Translate this page into:
Sensitive skin: An overview
Correspondence Address:
Arun C Inamadar
Department of Dermatology, SBMP Medical College, BLDE University, Bijapur - 586 103
India
| How to cite this article: Inamadar AC, Palit A. Sensitive skin: An overview. Indian J Dermatol Venereol Leprol 2013;79:9-16 |
Abstract
Sensitive skin is less tolerant to frequent and prolonged use of cosmetics and toiletries. It is self-diagnosed and typically unaccompanied by any obvious physical signs of irritation. With the change in lifestyle and also with increased opportunity to use many new brands of cosmetics and toiletries, there has been an increase in females complaining of unique sensation in their facial skin. Sensitive skin presents as smarting, burning, stinging, itching, and/or tight sensation in their facial skin. The condition is found in more than 50% of women and 40% of men, creating a sizable demand for products designed to minimize skin sensitivity. Good numbers of invasive and non-invasive tests are designed to evaluate and predict the sensitive skin. Management includes guidelines for selecting suitable cosmetics and toiletries in sensitive skin individuals.Introduction
Sensitive skin is self-diagnosed and typically unaccompanied by any obvious physical signs of irritation, and the number of individuals who claim sensitivity has risen steadily with the number of consumer products targeted toward this supposedly uncommon group. It affects a large part of the population and is accompanied with great interest by the cosmetic industry. Sensitive skin is a subject of intense research work. Approximately, 50% of women and 40% of men surveyed regarded themselves as having sensitive skin, creating a sizable demand for products designed to minimize skin sensitivity. [1],[2] Some studies have suggested that sensitive skin is a result of impaired barrier function, which leads to the exposure of immune system cells and sensitive nerves, resulting in marked cutaneous responses to otherwise harmless stimuli. [3]
Definition and Classification
A single definition of this condition remains elusive as the condition is self-diagnosed and there is no agreement, beyond heightened sensitivity, on its symptoms. [4] Generally accepted definition of sensitive skin is less tolerant to frequent and prolonged use of cosmetics and toiletries. [5] Sensitive skin (Syn. : r0 eactive, hyper-reactive, intolerant, or irritable skin) is defined [4],[6],[7],[8] as the onset of erythema and/or prickling, burning, or tingling sensations (possibly pain or pruritus), due to various factors, which may be physical (ultraviolet radiation, heat, cold, and wind), chemical (cosmetics, soap, water, and pollution), psychological (stress), or hormonal (menstrual cycle).
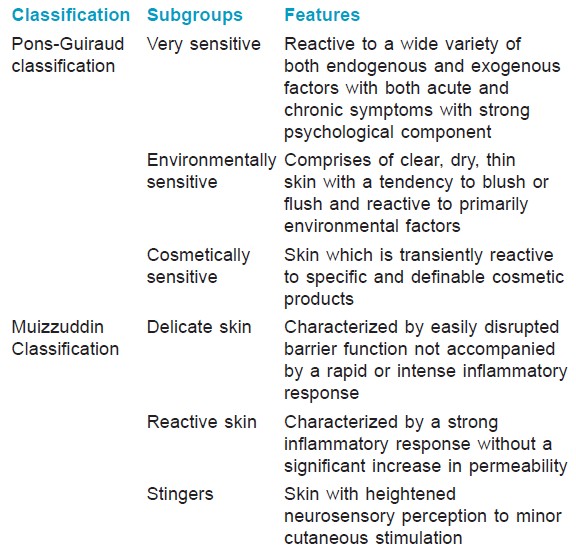
Sensitive skin can also be defined in both subjective form and objective terms. [9] Subjective perceptions (stinging, burning, pruritus, and tightness) of sensitive skin are noticed immediately following cosmetic product application or delayed by minutes, hours, or days. Objective perceptions of sensitive skin are based on physician evaluation and include the entire repertoire of cutaneous reactions. The phenomenon of sensitive skin is classified comprising of distinct subgroups of clinical sensitivities by Pons-Guiraud [4] and Muizzuddin [6] separately [Table - 1].
Epidemiology
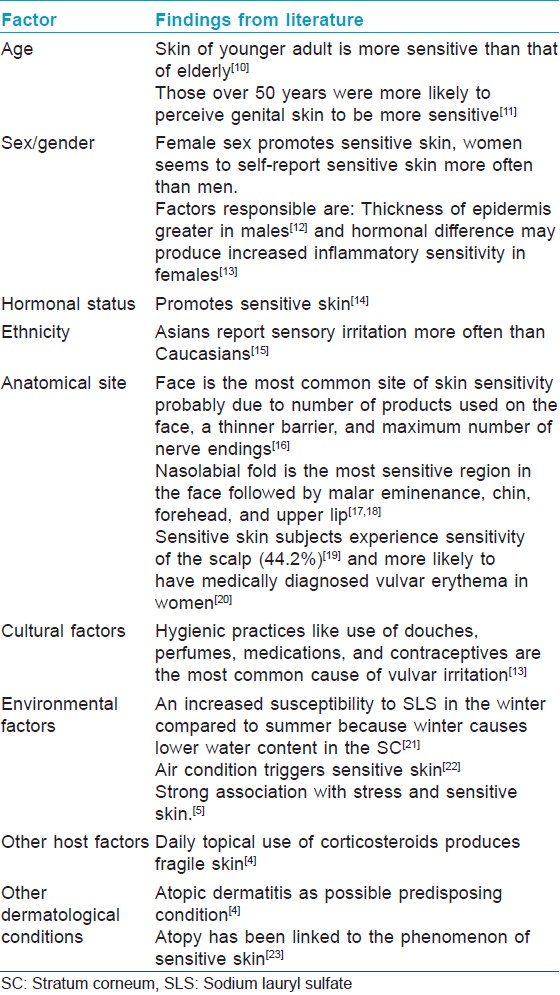
Numerous potential host factors and environmental factors play a role in experimental variableness noted in sensitive skin. Following section summarizes the findings from the literature on the effect of age, gender, race/ethnicity, anatomical site, cultural influences, environmental, and other possible factors on skin sensitivity.
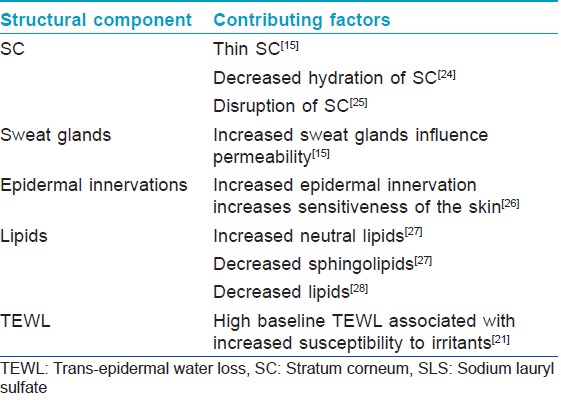
Host factors such as female sex, young adults aged between 18 and 50 years, hormonal differences in women producing increased inflammatory sensitivity, cultural habits in developed countries, and environmental factors like winter, stress, and atopic dermatitis are thought to promote sensitive skin [Table - 2]. Structural differences such as thickness, hydration level, and innervations in the stratum corneum (SC) and/or epidermis do play a role in propensity toward sensitive skin [Table - 3]. Baseline trans-epidermal water loss (TEWL) is significant for barrier function. Blacks and Asians will have higher baseline TEWL making them more prone for "sensitive skin."
Pathophysiology
Pathophysiology of sensitive skin is poorly understood. Main feature of sensitive skin is decrease in "skin′s threshold," not directly related to any immunological or allergic mechanism. Sensitive skin individual may have one of the following anatomical cutaneous changes : 0 heightened neurosensory input, enhanced immune responsiveness, and/or diminished barrier function. [9] Understanding of each of these factors is helpful in identifying the pathophysiology of varied presentations of sensitive skin.
Neural basis
Variety of sensory symptoms noted in sensitive skin, point fingers to neurosensory dysfunction of nerves in the skin. Sensitive skin patients may have [9] following neural changes to account for this reaction:
- Altered nerve endings
- Increased neurotransmitter release
- Unique central information processing
- Chronic nerve ending trauma, and
- Slower neurotransmitter removal.
A study, using functional magnetic resonance imaging (MRI), established a link between the intensity of self-perceived sensitive skin and modification of cerebral activation in response to lactic acid-induced skin provocative test. [29] It showed an increased activity in the primary sensorimotor cortex contralateral to the application site as well as in a bilateral frontoparietal network. They were also observed to have significantly greater increases in neural activity than those without sensitive skin.
Skin sensations, such as pain, itching, and warmth are mediated by unmyelinated C-fibers. [30] They are equipped with sensory neuroreceptors [31] such as endothelin receptors (ET) and transient receptor potential (TRP) family receptors for pain (noxious thermoreceptors), heat (heat receptors), cold (cold receptors: TRPM8, TRPA1), and neurotropins (role in skin homeostasis and inflammatory diseases). These sensory receptors are expressed on nerve endings and also in keratinocytes, which may explain why sensitive skin responds to different environmental, physical, and chemical factors limited to the skin. [30]
ET receptors may be involved in mediating nociceptive symptoms in sensitive skin. [31] Heat receptor TRPV1 (vanilloid receptor) is involved in epidermal barrier homeostasis and has an influence on the barrier function in sensitive skin. [32] Cold receptor, TRPM8, is involved in cold-mediated sensitive skin. [33]
Neural basis of sensitive skin suggests that the physical factors may lead to an interaction between nerve growth factor, ET, and TRP receptors, which may induce hypersensitivity and results in the symptoms of sensitive skin. [31]
Skin barrier impairment
A well-organized multilayered lipid structure between the corneocytes is essential for barrier function. Perturbed barrier function causes patients with pre-existing clinical and subclinical dermatological disease to present with sensitive skin. [9] Dry skin, rosacea, and acne have also been linked to enhance skin reactivity and were associated with sensitive skin, which may indicate a tendency to barrier impairment and increased vascular reactivity. [1],[25] Barrier permeability is key to identify sensitive skin population.
Clinical Parameters
Phenomenon of sensitive skin is diagnosed mainly by the subjective perceptions from patient observation. It is devoid of documental clinical signs. There can be identifiable clinical parameters with subjective irritation such as less hydrated and less supple skin. Skin will be more erythematous and more telangiectatic. [34]
Investigation for Sensitive Skin
We cannot depend on the conventionally utilized histopathological studies that involve invasive procedures for the study of such normal appearing skin of healthy young adult female viz., of facial skin! Pre-marketing testing is essential to ensure that the cosmetic and skin care products developed for "sensitive skin" population perform upto expectations to give the treating dermatologist confidence in prescribing them. This necessity has resulted in development of an array of tests for assessment purpose. [9] Kligman encouraged his co-workers to introduce non-invasive bio-physical measurements for evaluation of sensitive skin. [35]
Testing methods for the investigation of sensitive skin are as follows [9] and they are tabulated with the details in respective tables:
- Tests for the development of sensitive skin panels [Table - 4]
 Table 4: Tests for the development of sensitive skin panels
Table 4: Tests for the development of sensitive skin panels - Bio-engineering tests to measure skin response [Table - 5]
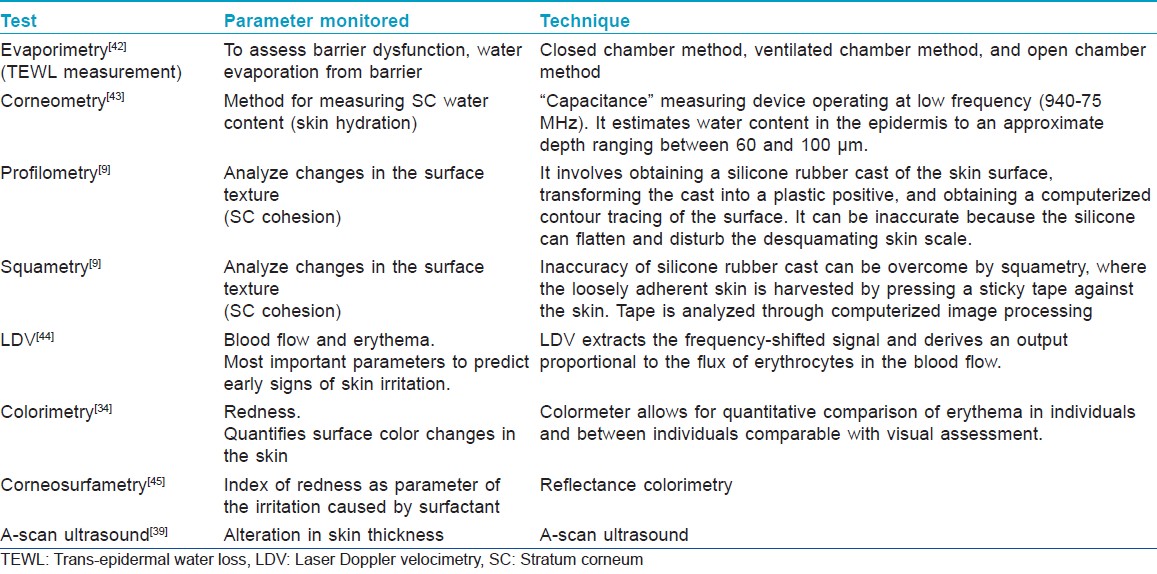 Table 5: Bio-engineering tests to measure skin response
Table 5: Bio-engineering tests to measure skin response -
In vivo testing on sensitive skin population [Table - 6]
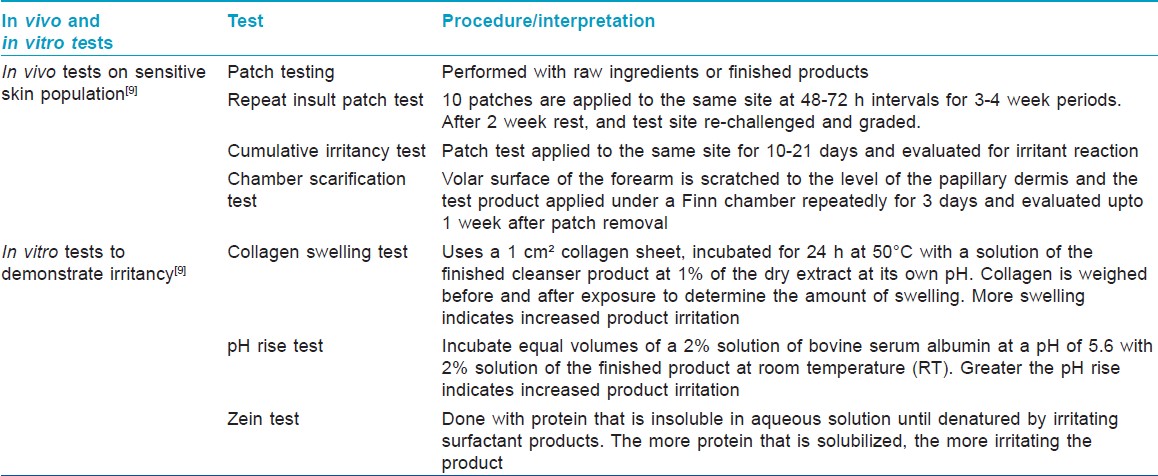 Table 6: In vivo and in vitro tests for evaluation of sensitive skin
Table 6: In vivo and in vitro tests for evaluation of sensitive skin - In vitro tests to demonstrate irritancy [Table - 6].
Methods are divided into those that assess neurosensory response (sensory reactivity tests), those that assess visible cutaneous signs of irritation (irritant reactivity tests), and those that measure structural and physiological parameters of the skin for indications of irritant effect (dermal function tests). In most of the tests designed to investigate the visible heightened neurosensory aspects of the sensitive skin, either stinging (lactic acid test) or vasodilatation sodium lauryl sulfate test is assessed. Most common site of test is nasolabial fold followed by cheek and forearm. There can be more intense stinging response in winter than summer. It may be due to the cumulative effect of heightened neurosensory input combined with defective barrier function possibly associated with the xerosis of winter. [46] Kligman was the pioneering dermatologist showing great interest in the development of non-invasive skin assessment allowing presumably more accurate evaluation of physiological changes indicative of sensitive skin. It is presumed that physiological changes indicative of sensitive skin can be detected at low levels before clinical disease presentation. [9] Following are the tests done and the parameters monitored from the test. [9],[34]
- TEWL: Water evaporation from barrier
- Corneometry: Skin hydration
- Colorimetry: Redness/erythema
- Squametry and Corneosurfametry: SC cohesion
- Laser Doppler velocimetry: Blood flow alterations/erythema
- A-scan ultrasound: Alteration in skin thickness.
Most popular non-invasive test is TEWL measurement. It is based on the estimation of water pressure gradient above the skin surface. It is done by two different techniques: Open chamber method and ventilated chamber method. Detailed account of methods can be found in article by Primavera and Berardesca. [34]
In vivo testing on sensitive skin population includes patch testing, repeat insult patch testing, cumulative irritancy testing, the chamber scarification test, the modified soap chamber test, and the forearm controlled application technique. The details are tabulated in [Table - 6]. Three common in vitro tests to evaluate the irritant potential of soaps are collagen swelling test, pH rise test, and Zein test.
Management
Management of sensitive skin involves treating the person affected, apt approach to formulate cosmetics and toiletries for sensitive skin individuals, and simple evaluation procedures with step by step elimination, avoidance, and introduction of cosmetics.
Approach to 0formulating 0sensitive 0skin 0products
Formulations appropriate for sensitive skin must avoid inducing both visible and invisible manifestations of skin sensitivity. [47] Demonstrable ability of the product appropriate for sensitive skin to reduce lactic acid malar eminence facial stinging after 6 days of application is a convenient test criterion. [9] Following are the goals to be met by any product for sensitive skin as detailed by Draelos. [9],[48],[49]
- Elimination of common allergens and irritants from formulations
- Eliminate highly allergenic contaminants
- Use suitable anti-oxidants
- Volatile vehicles like menthol to be eliminated or reduced
- Avoid solvents that promote skin penetration (propylene glycol), select polyethylene glycols that do not penetrate SC
- Careful selection of surfactants
- Select low sensitizing preservatives.
Treatment of sensitive skin patient
There is no simple treatment routine for managing the sensitive skin. It involves a detailed protocol designed to provide logical and timely approach to the treatment. It is going to be time-consuming exercise because of the number of cosmetics and toiletries involved in the causation of the condition. There is going to be series of "do′s" and "don′t′s" while selecting the right cosmetics.
Certain "do′s" while selecting the cosmetic for sensitive skin are the following:
- Powder cosmetics preferred
- Use cosmetics which are easily removable by water
- Always use fresh cosmetics
- Use black-colored eyeliner and mascara
- Select pencil form of eyeliner and eyebrow cosmetics
- Select light earth tone eye shadows
- Select physical sunscreen agent
- Purchase cosmetics products with less than 10 ingredients
- No nail polishes
- Use powder/cream formulations of facial foundations.
An approach to treating the patient with sensitive skin [9] useful in practice is as follows:
A. "Two-week" strategy
- Discontinue all topical cosmetics and skin care products and use only synthetic detergent (Syndets) soap for 2 weeks. (Soap vs. Syndet : d0 iffer in surfactant, differ in pH, Syndet bars are milder or less irritating than soap-based bars, always consider the surfactant and the key ingredients of cleansing bars because of their interaction with SC.)
- Discontinue all topical prescription medications with drying and irritating ingredients (e.g., tretinoin, benzoyl peroxide) for 2 weeks.
- Eliminate all sources of skin friction for 2 weeks.
- After 2 weeks, examine for any underlying dermatoses (e.g.. rosacea) and treat with appropriate medications for at least 2 weeks.
B. Tests/evaluation
- Patch and photo-patch test patient to find out any sources of allergic contact dermatitis and advise the patient accordingly.
- Do facial sting test.
- Provocative use test : t0 esting of cosmetics that are common source of sensitive skin. Apply them at least 5 nights to a 2-cm area lateral to the eye. They should be tested in the following order : m0 ascara, eye liner, eyebrow pencil, eye shadow, facial foundation, and any other colored facial cosmetics.
C. Restart
Allow the female patient to add one facial cosmetic of low-allergenic potential per week in the following order : l0 ipstick, face powder, powder blush, etc.
Novel approaches for treatment of sensitive skin
There are ongoing studies in search of a better molecule to treat or prevent the "sensitive skin" issue. The tremendous interest is based on several studies showing that about 50% of the population declares to have sensitive skin. Two studies showing promising results are discussed below.
Trans-4-tert-butylcyclohexanol
Skin sensitivity toward capsaicin, a natural activator of TRPV1, is known to correlate with sensitive skin. In a screening campaign based on recombinant HEK293-cells stably transfected with hTRPV1, the selective antagonist trans-4-tert-butylcyclohexanol was identified. This antagonist is able to inhibit capsaicin-induced hTRPV1 activation. In a clinical study [50] with 30 women using topical treatment with O/W emulsions containing 31.6 ppm capsaicin, authors were able to show that 0.4% of this inhibitor significantly reduces capsaicin-induced burning (P < 0.0001) in vivo. Thus, trans-4-tert-butylcyclohexanol has the potential as a novel bioactive for the treatment of sensitive skin.
Bacterial lysate
In a study [51] using a probiotic lysate, Bifidobacterium longum sp. extract, authors demonstrated first in vitro, and then in a clinical trial, that this non-replicating bacteria form applied to the skin was able to improve sensitive skin. Ten percent topical cream containing the active extract was tested in a randomized, double-blind, placebo-controlled trial in 66 female volunteers. Clinical and self-assessment scores revealed a significant decrease in skin dryness after 29 days for volunteers treated with the cream containing the 10% bacterial extract. Authors speculate that this new ingredient may decrease skin sensitivity by reducing neuron reactivity and neuron accessibility. The study findings suggest that new approaches, based on a bacterial lysate, could be developed for the treatment and/or prevention of symptoms related to reactive skin.
Conclusion
Sensitive skin is a universal phenomenon in modernized society with ample usage of cosmetics and toiletries. Though the incidence is lower than Caucasians, it is seen among Asians too. Various invasive and non-invasive bio-physical methods have been developed to assess and predict sensitive skin. Facial skin exhibits unique functional properties and is the common site of sensitive skin. Barrier stability of SC is an important player in causation of sensitive skin. Neurotransmitters with neuroreceptors play role in the pathogenesis of sensitive skin. Management involves selection of right cosmetics and toiletries and what to avoid or use.
| 1. |
Willis CM, Shaw S, Lacharriere OD, Baverel M, Reiche L, Jourdain R, et al. Sensitive skin: An epidemiological study. Br J Dermatol 2001;145:258-63.
[Google Scholar]
|
| 2. |
Loffler H, Aramaki J, Effendy I, Maibach H. Sensitive skin. In: Zhai H, Maibach H, editors. Dermatotoxicology. New York: CRC Press; 2004. p. 123-35. s
[Google Scholar]
|
| 3. |
Pedro P, Catarina R, Catarina P, Monteiro RL. Is there any barrier impairment in sensitive skin?: A quantitative analysis of sensitive skin by mathematical modeling of transepidermal water loss desorption curves. Skin Res Technol 2011;17:181-5.
[Google Scholar]
|
| 4. |
Pons-Guiraud A. Sensitive skin: A complex and Multifactorial syndrome. J Cosmet Dermatol 2005;3:145-8.
[Google Scholar]
|
| 5. |
Farage MA. Perceptions of sensitive skin: Changes in perceived severity and associations with environmental causes. Contact Dermatitis 2008;59:226-30.
[Google Scholar]
|
| 6. |
Muizzuddin N, Marenus KD, Maes DH. Factors defining sensitive skin and its treatment. Am J Contact Dermat 1998;9:170-5.
[Google Scholar]
|
| 7. |
Frosch PJ, Kligman AM. A method of apraising the stinging capacity of topically applied substances. J Soc Cosmet Chem 1977;28:197-209.
[Google Scholar]
|
| 8. |
Berardesca E, Fluhr JW, Maibach HI. What is sensitive skin? In: Berardesca E, Fluhr JW, Maibach HI, editors. Sensitive Skin Syndrome. New York: Taylor & Francis; 2006. p. 1-6.
[Google Scholar]
|
| 9. |
Draelos ZD. Sensitive skin: Perceptions, evaluation, and treatment. Contact Dermatitis 1997;8:67-78.
[Google Scholar]
|
| 10. |
Cua AB, Wilhelm KP, Maibach HI. Cutaneous sodium lauryl sulphate irritation potential: Age and regional variability. Br J Dermatol 1990;123:607-13.
[Google Scholar]
|
| 11. |
Farage MA. Perceptions of sensitive skin with age. In: Farage MA, Miller KW, Maibach HI, editors. Textbook of Aging Skin. Berlin-Heidelberg: Springer-Verlag; 2010. p. 1027-46.
[Google Scholar]
|
| 12. |
Sandby-Møller J, Poulsen T, Wulf HC. Epidermal thickness at different body sites: Relationship to age, gender, pigmentation, blood content, skin type and smoking habits. Acta Derm Venereol 2003;83:410-3.
[Google Scholar]
|
| 13. |
Farage MA. Vulvar susceptibility to contact irritants and allergens: A review. Arch Gynecol Obstet 2005;272:167-72.
[Google Scholar]
|
| 14. |
Britz MB, Maibach HI, Anjo DM. Human percutaneous penetration of hydrocortisone: The vulva. Arch Dermatol Res 1980;267:313-6.
[Google Scholar]
|
| 15. |
Aramaki J, Kawana S, Effendy I, Happle R, Loffler H. Differences of skin irritation between Japanese and European women. Br J Dermatol 2002;146:1052-6.
[Google Scholar]
|
| 16. |
Chew A, Maibach H. Sensitive skin. In: Loden M, Miabach H, editors. Dry Skin and Moisturizers: Chemistry and Function. Boca Raton, FL: CRC Press; 2000. p. 429-40.
[Google Scholar]
|
| 17. |
Saint-Martory C, Roguedas-Contios AM, Sibaud V, Degouy A, Schmitt AM, Misery L. Sensitive skin is not limited to the face. Br J Dermatol 2008;158:130-3.
[Google Scholar]
|
| 18. |
Marriott M, Holmes J, Peters L, Cooper K, Rowson M, Basketter DA. The complex problem of sensitive skin. Contact Dermatitis 2005;53:93-9.
[Google Scholar]
|
| 19. |
Misery L, Sibaud V, Ambronati M, Macy G, Boussetta S, Taieb C. Sensitive scalp: Does this condition exist? An epidemiological study. Contact Dermatitis 2008;58:234-8.
[Google Scholar]
|
| 20. |
Farage MA, Bowtell P, Katsarou A. The relationship among objectively assessed vulvar erythema, skin sensitivity, genital sensitivity, and self-reported facial skin redness. J Appl Res 2006;6:272-81.
[Google Scholar]
|
| 21. |
Lee CH, Maibach HI. The sodium lauryl sulfate model: an overview. Contact Dermatitis 1995;33:1-7.
[Google Scholar]
|
| 22. |
Misery L, Myon E, Martin N, Consoli S, Boussetta S, Nocera T, et al. Sensitive skin: Psychological effects and seasonal changes. J Eur Acad Dermatol Venereol 2007;21:620-8.
[Google Scholar]
|
| 23. |
Effendy I, Loeffler H, Maibach HI. Baseline transepidermal water loss in patients with acute and healed irritant contact dermatitis. Contact Dermatitis 1995;33:371-4.
[Google Scholar]
|
| 24. |
Corcuff P, Lotte C, Rougier A, Maibach HI. Racial differences in corneocytes. A comparison between black, white and oriental skin. Acta Derm Venereol 1991;71:146-8.
[Google Scholar]
|
| 25. |
Loffler H, Effendy I. Skin susceptibility of atopic individuals. Contact Dermatitis 1999;40:239-42.
[Google Scholar]
|
| 26. |
Marriott M, Whittle E, Basketter DA. Facial variations in sensory responses. Contact Dermatitis 2003;49:227-31.
[Google Scholar]
|
| 27. |
Lampe MA, Burlingame AL, Whitney J, Williams ML, Brown BE, Roitman E, et al. Human stratum corneum lipids: Characterization and regional variations. J Lipid Res 1983;24:120-30.
[Google Scholar]
|
| 28. |
Seidenari S, Francomano M, Mantovani L. Baseline biophysical parameters in subjects with sensitive skin. Contact Dermatitis 1998;38:311-5.
[Google Scholar]
|
| 29. |
Querleux B, Dauchot K, Jourdain R, Bastien P, Bttoun J, Anton JL, et al. Neural basis of sensitive skin: An fMRI study . Skin Res Technol 2008;14:454-61.
[Google Scholar]
|
| 30. |
Denda M, Nakatani M, Ikeyama K, Tsutsumi M, Denda S. Epidermal keratinocytes as the forefront of the sensory system. Exp Dermatol 2007;16:157-61.
[Google Scholar]
|
| 31. |
Stander S, Schneider SW, Weishaupt C, Luger TA, Misery L. Putative neural mechanisms of sensitive skin. Exp Dermatol 2009;18:417-23.
[Google Scholar]
|
| 32. |
Kawamata T, Ji W, Yamamoto J, Niiyama Y, Furuse S, Namiki A. Contribution of transient receptor potential vanilloid subfamily 1 to endothelin-1-induced thermal hyperalgesia. Neuroscience 2008;154:1067-76.
[Google Scholar]
|
| 33. |
Xing H, Chen M, Ling J, Tan W, Gu JG. TRPM8 mechanism of cold allodynia after chronic nerve injury. J Neurosci 2007;27:13680-90.
[Google Scholar]
|
| 34. |
Primavera G, Beradesca E. Sensitive skin: Mechanisms and diagnosis. Int J Cosmet Sci 2005;27:1-10.
[Google Scholar]
|
| 35. |
Kligman AM. The invisible dermatoses. Arch Dermatol 1991;127:1375-82.
[Google Scholar]
|
| 36. |
Frosch P, Kligman AM. Method for appraising the sting capacity of topically applied substances. J Soc Cosmet Chem 1977;28:197-209.
[Google Scholar]
|
| 37. |
Christensen M, Kligman AM. An improved procedure for conducting lactic acid stinging tests on facial skin. J Sot Cosmet Chem 1996;47:1-11.
[Google Scholar]
|
| 38. |
Agner T, Serup J. Quantification of the DMSO response: A test for assessment of sensitive skin. Clin Exp Dermatol 1989;14:214-7.
[Google Scholar]
|
| 39. |
Agner T, Serup J. Skin reactions to irritants assessed by non-invasive bioengineering methods. Contact Dermatitis 1989;20:352-9.
[Google Scholar]
|
| 40. |
Berardesca E, Cespa M, Farinelli N, Rabbiosi G, Maibach H. In viva transcutaneous penetration of nicotinates and sensitive skin. Contact Dermatitis 1991;25:35-8.
[Google Scholar]
|
| 41. |
Hannuksela A, Hannuksela M. Irritant effects of a detergent in wash and chamber tests. Contact Dermatitis 1995;32:163-6.
[Google Scholar]
|
| 42. |
Wilson DR, Maibach H. Transepidermal water loss: A review. In: Leveque JL, editor. Cutaneous investigation in health and disease. Noninvasive methods and instrumentation. New York: Marcel Dekker Inc.; 1989. p. 113-33.
[Google Scholar]
|
| 43. |
Berardesca E. EEMCO guidance for the assessment of the stratum corneum hydration: Electrical methods. Skin Res Technol 1997;3:126-32.
[Google Scholar]
|
| 44. |
Zuang VR, Archer G, Berardesca E. Detection of skin irritation potential of cosmetics by non-invasive measurements. Skin Pharmacol Appl Skin Physiol 2000;13:358-71.
[Google Scholar]
|
| 45. |
Pierard GE, Goffin V, Pierard-Franchimont C. Corneosulfametry: A predictive assessment of the interaction of personal care cleansing products with human stratum corneum. Dermatology 1994;189:152-6.
[Google Scholar]
|
| 46. |
Leyden JJ. Risk assessment of products used on skin. Am J Contact Dermat 1993;4:158-62.
[Google Scholar]
|
| 47. |
Maes D, Marenus K, Smith WP. Invisible irritation: A new look at product safety. Cosmet Toilet 1990;105:43-50.
[Google Scholar]
|
| 48. |
Amin S, Maibach HI. Cosmetic intolerance syndrome: Pathophysiology and management. Cosmet Dermatol 1996;9:34-42.
[Google Scholar]
|
| 49. |
Maibach HI, Engasser PG. Dermatitis due tocosmetits. In: Fisher AA, editor. Contact Dermatitis. 3 rd ed. Philadelphia, PA: Lea & Febiger; 1986. p. 368-93.
[Google Scholar]
|
| 50. |
Kueper T, Krohn M, Haustedt LO, Hatt H, Schmaus G, Vielhaber G. Inhibition of TRPV1 for the treatment of sensitive skin. Exp Dermatol 2010;19:980-6.
[Google Scholar]
|
| 51. |
Gueniche A, Bastien P, Ovigne JM, Kermici M, Courchay G, Chevalier V, et al. Bifidobacterium longum lysate: A new ingredient for reactive skin. Exp Dermatol 2010;19:e1-8.
[Google Scholar]
|
Fulltext Views
18,308
PDF downloads
3,701





