongioletti F. Bullous morphoea: A retrospective study. Clin Exp Dermatol 2017;42:532-5.
[Google Scholar]
|
| 10. |
Forschner A, Metzler G, Rassner G, Fierlbeck G. Morphea with features of lichen sclerosus et atrophicus at the site of a herpes zoster scar: Another case of an isotopic response. Int J Dermatol 2005;44:524-5.
[Google Scholar]
|
Fulltext Views
4,914
PDF downloads
2,652





