Translate this page into:
Sclerotherapy in the management of varicose veins and its dermatological complications
2 Department of DVL, Bangalore Medical College and Research Institute, Bangalore, Karnataka, India
Correspondence Address:
Nagesh T Subbarao
Department of DVL, Sapthagiri Institute of Medical Sciences and Research Center, Chikkasandra, Hesaraghatta Main Road, Bangalore, Karnataka
India
| How to cite this article: Subbarao NT, Aradhya SS, Veerabhadrappa NH. Sclerotherapy in the management of varicose veins and its dermatological complications. Indian J Dermatol Venereol Leprol 2013;79:383-388 |
Abstract
Background: Varicose veins and its dermatological complications like stasis dermatitis, ulcers, spontaneous bleeding are commonly seen in the dermatology clinics. Surgery has been the most often used treatment for varicose veins. Sclerotherapy refers to introduction of sclerosing solution into the varicose veins, which causes endothelial damage and subsequent fibrosis. Sclerotherapy is being practised extensively by dermatosurgeons in the west. However, there are no Indian studies which specifically evaluate the role of sclerotherapy in the management of varicose veins and its skin complications. Hence, this study aims to evaluate the efficacy of sclerotherapy in managing varicose veins and its complications. Aims: To study the safety and efficacy of sclerotherapy in the treatment of varicose veins and its dermatological complications. Methods: This is a prospective study involving 50 patients with varicose veins and its dermatological complications attending the dermatology out-patient department. The study was conducted over a period of 18 months. After thorough clinical, laboratory, and radiological evaluation, the patients were treated with sclerotherapy using Sodium Tetradecyl Sulphate of various concentrations depending on the vessel size. The patients were then followed up to look for disappearance of veins, healing of ulcers and eczema, and any complications.Results: Patients showed a good response to treatment with sclerotherapy. 70-80% of patients showed symptomatic improvement along with disappearance of veins and healing of eczema and ulcers. Most of the complications were minor, which resolved over a period of few weeks. Conclusion : Sclerotherapy is a simple, safe and effective procedure for the treatment of varicose veins and its dermatological complications. The procedure is particularly effective for smaller, early varicosities and also for residual veins after surgery. Hence we recommend more and more of our fellow dermatologists to take up this procedure, which can be an efficient tool to manage patients with varicose veins and its related complications.Introduction
Varicose veins can be defined as: superficial veins of the lower limb, which have permanently lost its valvular efficiency and as a product of resultant venous hypertension in the standing position become dilated, tortuous, and thickened. [1] About 17-50% of patients with varicose veins may have cutaneous findings. [2] Varicose veins may cause significant morbidity including stasis dermatitis, ankle oedema, spontaneous bleeding, superficial thrombophlebitis, recurrent cellulitis, lipodermatosclerosis and ulceration of the ankle and foot. [3] Varicose veins and its related complications are commonly seen in the dermatology clinics.
The various modalities to treat varicose veins include surgery (stripping, ambulatory phlebectomy, high ligation), sclerotherapy and endo-venous occlusion by lasers or radiofrequency. The indications for any of the treatments of varicose veins include: (a) prevention of complications; (b) relief of symptoms; and (c) improvement of cosmetic appearance. [4]
Sclerotherapy refers to the introduction of a sclerosing solution into the lumen of a vessel producing endothelial damage, which leads to thrombosis and subsequent fibrosis. It has been extensively used by dermato-surgeons in the management of superficial varicose veins and other venous abnormalities. [5] However, it has not been widely practiced in India. The search for more effective means of prevention and treating varicose veins and its complications continues and this study aims at establishing the role and efficacy of sclerotherapy in managing varicose veins and its dermatological complications.
Methods
The study included 50 patients who presented with symptoms of primary varicose veins and its dermatological complications. The study was taken up after the clearance from ethics committee and it extended over a period of 18 months from December 2006 to August 2008.
After obtaining adequate history, the patients were meticulously examined in standing position with good illumination to look for the varicose veins. Later the patients underwent venous doppler and were evaluated specifically for (a) sapheno-femoral junction incompetence; (b) sapheno-popliteal junction incompetence; (c) perforator incompetence; (d) deep venous system; and (e) presence of abnormal or unnamed veins or perforators [Figure - 1].
 |
| Figure 1: Stasis ulcer with marking of perforators during venous Doppler |
Patients having sapheno-femoral and sapheno-popliteal incompetence were referred to the department of surgery to undergo high ligation and were then taken up for sclerotherapy.
Inclusion criteria
The inclusion criteria for the study was patients older than 18 years with varicose, reticular and/or telangiectatic leg veins and having skin manifestations of varicose veins like eczema, ulceration, lipodermatosclerosis, etc.
Exclusion criteria
The various exclusion criteria for the study were (a) deep venous thrombosis; (b) saphenofemoral junction/saphenopopliteal junction incompetence; (c) pregnancy; (d) myocardial decompensation; (e) hypercoagulable state; (f) dependency edema; (g) arterial disease; (h) diabetes mellitus; and (i) any other serious illness.
The following investigations were carried out before the procedure: (a) Complete hemogram; (b) Random blood sugar; (c) Coagulation profile; (d) Urine-albumin, sugar and microscopy; and (e) Venous doppler of involved limb.
Procedure
The procedure involved injection of appropriate amount of Sodium Tetradecyl Sulphate (STS) in appropriate concentrations into the required vein under aseptic precautions [Figure - 2]. Fegan′s technique was used for injecting the sclerosant. [2] The patient was made to sit with the leg to be treated in the dependent position. The vein was cannulated with a needle and the leg was elevated and supported over the table to allow drainage of blood. A small amount of blood was withdrawn into the syringe before injection to ensure that needle remains in the varicosity lumen. Approximately 0.5-1 ml of sclerosant would be injected at each site. Finger pressure was applied several centimeters above and below the injection point and maintained for 60 s followed by immediate application of compression. The procedure was done in the dermato-surgery operation theatre. The sclerosant concentration was decided depending on the size of veins. The sclerosant was diluted to required concentrations using 0.9% normal saline. [6] Commonly used concentrations were 0.3-0.5% of STS depending on the size of the veins. 0.75% STS was used to inject the perforators [Table - 1]. Not more than 1 ml was injected at each site and maximum of five injections were given at each session using 1 ml syringes.
 |
| Figure 2: Position of hand while injecting |

Elastic compression bandage was applied after injecting the sclerosant. The patient was advised to use the compression bandage for the next 3 months.
The procedure was done in multiple sessions (4-6) with a gap of 3-4 weeks between the sessions.
Follow-up
All patients were observed for 1 h after the procedure to look for any evidence of allergic reactions (analphylaxis) and sent home on the same day. They were asked to review after 3 days in case of any adverse events at the site of injecting the sclerosant. They were all followed-up for a minimum of 6 months after the procedure and the response was evaluated by two doctors independently to look for: (a) Symptomatic relief; (b) Recurrence of varicosity; (c) Healing of venous ulcers; (d) Response of eczema; (e) Pigmentation; and (f) Reduction of edema.
Results
The study included 50 patients with primary varicose veins and its complications. In the study out of 50 patients, maximum number of patients, 20 (40%) were in the 31-40 years age group followed by 16 (32%) patients in the 41-50 years age group, next followed by 51-60 years age group and the least being in 20-30 years age group with 8% of patients.
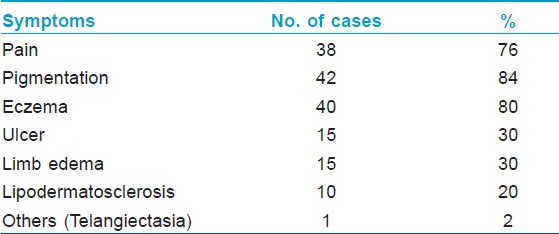
Out of the 50 cases included in the study, 30 (60%) cases were male with only 20 (40%) female patients. In the present study, the commonest presentation was that of dilated and tortuous veins. The other symptoms were (a) pain in the affected limb - 38 patients (76%); (b) eczema - 40 patients (80%); (c) oedema - 15 patients (30%); (d) ulceration - 15 patients (30%); (e) lipodermatosclerosis - 10 cases (20%); and (f) telangiectasia and atrophie blanche - 2 cases (4%) [Table - 2].
Therapeutic results
As a good result we considered disappearance of varices and eczema, reduction of edema, healed ulcers and relief of symptoms (pain, fatigue, tiredness). No concomitant local medications were used for venous ulcers. The response is based on the clinical findings of basic signs of varicose veins.
Pain improved in 29 patients out of 38 cases (76%), dilated veins reduced in 45 (90%) out of 50 cases, oedema reduced in 7 of 15 patients (46%), ulceration reduced in 10 (66%), pigmentation responded poorly with 8 cases showing response out of 42 cases, eczema showed a good response with 33 (82.5%) out of 40 patients showing improvement and lipodermatosclerosis responded poorly with 2 out of 10 patients showing improvement. ([Table - 3], [Figure - 3], [Figure - 4], [Figure - 5], [Figure - 6]
 |
| Figure 3: (a and b) Dilated veins before and after sclerotherapy |
 |
| Figure 4: (a and b) Ulcer before and after treatment |
 |
| Figure 5: (a and b) Eczema and pigmentation before and after treatment |
 |
| Figure 6: (a and b) Dilated veins before and after sclerotherapy |

Complications
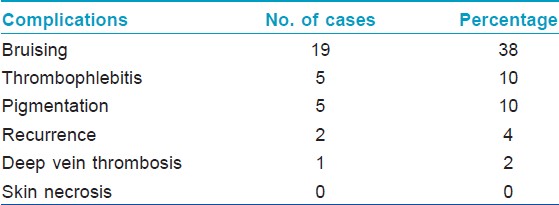
Pain and bruising at the site of injection was the most common complication seen in 19 (38%) patients followed by phlebitis in 5 (10%) cases, pigmentation was seen in 5 (10%) cases, and deep vein thrombosis (DVT) was noted in a patient (2%) [Table - 4]. There were no episodes of skin necrosis and anaphylaxis. However, most of the complications resolved over a period of few weeks, with pigmentation taking a longer time to resolve.
Discussion
The etiology of varicose veins is multi-factorial and all treatments presently available including, surgery and sclerotherapy are palliative and not etiological. [7] Varicose veins with its dermatological complications are commonly seen in the dermatology OPD (out patient department). Surgical procedures like ligation and stripping are the preferred modalities of treatment. Sclerotherapy is a valuable method of treatment for varicose veins of the lower limb and is one of the frequently used procedures by Dermatologists in the west. [2],[8] However, on extensive review of literature, there are no Indian studies which have specifically evaluated the role of sclerotherapy in the management of varicose veins and its complications.
Sclerotherapy is the injection of a chemical solution (sclerosant) into a vein, damaging the endothelial lining and causing vessel occlusion and the development of fibrous tissue. [9] The objective of sclerotherapy is not only to produce complete endothelial damage and subsequent fibrosis of the entire vein wall without recanalization, but also to locate the points of abnormal flow from the deep to the superficial veins and must be permanently obliterated by the injection of a sclerosant. With this, the secondary incompetent but not permanently damaged valves can regain their normal functions. The most important aspect of treatment is to diminish local venous hypertension by interrupting the leaking points via perforating veins into the superficial network. The migration of the sclerosing solution in isolated segments (digital compression) of injected superficial vein can reliably close the perforator complex of perforators. Localization of incompetent perforating veins by this technique could yield a perfect result in 90 out of 100 patients. The incompetent perforators are almost always found near the skin changes and in typical places in the legs (Cockett, Boyd, Dodd). [7]
Sclerosing solutions are classified into three groups, based on the mechanism of action; detergent agents, osmotic agents and chemical irritants. The various sclerosants include STS, polidocanol, hypertonic saline, sodium morrhuate, etc. STS, a detergent sclerosant was used in our study. It causes destruction of endothelium by altering the surface tension around the endothelial cells by a process known as protein theft mechanism. [10]
A study conducted by Fun on the etiology and symptomatology of varicose veins of lower limbs has shown patients having pain in 59%, pigmentation in 58%, edema in 53%, eczema in 29%, ulceration in 28%, bleeding in 21% and lipodermatosclerosis in 20%. [11] Hence our study correlates well with the above study except for pigmentation, eczema and varicosity. This disparity is because the above study was an epidemiological study and our study is a therapeutic study conducted mainly on patients with dermatological complications of varicose veins. Hence presence of eczema and pigmentation was more in our study.
According to a study conducted by Labas et al. on the results of compression sclerotherapy, 78% of patients showed improvement in pain, 83% showed disappearance of varices, 72% showed reduction of edema, 80% showed improvement in eczema, 94% showed healed ulcers. [7] A study conducted by Kahle et al. has shown 76.8% improvement in the disappearance of varicose veins. [12] Cabrera et al. have reported complete healing of venous ulcers in 83% of patients. [13] Hence the results of our study correlate well with the above studies.
The common complications reported by Labas et al. in their study include pigmentation in 12%, local necrosis in 7% and DVT in 0.01% of patients. [7] According to a study by Leach and Goldman, bruising was seen in 54% of patients, pain in 15% of patients. [14] Another study by Goldman has shown ecchymosis in 70%, hyperpigmentation in 64%, vein thrombosis in 46%, local urticaria in 36%, telangiectatic matting in 11% and skin necrosis in 6% of patients. [5] Most of the complications in our study are minor and gradually resolved. Other rare complications reported in the literature include anaphylaxis, extensive tissue necrosis and pulmonary embolism. [15],[16] However, the treating physician should be aware of the early signs of anaphylaxis and should have emergency equipment available. The disparity in percentage of patients having complications like DVT and local necrosis is mainly because of the smaller sample size in our study.
Conclusion
Sclerotherapy is a simple, safe, and effective procedure for the treatment of varicose veins of the lower limb. The procedure is particularly effective for early smaller varicosities, which may help in preventing the development of skin changes and also for residual varicosities after surgery. This being an out-patient procedure, it reduces the cost and morbidity associated with surgical treatment. When the procedure is done with adequate precautions, there are relatively very few complications which are usually minor. Any treatment failures could be most often due to inappropriate technique rather than shortcoming of the procedure. [7] However, further larger Indian studies can be taken up for the evaluation of this technique and also newer advances like ultrasound guided foam sclerotherapy can be incorporated in our practice, which further enhances the efficacy and safety of the procedure. Hence we recommend more and more of our fellow dermatologists to take up this procedure, which can be an efficient tool to manage patients with varicose veins and its related complications.
Acknowledgements
The authors sincerely thank the help and guidance provided by Dr. Dinker B Rai in conducting the study.
| 1. |
Callam MJ. Varicose veins. In: Cuschieri A, Steele RJ, Moossa A, editors. Essential Surgical Practice. 4 th ed. New Delhi: Arnold Publishers; 2002. p. 879-90.
[Google Scholar]
|
| 2. |
Goldman MP, Weiss RA, Bergan JJ. Diagnosis and treatment of varicose veins: A review. J Am Acad Dermatol 1994;31:393-413.
[Google Scholar]
|
| 3. |
Weiss RA, Weiss MA. Treatment of varicose and telangiectatic veins. In: Freedberg JM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's Dermatology in General Medicine. 6 th ed. New York: McGraw Hill publishers; 2003. p. 2549-56
th ed. New York: McGraw Hill publishers; 2003. p. 2549-56'>[Google Scholar]
|
| 4. |
Baccaglini U, Spreafico G, Castoro C, Sorrentino P. Sclerotherapy of varicose veins of the lower limbs. Consensus paper. North American Society of Phlebology. Dermatol Surg 1996;22:883-9.
[Google Scholar]
|
| 5. |
Goldman MP. Treatment of varicose and telangiectatic leg veins: Double-blind prospective comparative trial between aethoxyskerol and sotradecol. Dermatol Surg 2002;28:52-5.
[Google Scholar]
|
| 6. |
Sadick N, Li C. Small-vessel sclerotherapy. Dermatol Clin 2001;19:475-81, viii.
[Google Scholar]
|
| 7. |
Labas P, Ohradka B, Cambal M, Ringelband R. The results of compression sclerotherapy. Phlebologie 2000;29:137-41.
[Google Scholar]
|
| 8. |
Tessari L, Cavezzi A, Frullini A. Preliminary experience with a new sclerosing foam in the treatment of varicose veins. Dermatol Surg 2001;27:58-60.
[Google Scholar]
|
| 9. |
Khunger N, Sacchidanand S. Standard guidelines for care: Sclerotherapy in dermatology. Indian J Dermatol Venereol Leprol 2011;77:222-31.
[Google Scholar]
|
| 10. |
Sacchidanand S, Nagesh TS. Sclerotherapy. In: Venkataram M, editor. ACS (I) Textbook on Cutaneous and Aesthetic Surgery. 1 st ed. New Delhi: Jaypee Medical publishers; 2012. p. 452-62.
[Google Scholar]
|
| 11. |
Fun SK. Varicose veins of the lower limbs: A study of aetiology and symptomatology. Hong Kong Pract 1988;10:3319-26.
[Google Scholar]
|
| 12. |
Kahle B, Leng K. Efficacy of sclerotherapy in varicose veins: Prospective, blinded, placebo-controlled study. Dermatol Surg 2004;30:723-8.
[Google Scholar]
|
| 13. |
Cabrera J, Redondo P, Becerra A, Garrido C, Cabrera J Jr, García-Olmedo MA, et al. Ultrasound-guided injection of polidocanol microfoam in the management of venous leg ulcers. Arch Dermatol 2004;140:667-73.
[Google Scholar]
|
| 14. |
Leach BC, Goldman MP. Comparative trial between sodium tetradecyl sulfate and glycerin in the treatment of telangiectatic leg veins. Dermatol Surg 2003;29:612-4.
[Google Scholar]
|
| 15. |
Bergan JJ, Weiss RA, Goldman MP. Extensive tissue necrosis following high-concentration sclerotherapy for varicose veins. Dermatol Surg 2000;26:535-42.
[Google Scholar]
|
| 16. |
Yamaki T, Nozaki M, Sasaki K. Acute massive pulmonary embolism following high ligation combined with compression sclerotherapy for varicose veins report of a case. Dermatol Surg 1999;25:321-5.
[Google Scholar]
|
Fulltext Views
6,110
PDF downloads
2,557





