Translate this page into:
Scurvy– Once a common condition likely to be missed in the uncommon times!
Corresponding author: Dr. Rachita S Dhurat, Department of Dermatology, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, India. rachitadhurat@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Dhurat RS, Sharma R, Pai SU, Zatakia SM. Scurvy-Once a common condition likely to be missed in the uncommon times! Indian J Dermatol Venereol Leprol. 2025;91:240-2. doi: 10.25259/IJDVL_400_2023
Dear Editor,
Scurvy, a Vitamin C deficiency disorder, has been documented since antiquity. An uncommon disease today, from a dermatological perspective, it can be missed due to subtle clinical signs. Thus one must correlate the characteristic clinico-radiologic findings and etiologic risk-factors for diagnosing scurvy.
A seven-year-old boy was admitted to the paediatric intensive care unit for seizures. The boy was diagnosed with West Syndrome at birth. Within seven days of admission, he developed fever, joint pain, abdominal pain, haematuria and ecchymotic patches. Treatment with systemic antibiotics, anticonvulsants, muscle relaxants and multivitamins were initiated by the paediatrician and he was referred to the dermatology department for ecchymotic patches. He was poorly built, lethargic with delayed milestones and spasticity in all four limbs. He had pallor and painful edema of the knee joints. Cutaneous examination revealed multiple ecchymotic patches over the knee joints and a few follicular and non-follicular palpable purpura on the lower limbs [Figure 1a]. We also noted sparse follicular keratotic papules and xerosis of the upper and lower limbs [Figure 1b]. We considered Henoch-Schönlein purpura and meningococcemia as differentials. Investigations revealed haemoglobin of 6.5 g/dL, reticulocyte count of 3.5%, white blood cell count of 8.3× 109/L with a normal differential count, and a platelet count of 233 × 109/L. His C-reactive protein level was 20 mg/L (normal <10 mg/L). Serum vitamin C level was 1.29 mg/dl (0.6–2 mg/dL). Blood cultures, coagulation profiles, electrolyte levels and liver and kidney function tests were all within reference ranges. Urine microscopy revealed 10 RBCs per field. Histopathological examination of palpable purpura revealed follicular plugging, a mild upper dermal lymphocytic infiltrate with extravasation of RBCs and no evidence of vasculitis. A radiological survey of the wrist and knees revealed cortical thinning, the Wimberger ring sign, the Frankel sign and the Pelkan spur [Figure 2]. The CT scan of brain showed subgaleal hematoma, cerebral atrophy and periventricular calcification. A normal blood culture and negative histopathologic features of Henoch-Schönlein purpura and the presence of characteristic radiological findings prompted the diagnosis of scurvy. The patient was re-evaluated for skin findings of scurvy. The dermoscopy of the keratotic papules revealed characteristic cork screw hair [Figure 3a]. Deep sectioning of histopathological tissue specimens revealed coiled hair [Figure 3b]. Thus the diagnosis of scurvy was confirmed. His ecchymotic patches and purpuric papules resolved completely with ten days of oral vitamin C (500 mg).

- Ecchymosis over knee joint.

- Xerosis with keratotic plugs over the knee joint.
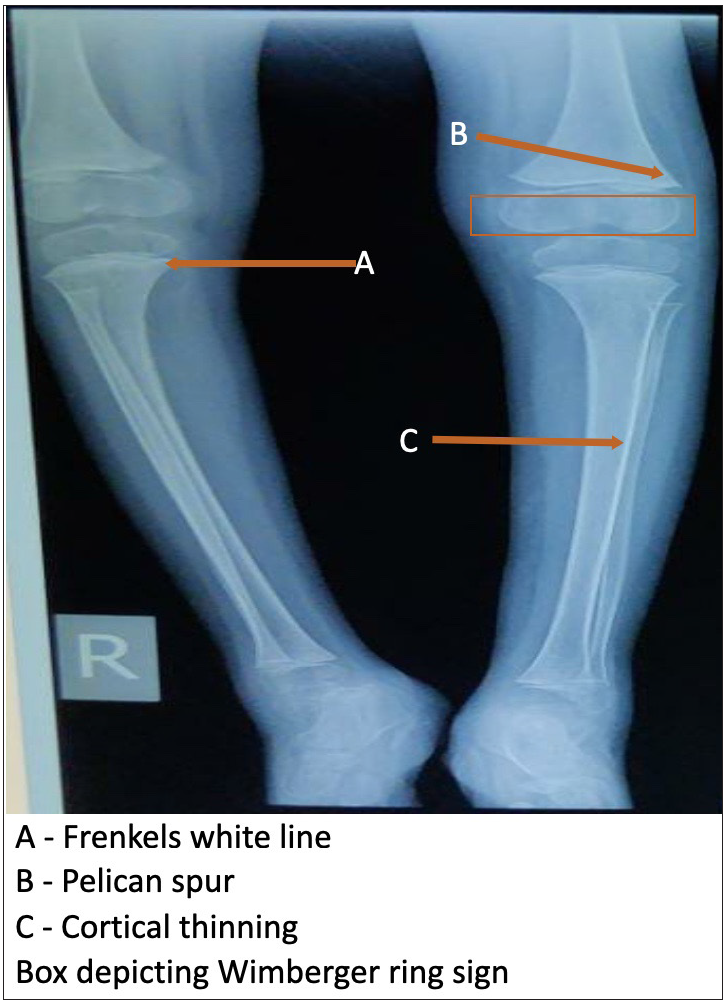
- Radiograph of knee joint.
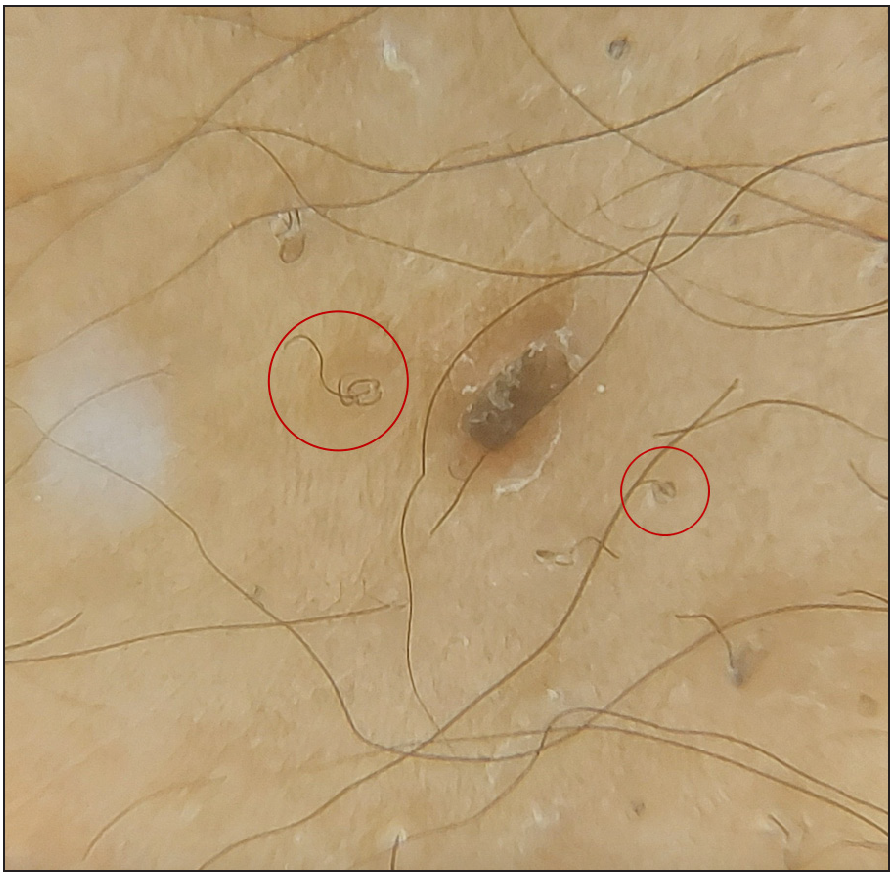
- Dermoscopy showing coiled hair.
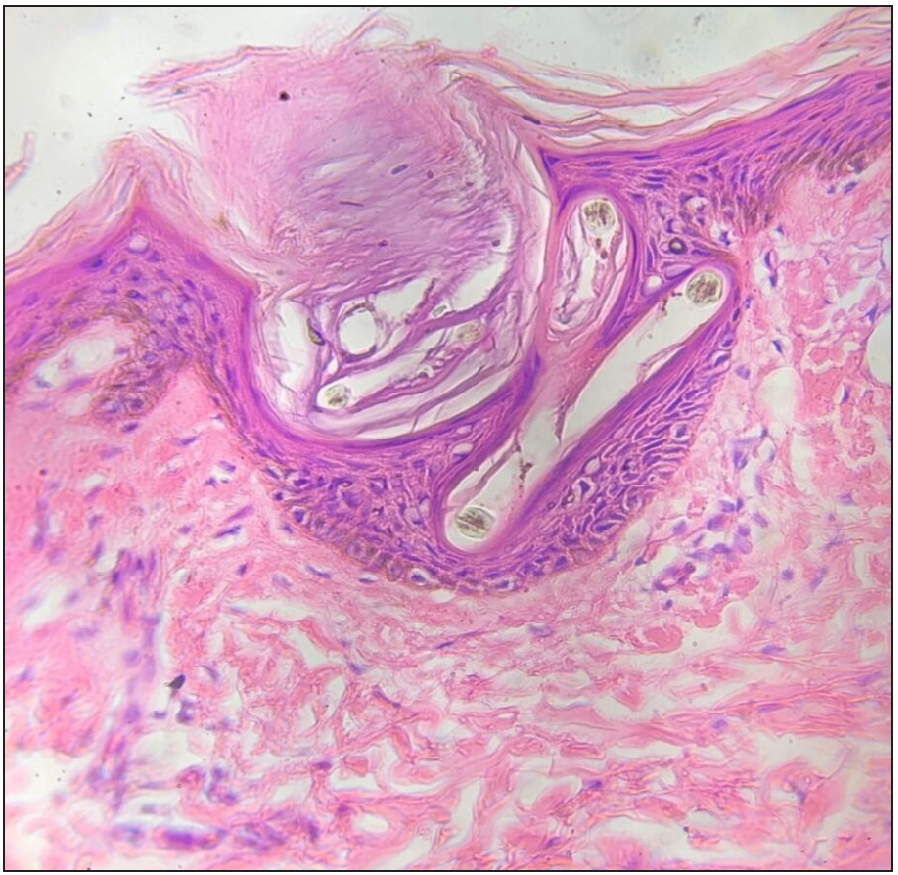
- Histopathology showing follicular plugging and corkscrew hair in epidermis (Haematoxylin & eosin, 40x).
Scurvy is a multiorgan systemic disease because of diversefunctions of vitamin C. The occurrence of scurvy in children with autism or other neuropsychiatric disorders is not uncommon.1 Additionally, the high-risk groups include children with iron load due to multiple blood transfusions, anorexia nervosa, celiac disease, Crohn’s disease, haemodialysis and other causes of a restricted diet.1 A few dermatological signs, which are seen in the early stages, are follicular hyperkeratosis and coiled corkscrew hair.2 Broken and lustreless hair are due to abnormal disulfide bonding and keratin formation.3 Fragile blood vessels resulting from impaired collagen synthesis give rise to perifollicular haemorrhages, petechiae and ecchymoses.2 Rarely, we may see nail splinter haemorrhages and alopecia.3 Serum vitamin C levels are considered specific, but laboratory tests are usually insensitive. It is known that serum concentrations do not always correspond with tissue storage of ascorbic acid. A reliable indicator of body storage is the measure of urinary excretion after intravenous ascorbic acid administration. Normally, 80% of absorbed vitamin C should be excreted within 3–5 hours. Also, the prompt resolution of symptoms after substitution treatment represents key evidence to confirm the diagnosis of scurvy.4 Multivitamin therapy is initiated in most critical cases, which explains the normal serum vitamin C level in our case. The patient had very subtle cutaneous features, making the diagnosis challenging. The natural course of undetected and untreated vitamin C deficiency can result in seizures and cardiac abnormalities and cases of sudden death have also been reported.5 This signifies the need for prompt detection and early treatment. The regimen for vitamin C supplementation in scurvy has not been established yet. Therapeutic supplementation with 1 g/day of oral vitamin C for 2 weeks is the usual treatment.5 The dose and duration of treatment should be individualised.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Scurvy: reemergence of nutritional deficiencies. Can Fam Physician. 2008;54:1403-6.
- [PubMed] [PubMed Central] [Google Scholar]
- Scurvy in an otherwise well young man. Med J Aust. 2006;185:331-2.
- [CrossRef] [PubMed] [Google Scholar]
- Musculoskeletal manifestations of scurvy. Joint Bone Spine. 2005;72:124-8.
- [CrossRef] [PubMed] [Google Scholar]





