Translate this page into:
Severely disfiguring multiple familial trichoepitheliomas with basal cell carcinoma
2 Department of Pathology, Imam Khomeini Hospital, Jondishapur University of Medical Sciences, Ahvaz, Iran
3 Department of Clinical Pharmacy, Faculty of Pharmacy, Tehran University of Medical Sciences, Tehran, Iran
Correspondence Address:
Amin Karimzadeh
Department of Dermatology, Imam Khomeini Hospital, Jondishapur University of Medical Sciences, Ahvaz
Iran
| How to cite this article: Mapar MA, Ranjbari N, Afshar N, Karimzadeh I, Karimzadeh A. Severely disfiguring multiple familial trichoepitheliomas with basal cell carcinoma. Indian J Dermatol Venereol Leprol 2014;80:349-352 |
Sir,
Trichoepitheliomas are benign adnexal neoplasms that originate from hair follicles. It can present as solitary non-familial or multiple familial forms. Multiple familial trichoepitheliomas is an autosomal dominant disorder characterized by numerous nodules and papules predominantly on the face and occasionally on the scalp. [1] Herein, we describe a rare case of this condition, with severe facial disfigurement, involving 6 members of a family in three generations. In the oldest affected member, one of the lesions evolved into a basal cell carcinoma.
A 55-year-old, rural housewife of Arabian descent presented with slowly progressive facial skin lesions since 37 years. She had noticed her skin lesions at the age of 18 years and they gradually increased in size and number. Although she had sought no medical advice for her asymptomatic lesions during these years (due to her low socio-economic status), her disfigured face resulted in social isolation. As one of her skin lesions became pruritic and ulcerated recently, she sought medical attention. Physical examination revealed numerous painless, round-to-oval, discrete and/or confluent, soft and firm, skin-colored or pinkish, papules and nodules ranging from 1 to 5 cm in size. These lesions covered the whole face but were predominantly clustered on her peri-nasal and chin areas. In the peri-nasal area, a solitary, 4 cm-sized, ulcerated nodule with telangiectasiae was also detected. In addition, a 4 × 3 cm, ulcerated, severely pruritic lesion was noted on her forehead [Figure - 1]. No areas of hypopigmentation were found on the skin lesions. The patient also denied ocular and skeletal problems. Dermatologic examination of the rest of her body was unremarkable. The patient had no significant underlying medical disease and had received no medications or herbal supplements.
 |
| Figure 1: Numerous skin-colored or pinkish, papules and nodules on the peri-nasal and chin areas along with a ulcerated nodule in the peri-nasal area and an, ulcerated, severely pruritic lesion on the forehead (highlighted with arrows) |
Biopsy from asymptomatic, non-ulcerated lesions in the peri-nasal area showed dermally located islands of basaloid cells with peripheral palisading, abortive hair follicle and keratinous cysts lined by squamous epithelium along with increased fibroblastic cells and stromal fibrosis [Figure - 2]a. Excisional biopsy of the ulcerated skin lesion in the peri-nasal area [Figure - 2]b revealed a neoplasm composed of nests of basaloid cells that originated from the overlying epidermis along with stromal retraction. In view of the patient′s history and clinical presentation, the histopathology was suggestive of a basal cell carcinoma. Immunohistochemical staining for three immunomarkers including CD10, CD34 and bcl-2 was performed on the two different skin lesions suspected to be trichoepithelioma and basal cell carcinoma. CD10 and bcl-2 markers were undetectable on the trichoepithelioma. By contrast, bcl-2 diffusely stained tumor nests and CD10 was detected in the periphery of basaloid cells of the lesion suspected to be basal cell carcinoma. In addition, CD34 stained neither the trichoepithelioma nor basal cell carcinoma [Figure - 3].
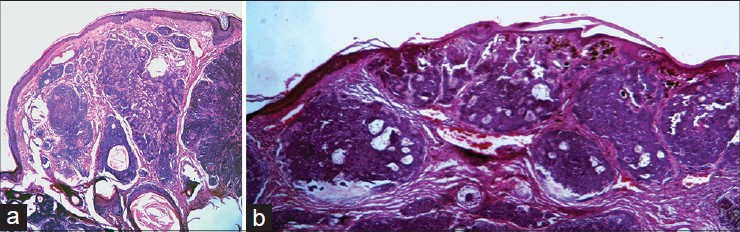 |
| Figure 2: Biopsy of the lesion in the peri-nasal area (H and E, original magnifications, ×10). (a) Island of basaloid cell with peripheral palisading and keratinocyte formation and horn cyst within the dermis, (b) basaloid cell origin from the epidermis with stromal retraction |
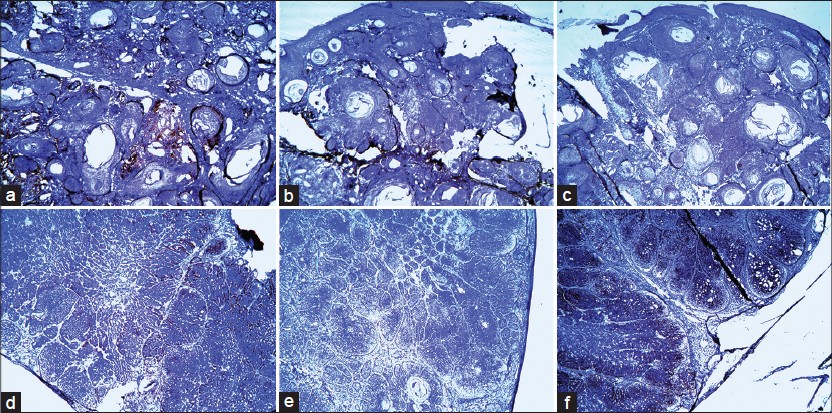 |
| Figure 3: Immunohistochemical staining for CD10, CD34 and bcl-2 on two different skin lesions suspected of trichoepitheliomas (a-c) and basal cell carcinoma (d-f). Original magnifications, ×4 |
The patient had 6 sons and 2 daughters. Two out of the six sons developed similar tiny dome-shaped lesions on their faces and forehead at ages 34 and 40 years that had been surgically excised. As they lived abroad, we had no access to their medical data including histopathology reports. Her other four sons and two daughters were unaffected. Interestingly, three grandsons aged 17, 21 and 25 years were affected with skin lesions that began at the ages 13, 15 and 19 years, respectively and were similar to those of their grandmother except that they did not have basal cell carcinoma. Their general health was good. The histopathology of lesions in the grandsons was suggestive of trichoepithelioma. The pedigree of the patient′s family is depicted in [Figure - 4]. The clinical manifestations, histopathological findings and family history provided confirmation of the diagnosis of multiple familial trichoepitheliomas.
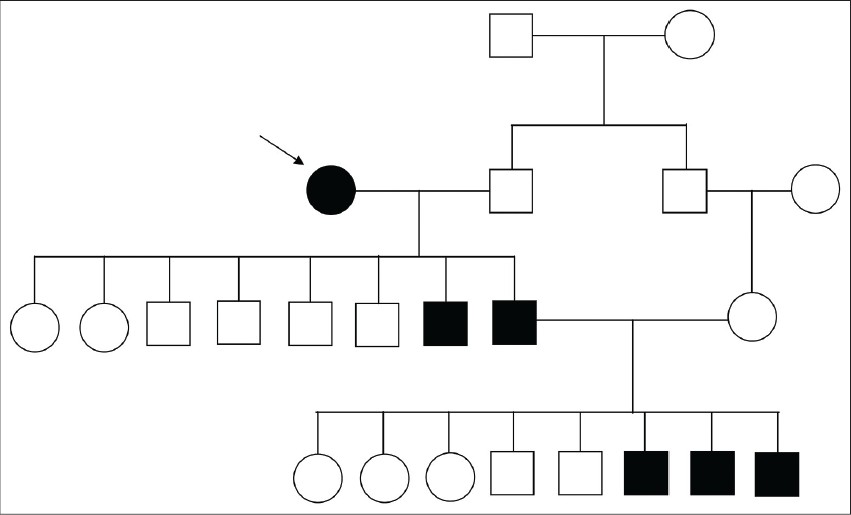 |
| Figure 4: Pedigree of the patient's family. Males and females are indicated by squares and circles, respectively. The patient (grandmother) is identified by the arrow. Probable involvement of the patient's parents and siblings with similar skin lesions (trichoepitheliomas) was unknown. The patient's husband and his family including the parents and the brother were unaffected |
Solitary rather than multiple familial trichoepitheliomas usually share microscopic features with basal cell carcinoma especially in small biopsies. [2] Several histopathological features suggesting a diagnosis of trichoepitheliomas over basal cell carcinoma have been described such as fibrocytic loss of stroma, aggregations with smooth borders, granulomatous inflammation, monomorphic nuclei and papillary mesenchymal bodies. [3] In the present case, histopathological findings (nests of basaloid cells originating from the overlying epidermis with stromal retraction) along with clinical manifestations (ulceration, telangiectasias and peripheral rolled edges) of the skin lesion at the peri-nasal area were in favor of basal cell carcinoma.
Genetic mutations such as those in the cylindromatosis tumor suppressor gene (CYLD) have been associated with multiple familial trichoepitheliomas. Brooke-Spiegler syndrome, characterized by different combinations of inherited adnexal neoplasms including multiple trichoepitheliomas, cylindromas and spiradenomas, is also linked to the CYLD gene. This finding suggests that cylindromas, spiradenomas and multiple familial trichoepitheliomas are phenotypic variations of a single genetic defect. [4] Unfortunately, genetic analyses were not carried out for any members of our reported family including the grandmother, her offspring and grandchildren. However, since cylindromas and/or spiradenomas were not seen in the biopsies of our patients, Brooke-Spiegler syndrome is unlikely.
Immunohistochemical staining technique may also help to distinguish between basal cell carcinoma and multiple familial trichoepitheliomas using antibodies against a number of immunomarkers such as CD34, bcl-2, androgen receptor, transforming growth factor-β and CD10. [2] The diffuse pattern of bcl-2 staining in our patient′s basal cell carcinoma was in accordance with previous reports. [5] However, a study has questioned the reliability of bcl-2 in distinguishing multiple familial trichoepitheliomas from basal cell carcinoma. [6] It has been reported that CD10 stains the basaloid cells in basal cell carcinoma while it stains the stroma in multiple familial trichoepitheliomas and may be a useful immunohistochemical marker in differentiating these two entities. [7] In our case, only the peripheral basaloid cells stained strongly with CD10 in the basal cell carcinoma while staining was completely undetectable in the trichoepitheliomas. Lack of CD34 staining in both lesions was in contrast to the study conducted by Illueca et al. [8] that reported CD34 expression in multiple familial trichoepitheliomas but not in basal cell carcinoma. Taken together, as in other reports, [9],[10] the immunomarkers used in our patient were not very helpful in differentiating these two conditions. Immunostaining with relatively novel markers such as androgen receptor, transforming growth factor-β, p75 neurotrophin receptor and pleckstrin homology-like domain, family A, member 1, (not currently available in our laboratory) may be more useful in this regard.
Trichoepitheliomas can undergo transformation to malignant neoplasms such as basal cell carcinoma. [1] According to Pincus et al. (2008), six English language reports have appeared from 1959 to 2008 describing eleven patients who developed this malignant neoplasm from multiple familial trichoepitheliomas. Cases of sporadic trichoepitheliomas associated with basal cell carcinoma have also been reported. In four of the above reports, patients presented when the lesions started to bleed and/or ulcerate. [9] Interestingly, one of our patients (the grandmother) sought medical attention because of ulceration and pruritus in a lesion. The history, clincal features, histopathological and immunohistochemistry findings were suggestive of the evolution of basal cell carcinoma directly from trichoepithelioma in our case. Clinicians should examine these patients carefully and be vigilant about any rapid growth or ulceration in the pre-existing lesions that may indicate malignant transformation. [9]
| 1. |
Calonje E. Tumors of the skin appendages. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Chichester: Wiley-Blackwell; 2010.
[Google Scholar]
|
| 2. |
Poniecka AW, Alexis JB. An immunohistochemical study of basal cell carcinoma and trichoepithelioma. Am J Dermatopathol 1999;21:332-6.
[Google Scholar]
|
| 3. |
Ackerman AB, Reddy VB, Soyer HP. Neoplasms with Follicular Differentiation. New York: Ardor Scribendi; 2001.
[Google Scholar]
|
| 4. |
Young AL, Kellermayer R, Szigeti R, Tészás A, Azmi S, Celebi JT. CYLD mutations underlie Brooke-Spiegler, familial cylindromatosis, and multiple familial trichoepithelioma syndromes. Clin Genet 2006;70:246-9.
[Google Scholar]
|
| 5. |
Verhaegh ME, Arends JW, Majoie IM, Hoekzema R, Neumann HA. Transforming growth factor-beta and bcl-2 distribution patterns distinguish trichoepithelioma from basal cell carcinoma. Dermatol Surg 1997;23:695-700.
[Google Scholar]
|
| 6. |
Abdelsayed RA, Guijarro-Rojas M, Ibrahim NA, Sangueza OP. Immunohistochemical evaluation of basal cell carcinoma and trichepithelioma using Bcl-2, Ki67, PCNA and P53. J Cutan Pathol 2000;27:169-75.
[Google Scholar]
|
| 7. |
Heidarpour M, Rajabi P, Sajadi F. CD10 expression helps to differentiate basal cell carcinoma from trichoepithelioma. J Res Med Sci 2011;16:938-44.
[Google Scholar]
|
| 8. |
Illueca C, Monteagudo C, Revert A, Llombart-Bosch A. Diagnostic value of CD34 immunostaining in desmoplastic trichilemmoma. J Cutan Pathol 1998;25:435-9.
[Google Scholar]
|
| 9. |
Pincus LB, McCalmont TH, Neuhaus IM, Kasper R, Oh DH. Basal cell carcinomas arising within multiple trichoepitheliomas. J Cutan Pathol 2008;35 Suppl 1:59-64.
[Google Scholar]
|
| 10. |
Arits AH, Parren LJ, van Marion AM, Sommer A, Frank J, Kelleners-Smeets NW. Basal cell carcinoma and trichoepithelioma: A possible matter of confusion. Int J Dermatol 2008;47 Suppl 1:13-7.
[Google Scholar]
|
Fulltext Views
3,665
PDF downloads
1,816





