Translate this page into:
Scleromyxedema: A rare case report with dermoscopic findings
Corresponding author: Dr. Arjun Prakashey, Department of Dermatology, Government Medical College, Bhavnagar, Gujarat, India. arjun.24jan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Prakashey A, Mehta H, Bharti AH, Agharia R. Scleromyxedema: A rare case report with dermoscopic findings. Indian J Dermatol Venereol Leprol. 2024;90:96-8. doi: 10.25259/IJDVL_740_2022
Dear Editor,
Cutaneous mucinosis is a heterogenous group of disorders which are characterised by an abnormal mucin deposition in skin. Scleromyxedema, also known as generalised papular and sclerodermoid lichen myxedematosus, is a cutaneous mucinosis characterised by a generalised papular and sclerodermoid eruption, a triad of increased fibroblast proliferation, mucin deposition and fibrosis. Monoclonal gammopathy is commonly associated.
A 50-year-old Indian male presented with an insidious onset and gradually progressive eruption of erythematous papules associated with thickening of skin primarily over the face and a tender swelling in the central aspect of the face. The patient did not have a history of any systemic disease, nor did he have any other systemic complaints on enquiry.
On cutaneous examination, the patient had a diffuse erythematous, mildly edematous, tender plaque on centrofacial area involving the glabella, and root of the nose giving rise to leonine facies [Figure 1a]. The chin also had a diffuse infiltration with shiny surface and a background yellowish hue. There was infiltration and thickning of both ears with a shiny appearance of the overlying skin. Additionally, there were sheets of firm, waxy, lichenoid to brownish papules, with few making linear configuration over the back of the neck, trunk, and proximal extremities [Figures 1b and 1c]. Increased furrowing of skin on the back (Shar-Pei Sign) and abdominal areas was noted. Both proximal interphalangeal joints had tightening of skin with central depression and an elevated rim (doughnut sign).

- Centrofacial erythematous plaque with infiltration of forehead with glabella (leonine facies) and chin.

- Papular eruption over the back with furrowing of creases visible on lower back (Shar-Pei sign).

- Central depression over proximal interphalangeal joint with elevated rim (doughnut sign).
Dermoscopic examination of the glabella (Dermlite DL4 dermatoscope–3 Gen Inc., San Juan Capistrano, CA, USA–×10 magnification, polarised mode) [Figure 2] revealed localised yellowish brown and yellowish white roundish structureless areas with interspersed linear irregular vessels and few out of focus vessels and accentuated pigmentary network at few areas. There was a relative alopecia with vellus hair showing peripilar scales and few white and black dots.
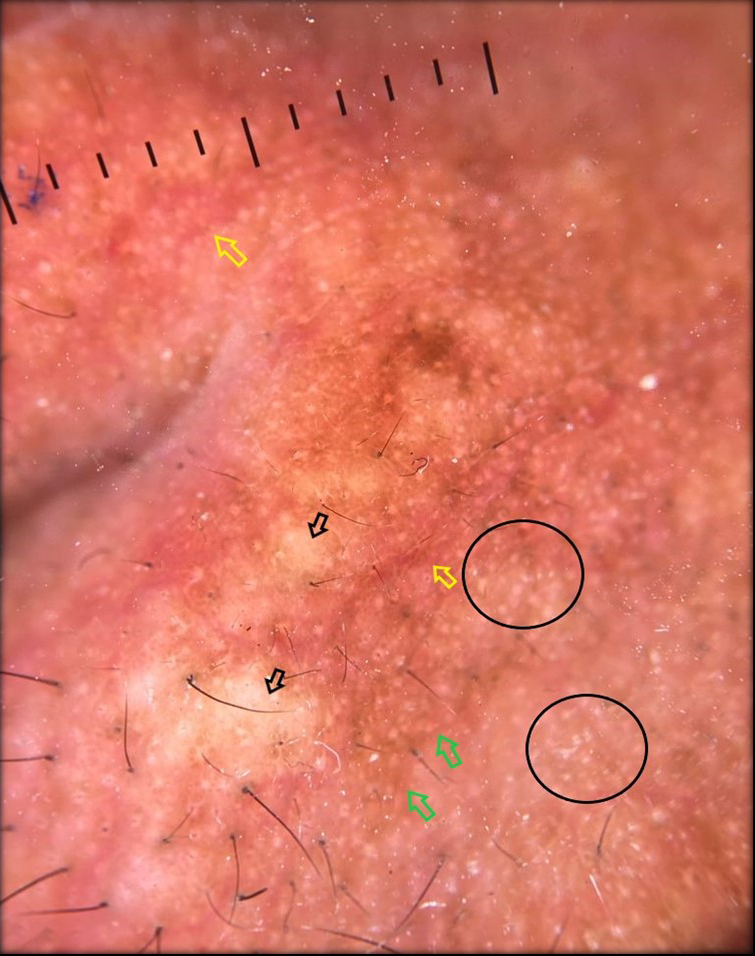
- Dermoscopy of the glabella showing localised yellowish brown and yellowish white structureless area (black arrow), ill focused linear irregular vessels (yellow arrow) accentuated pigmentary network (green arrow), clustered whitish round homogenous areas leading to sago grain like appearanced due to eccrine openings (black circles).
Dermoscopy of lesion on neck [Figure 3] showed glistening yellowish white round to oval areas with loss of pigmentary network (few coalescing into a linear array with accentuation of pigmentation in the periphery).
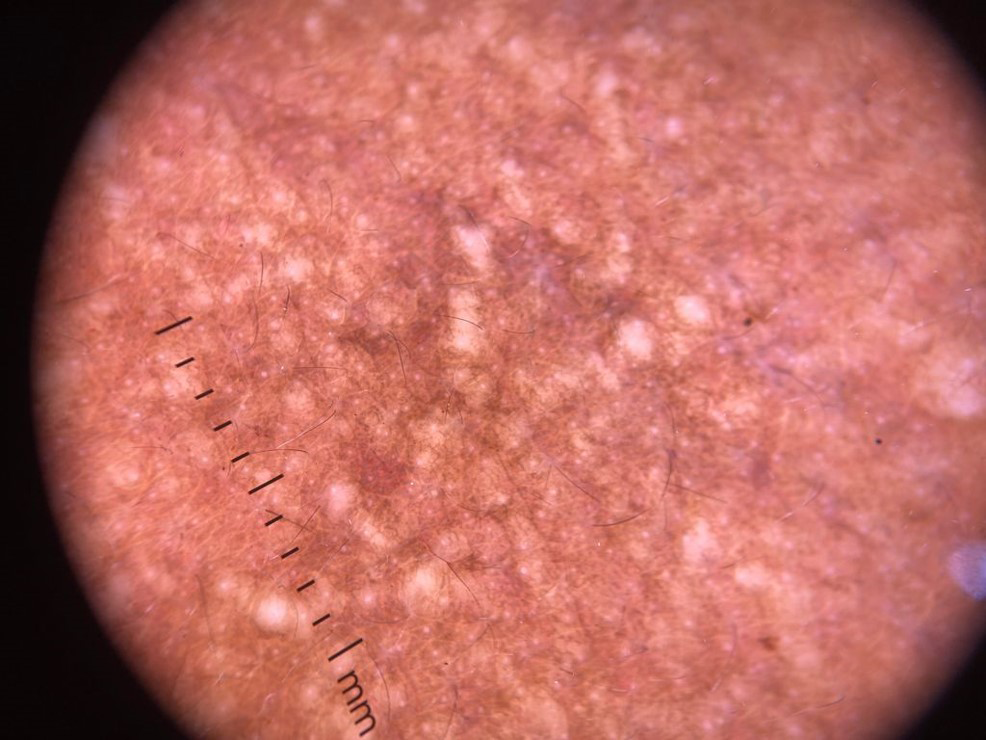
- Dermoscopy from papular lesions over the neck showing glistening yellowish white, round to oval areas (coalescence into a linear array is prominent with accentuation of pigmentation in the periphery).

- Dermoscopy from papular lesions over the neck showing glistening yellowish white, round to oval areas (coalescence into a linear array is prominent with accentuation of pigmentation in the periphery).
Systemic examination of the patient including the sensorimotor examination was normal.
Serum protein electrophoresis with immunofixation showed an IgG monoclonal gammopathy. Chest X-ray showed mediastinal lymph node enlargement. Spirometry revealed a mild (30–50%) restrictive pattern but high resolution commuted tomography (HRCT) of chest did not show any fibrotic changes. Electrocardiogram was low voltage with a mild left axis deviation.
Histopathological examination of the glabellar skin was suggestive of scleromyxedema, as shown [Figures 4a and 4b].

- White arrow displays epidermal acanthosis and hyprpigmentation of the basal layer which corresponds to the accentuation of pigment network. The red arrow displays presence of dilated capillaries which correspond dermoscopically to the telangiectasia and linear curved vessels. The yellow arrows suggest areas of deposition of mucinous material. (Haematoxylin and eosin stain, × 10 magnification).

- There is presence of fibroplasia and bluish material in the mid and deep dermis denoted by yellow arrows, which on alcian blue stain displays bluish discoloration suggestive of mucin depositions. (Alcian blue stain at pH 2.5, × 10 magnification).
On the basis of the above findings, a provisional diagnosis of scleromyxedema was considered. Opinion from a hemato-oncologist as well as a rheumatologist was sought and the patient was advised a bone marrow aspiration and biopsy.
Strikingly, our patient did not show any signs or symptoms of systemic involvement at the time of diagnosis, but long term follow-up is still essential.
Previously, Mendes Bastos P et al. had described clusters of round white-ivory homogenous areas resembling rice grains, which they reported to correlate well to dermal fibroblast proliferation and collagen accumulation.1 Dermoscopically, we were also able to notice yellowish-white round structureless areas which seem to correlate well with mucin deposition on histopathology along with pigmentary and vascular changes [Table 1].
Sr
Dermoscopy
Histopathology
1
Yellowish white structureless areas.
Interstitial fibrosis and mucin deposition.
2
Linear and irregular vessels.
Dilated capillary in the papillary dermis.
3
Accentuated pigmentary network.
Irregular epidermal acanthosis and basal layer hypermelanisation.
4
Erythema in the periphery.
Superficial peri vascular, peri appendageal infiltrate.
Scleromyxedema is a chronic and unpredictable disease associated with monoclonal gammopathy and severe systemic implications including neurologic, haematologic and cardiologic involvement leading to a guarded prognosis. However, our patient had no clinically evident systemic involvement with presence of classic cutaneous lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Dermoscopy and reflectance confocal microscopy for the diagnosis of scleromyxedema. JAAD Case Rep. 2019;5:451-3.
- [CrossRef] [Google Scholar]





