Translate this page into:
Serpentine and annular presentation of extragenital lichen sclerosus-morphea overlap
Corresponding author: Dr. Anupama Bains, Department of Dermatology, All India Institute of Medical Sciences, Jodhpur, India. whiteangel2387@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhatia D, Bains A, Vishwajeet V. Serpentine and annular presentation of extragenital lichen sclerosus-morphea overlap. Indian J Dermatol Venereol Leprol. 2025;91:S43-S45. doi: 10.25259/IJDVL_1317_2023
Dear Editor,
Morphea and lichen sclerosus et atrophicus (LS) share many clinical and histopathological features and are considered as a part of the same disease spectrum.1 We report a case of annular and serpentine presentation of extragenital lichen sclerosus – morphea overlap leading to deformity of fingers.
A 30-year-old woman presented with complaints of multiple asymptomatic depigmented atrophic plaques on the dorsal surface of both hands for the past three years. These were gradually progressive leading to difficulty in mobilisation of distal interphalangeal joints (DIP) of both index fingers. Examination revealed well-defined ivory white plaques with central atrophy, peripheral hyperpigmentation arranged in an annular and serpentine pattern on the dorsum of the index and little fingers of the right hand [Figure 1a]. The lesion on the right index and middle finger was extending up to the fingertip leading to atrophy and thinning of the pulp of the fingertips. Also, partial fixed flexion deformity of DIP of both right and left index fingers was noted [Figures 1b and 1c]. There were no genital lesions. There was no history suggestive of connective tissue disorders like Raynaud phenomenon and photosensitivity. Dermoscopic evaluation of the annular lesion revealed whitish keratotic follicular plugs on the background of white structureless patches in an annular pattern and a few chrysalis-like structures [Figure 2] (Dermlite 4, non-polarising mode, 20x). Skin biopsy from lesions showed hyperkeratosis, follicular plugging, a flattened and thinned out epidermis with sclerosis and homogenization of collagen reaching up to the deeper dermis with interspersed mild interstitial lymphocytic inflammatory infiltrate in the dermis and decreased appendages [Figures 3a, 3b and 3c]. Special stains for elastin like Verhoeff-van Gieson stain could not be done due to their unavailability at our centre. Considering the deformity of multiple digits, we also did a rheumatological workup including X-rays of both hands and rheumatoid factor which was normal. Clinically, the patient had fixed flexion deformities in multiple fingers and histopathology showed dense sclerosis reaching up to the deeper dermis with a lack of vacuolar degeneration along the dermo-epidermal junction which was suggestive of morphea. Also, the presence of depigmented atrophic plaques with multiple follicular plugs which were more prominent on dermoscopy and histopathological findings of hyperkeratosis, follicular plugging with thinned out epidermis were suggestive of LS. Therefore, although histopathology was more suggestive of morphea, on the basis of overall clinical, dermoscopy and histopathological findings the diagnosis of extragenital LS- morphea overlap was made. The patient was treated with oral betamethasone 5 mg twice a week along with clobetasol propionate ointment 0.05% once a day application. She was also advised physiotherapy. The patient is under follow-up and has shown improvement in terms of no new lesions and no extension of the previous lesions.

- Well-defined depigmented plaques with central atrophy on the dorsal surface of fingers. Note the serpentine pattern on the index finger and annular morphology on the little finger and ring finger.

- Depigmented atrophic linear plaques extending up to the fingertips and leading to atrophy and thinning of finger pulp of both index fingers.

- Partial fixed flexion deformity of the right index finger.

- Dermoscopy shows well-defined white structureless areas with overlying multiple follicular plugs (black star). There are a few ill-defined shiny, whitish linear streaks within the white structureless area known as chrysalis-like structures (blue arrow and black arrow) (Dermlite 4, non-polarising mode, 20x).

- Thinned-out atrophic epidermis with hyperkeratosis, follicular plugging, sclerosis and dense homogenisation of the collagen reaching up to the deep reticular dermis and interstitial lymphocytic infiltrate. (Haematoxylin and eosin, 40x).

- Mild interstitial lymphocytic inflammatory infiltrate is noted in the dermis interspersed within the zone of homogenised collagen bundles. (Haematoxylin and eosin, 100x).
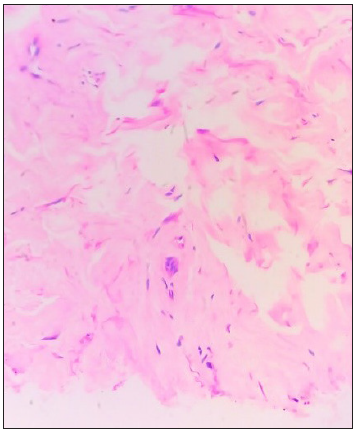
- Homogenisation of the collagen noted up to the deeper dermis with mild interstitial lymphocytic infiltrate. (Haematoxylin and eosin, 200x).
LS is an inflammatory disorder of unknown aetiology with both genital (85%) and extragenital involvement (15%–20%).1 Extragenital LS commonly involves the upper trunk, shoulders and neck as ivory-white opalescent papules which often coalesce to form plaques and later lead to a thin parchment-like skin.1 Other less common morphologies reported in the literature are guttate, bullous, haemorrhagic, zosteriform, annular and linear forms.1 Morphea usually presents as erythematous to hyperpigmented indurated plaques with characteristic violaceous to erythematous rim around the lesions. Other presentations include nodular, plaque, guttate, linear, bullous morphea, etc.2 The association of LS with morphea is still controversial. Few authors suggest that LS is a subtype of morphea involving the papillary dermis and is therefore often referred to as subepidermal morphea. Others suggest that both are manifestations of the same disease as they share many similar clinico-pathologic findings with morphea having more chances of systemic association. It has been described that almost 5% of morphea patients have coexistent LS within the same lesion.3 There are reports of conversion of LS to morphea or vice versa on consecutive skin biopsies.1 However, many researchers suggest that both are distinct diseases with few differentiating features between both diseases and the presence of both in the same lesion is merely coincidental.1
Histologically, LS is characterised by follicular plugging, hyperkeratosis, epidermal atrophy, basal cell vacuolar degeneration and homogenisation of collagen mainly in the papillary dermis. On the other hand, morphea is characterised by the homogenisation of collagen and thickened collagen bundles in the deeper dermis i.e., till the reticular dermis. There is lymphocytic interstitial infiltrate and trapped adnexa leading to decreased appendages in morphea.4
Dermoscopy findings of lichen sclerosus include whitish-yellow patches, keratotic follicular plugs, linear or dotted vessels, scaling, haemorrhagic spots and chrysalis-like structures. These are shiny, bright white orthogonal linear streaks.5 Morphea on dermoscopy reveals white structureless areas named fibrotic beams. These fibrotic beams are usually smaller, more opaque and have less defined margins than the whitish patches seen in LS. Morphea, in addition, can also have structureless or reticular brownish areas and linear branching vessels which cross the white fibrotic beams.5
The coexistence of lichen sclerosus and morphea within the same lesion has been described in a few cases in the literature, however, none of the reports showed the acral area to be involved.4,6,7 We were unable to find any reports that have described its annular or serpentine form. Also, LS - morphea overlap at acral sites leading to deformity of fingers was unique. Awareness regarding such presentation is important because early diagnosis and treatment can significantly improve patient outcome and can prevent disease progression.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Extragenital lichen sclerosus: A comprehensive review. Aust J Dermatol. 2022;63:452-62.
- [CrossRef] [PubMed] [Google Scholar]
- Morphea: The 2023 update. Front Med. 2023;10:1108623.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Coexistence of lichen sclerosus and morphea: A retrospective analysis of 472 patients with localized scleroderma from a German tertiary referral center. J Am Acad Dermatol. 2012;67:1157-62.
- [CrossRef] [PubMed] [Google Scholar]
- Histopathological coexistence of extragenital lichen sclerosus and morphea in a single lesion. Cureus. 2020;12:e12215.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopy of morphea and cutaneous lichen sclerosus: Clinicopathological correlation study and comparative analysis. Dermatology. 2018;233:462-70.
- [CrossRef] [PubMed] [Google Scholar]
- Coexistence of lichen sclerosus et atrophicus and morphea in the same lesion: A case report. Cureus. 2023;15:e43062.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Concomitance of lichen sclerosus et atrophicus and morphea in the same lesions. J Eur Acad Dermatol Venereol. 1994;3:407-10.
- [Google Scholar]





