Translate this page into:
Sensitivity and specificity of the trichoscopy
Correspondence Address:
Elzbieta Kowalska-Oledzka
ul. Bony 34a, 02-496 Warsaw
Poland
| How to cite this article: Kowalska-Oledzka E, Slowinska M, Rakowska A. Sensitivity and specificity of the trichoscopy. Indian J Dermatol Venereol Leprol 2012;78:636-637 |
Sir,
Chronic hair loss frequently affects female patients, but there is little or no objective technology available to aid the dermatologist in setting a proper diagnosis and monitoring treatment efficacy. Nowadays the diagnosis of alopecia is made on the basis of medical history of hair loss, clinical examination (the presence of hair thinning evaluated by the three-point Ludwig scale, the Olsen scale, or the Hamilton-Norwood scale in female androgenic alopecia (FAGA)), diffuse hair loss in telogen effluvium (TE), pull test, trichogram, and histopathology. [1],[2] Trichoscopy is a noninvasive method which could be used as a diagnostic tool in hair and scalp disorders and limits the necessity of performing the biopsy. [3],[4] In order to determine the specificity and sensitivity of the trichoscopy in a diagnosing process of hair loss in female patients, we examined 296 female patients with hair loss including 141 patients with FAGA, 54 with TE, 97 with FAGA coexistent with TE (FAGA + TE), and 50 healthy controls without any medical history about hair loss. The mean age of patients was 36.1 years (18-65, SD 12.5) [Figure - 1] and [Figure - 2]. The mean age of healthy controls was 36.4 (19-64, SD 12.1). All patients and the control group were examined by trichoscopy with the use of Fotofinder II (Teachscreen Software, Bad Brinbach, Germany) according to the standard procedure. [5] A typical trichoscopic pattern for FAGA showed reduced number of terminal hairs in the frontal area vs. occipital area, increased number of vellus hairs and empty follicular orifices in the frontal area, reduction of mean thickness of hair shafts, reduction of the percentage of triple-hair units with simultaneous increase of percentage of single-hair units, and increased percentage of thin hairs with concomitant decreased percentage of thick hairs and the presence of perifollicular discolorations in the frontal area. TE was characterized by early regrowth of new terminal hairs, few vellus hairs, and empty follicular orifices, reduction of the percentage of triple-hair units with simultaneous increase of percentage of single-hair units, and increased percentage of thin hairs with concomitant decreased percentage of thick hairs. Due to conducted analysis, we proved that the trichoscopic diagnosis and the clinical diagnosis showed high compliance (P for a marginal homogeneity test ≤0.0001). Cohen′s kappa coefficient, a standard, statistical measure of the compatibility of two diagnostic methods, for the trichoscopic diagnosis and the clinical diagnosis was 0.8262 and achieved the satisfactory level. We diagnosed FAGA by trichoscopy in 145 cases (vs. 141 cases as a clinical diagnosis), 47 cases of TE (vs. 54 cases as a clinical diagnosis), 43 cases of FAGA + TE (vs. 97 cases as a clinical diagnosis), 40 cases of FAGA with regrowth (vs. 0), and 19 cases without any abnormalities in trichoscopy (vs. 0). We also calculated the sensitivity and specificity of the trichoscopic diagnosis vs. clinical diagnosis for FAGA and TE. Trichoscopy as a diagnostic method for FAGA was characterized by very high sensitivity and achieved 96% and also high specificity reached 98%. Very high PPV (positive predictive value) and NPV (negative predictive value) coefficients indicated 1% of false-positive results and 7% false-negative results. Likelihood ratios for positive and negative results proved important role of the trichoscopy to confirm the diagnosis of FAGA (LR + 60.06) and usefulness to the excluding of the androgenic alopecia. Lower values of sensitivity of the trichoscopy were detected in the diagnosis of TE and revealed 85%. The value of specificity for TE was comparable and revealed 98%. These results were verified by high PPV (4% false-negative results) and NPV (10% false-negative results).
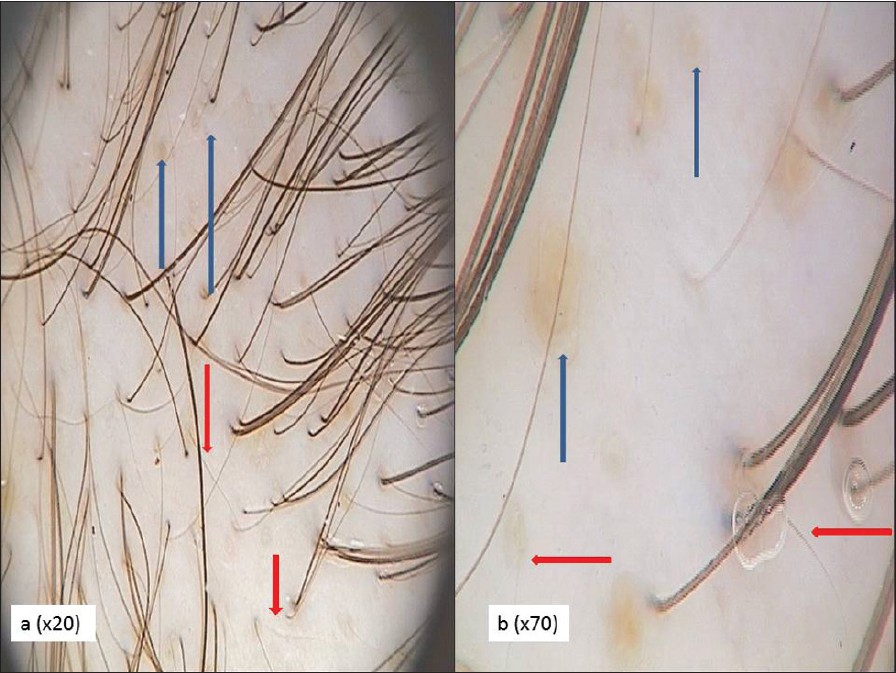 |
| Figure 1: Androgenic alopecia. Trichoscopy of the frontal area of the scalp (a: 20-fold and b: 70-fold). Blue arrows - yellow dots, red arrows - vellus hairs |
 |
| Figure 2: Telogen effluvium. Trichoscopy of the frontal area of the scalp (c: 20-fold and d: 70-fold). Thin- and medium-sized hairs, single-hair and double-hair units |
The comparison of the diagnosis compliance for the trichogram and the trichoscopy was also performed and showed that only 82 from 116 cases of FAGA diagnosed by trichoscopy confirm the diagnosis by trichogram (70, 6%). Of 39 patients with trichoscopic diagnosis of FAGA + TE, 16 (41%) were positively verified by the trichogram. There is no possibility to confirm the diagnosis of FAGA with hair regrowth by trichogram (35 patients in the trichoscopy vs. 0 in the trichogram). Fifty percentage of cases diagnosed as TE in the trichogram maintain the diagnosis in trichoscopy.
Cohen′s kappa coefficient was 0.0997 and revealed the nonsatisfactory level. Sensitivity of the trichoscopy vs. trichogram reached 93% for diagnosing FAGA and 54% for TE. Specificity achieved lower values: 34% for FAGA and 62% for TE. Trichoscopy can also precise the diagnosis of coexistence of FAGA and TE. Presented data proved that the trichoscopy is characterized by high sensitivity and specificity in the diagnosis of FAGA and TE and could be consider as a reference test for the diagnostic purposes.
| 1. |
Blume-Peytavi U, Blumeyer A, Tosti A, Finner A, Marmol V, Trakatelli M, et al. S1 guidelines for diagnostic evaluation in androgenic alopecia in men, women and adolescents. Br J Dermatol 2011;164:5-15.
[Google Scholar]
|
| 2. |
Sinclair R, Jolley D, Mallari R, Magee J. The reliability of horizontally sectioned scalp biopsies in the diagnosis of chronic diffuse telogen hair loss in women. J Am Acad Dermatol 2004;51:189-99.
[Google Scholar]
|
| 3. |
Rudnicka L, Olszewska M, Rakowska A, Kowalska-Oledzka E, Slowinska M. Trichoscopy: A new method for diagnosing hair loss. J Drugs Dermatol 2008;7: 651-4.
[Google Scholar]
|
| 4. |
Ross EK, Vincenzi C, Tosti A. Videodermoscopy in the evaluation of hair and scalp disorders. J Am Acad Dermatol 2006;55:799-806.
[Google Scholar]
|
| 5. |
Rakowska A, Slowinska M, Kowalska-Oledzka E, Olszewska M, Rudnicka L. Dermoscopy in female androgenic alopecia: Method standarization and diagnostics criteria. Int J Trichology 2009;1:123-30.
[Google Scholar]
|
Fulltext Views
4,174
PDF downloads
2,617





