Translate this page into:
Sirolimus in dermatology: Jack of many trades
Corresponding author: Dr. Rahul Mahajan, Department of Dermatology, Post Graduate Institute of Medical Education and Research Chandigarh, Chandigarh, India. drrahulpgi@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Singh S, Sharma A, Malhi K, De D, Handa S, Mahajan R, et al. Sirolimus in dermatology: Jack of many trades. Indian J Dermatol Venereol Leprol. 2025;91:S32-S34. doi: 10.25259/IJDVL_869_2023
Dear Editor,
Phosphoinositide 3-kinase/protein kinase B/mammalian target of rapamycin (PI3K/AKT/mTOR) pathways are downstream signalling pathways involved in a variety of pathologic processes in dermatology. Sirolimus, an mTOR pathway inhibitor, is used for vascular malformations like Klippel Trenaunay syndrome (KTS) and Blue Rubber Bleb Naevus syndrome (BRBNS). 1 Apart from this, some studies have reported the use of topical sirolimus in tuberous sclerosis, fibrofolliculomas, and port wine stains previously, with inconsistent results. 2 In this case series, we assess the efficacy and safety of oral and topical sirolimus in various dermatological disorders across six paediatric patients in northern India [Table 1]. Topical 0.1% sirolimus was formulated with 100 tablets of 1 mg strength in 100 g of petrolatum. 3
| Case number | Demographics | Clinical indication | Formulation and concentration used | Treatment outcome | Response time | Side effects |
|---|---|---|---|---|---|---|
| Case 1 | 12-year-old male | Klippel Trenaunay syndrome | Oral sirolimus at dose of 0.8 mg/m2 | Decrease in pain and hypertrophy demonstrated both clinically (reduction in mid-arm circumference) as well as radiographically | 10 months | Transient leukopenia |
| Case 2 | 13-year-old female | Blue rubber bleb naevus syndrome | Oral sirolimus at dose of 0.6 mg/m2 | Non-progression of existing lesions, absence of bleeding, and new lesions | 6 months | None |
| Case 3 | 2-year-old male | Sturge-Weber syndrome with a facial port-wine stain | Topical sirolimus 0.1% twice daily | Significant reduction in erythema and edema | 6 weeks | Mild local site irritation |
| Case 4 | 18-year-old female | Neviform/ multisegmental angiokeratoma | Topical sirolimus 0.1% twice daily | Substantial improvement in the overall appearance of the lesions (decrease in angiomatous and keratotic components) | 3 months | None |
| Case 5 | 15-year-old female | Trichoepithelioma | Topical sirolimus 0.1% twice daily | A decrease in the size of the papules was seen when compared with the baseline | 2 months | None |
| Case 6 | 10-year-old female | Adenoma sebaceum | Topical sirolimus 0.1% twice daily | Substantial clearance of the lesions (decrease in angiomatous and fibrous components) | 3 months | None |
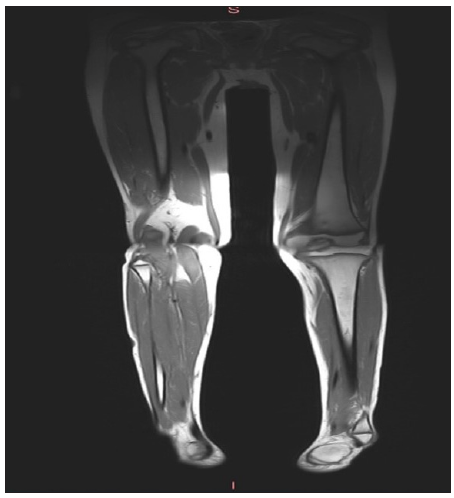
Our first patient was a 12-year-old boy of KTS with type 2 Phacomatosis Pigmentovascularis (PPV) who presented with painful, excessive growth on the right side of the body and pink-purple stains over the right side of the face associated with naevus of Ota over the right sclera [Figure 1a]. Magnetic resonance imaging (MRI) of soft tissues revealed diffusely increased girth of the right extremities with multiple prominent superficial venous channels [Figure 1b]. Oral sirolimus (0.8 mg/m2) was initiated due to refractory symptoms. After approximately 10 months, significant clinical and radiological improvement was observed [Figure 1c].

-
Facial port wine stain, naevus of Ota, and right-sided facial hypertrophy in a patient of Klippel Trenaunay Syndrome with phacomatosis pigmentovascularis.
-
T1-weighted MRI of lower limbs demonstrating soft tissue and muscular hypertrophy of right lower limb.

-
MRI of lower limbs after 10 months of Sirolimus therapy showing no significant soft tissue hypertrophy.
The 2nd case was of a 13-year-old girl who presented with multiple bluish compressible swellings over her body since 1 year of age associated with bleeding. MRI of the right knee revealed multiple venous malformations. Based on clinical and investigational data, she was diagnosed with a case of BRBNS with iron deficiency anaemia. Given the refractory and extensive nature of the disease, she was started on sirolimus in 2014 at a dose of 0.6 mg/m2 with a notable improvement in the form of non-progression of existing lesions, absence of bleeding, and new lesions.
The third patient, a 2-year-old boy diagnosed case of Sturge-Weber syndrome with facial port-wine stain (PWS) [Figure 2a] showed significant improvement after 6 weeks of topical sirolimus 0.1%, with reduced erythema and edema [Figure 2b].

-
2-year-old boy diagnosed case of Sturge-Weber syndrome with facial port wine stain.

-
After 6 weeks of treatment with topical sirolimus 0.1%, a significant reduction in the erythema was appreciated.
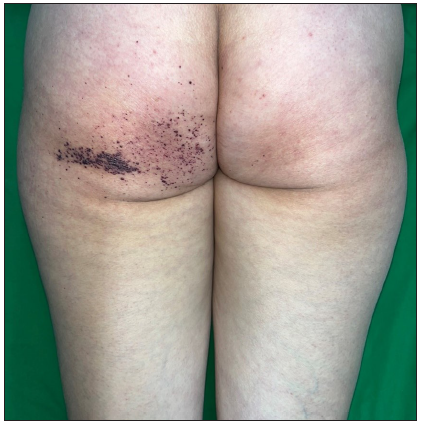
Our fourth case was that of a 17-year-old female, who had multiple erythematous, keratotic papules on her right buttock [Figure 3a], the dermoscopic evaluation showed dark blue and red lacunae with a whitish veil, histological examination showed hyperkeratosis and numerous thin-walled dilated blood vessels leading to a diagnosis of neviform/multisegmental angiokeratoma. Fabry’s disease was considered and excluded due to a lack of specific features. Following 3 months of topical 0.1% sirolimus, there was a substantial reduction in the overall appearance of the lesions [Figure 3b].

-
Multiple, discrete, erythematous, keratotic papules on her right buttock extending to her leg in a segmental distribution.
-
Following 3 months of initiation there was a substantial reduction in the overall appearance of the lesions.
The other two cases treated with topical sirolimus were that of multiple trichoepitheliomas in a 15-year-old girl and adenoma sebaceum in a 10-year-old girl. The details are given in Table 1.
PI3K/AKT/mTOR pathways are crucial in vascular morphogenesis, evident in mutations associated with vascular anomalies. KTS, a rare disorder with PIK3CA mutations, features capillary, venous, and lymphatic malformations with limb overgrowth. 4 Traditional management involves surgical excision and interventions like sclerotherapy, but these may be ineffective. Sirolimus shows promise in refractory cases. 5 Our case demonstrated pain reduction and near-complete resolution of limb hypertrophy after 10 months of sirolimus therapy.
BRBNS, resulting from TEK gene mutations, causes dysregulation in mTOR signalling pathways. 6 It leads to recurrent venous malformations in the skin and gastrointestinal tract, with a risk of life-threatening bleeding. 6 Sirolimus is effective in some cases due to its anti-angiogenic properties, but it’s not curative, as lesions recur upon therapy withdrawal.
Topical sirolimus is a new and rather less commonly used preparation in clinical practice in dermatology. Due to the lack of a commercially accessible FDA-approved topical formulation, compounding pharmacies make sirolimus creams, ointments, and gels. The effectiveness of topical sirolimus for PWS has previously been evaluated in four studies (2 randomised controlled trials (RCTs) and 2 observational studies), involving 47 patients. In all the studies, it was administered as an adjuvant therapy to pulsed dye laser (PDL) treatment. Efficacy results in these studies show heterogeneous outcomes in terms of improvement. 7 Angiokeratoma, PWS, and trichoepithelioma are rather less reported dermatological conditions where topical sirolimus has been tried in our case series. 7
Our limited experience with topical sirolimus which was compounded in our setup has supported the efficacy of this agent in treating multiple dermatological conditions without any significant side effects that can warrant discontinuation of therapy.
Concluding, sirolimus demonstrates efficacy in diverse dermatological conditions, emphasising its versatility and potential as a standalone therapy, particularly in paediatric cases with challenging presentations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Sirolimus is efficacious in treatment for extensive and/or complex slow-flow vascular malformations: A monocentric prospective phase II study. Orphanet J Rare Dis. 2018;13:191.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Topical rapamycin as a treatment for fibrofolliculomas in Birt-Hogg-Dubé syndrome: A double-blind placebo-controlled randomized split-face trial. PLoS One. 2014;9:99071.
- [CrossRef] [PubMed] [Google Scholar]
- Topical sirolimus: Difference between compounded preparations and commercial oral solution. Pediatr Dermatol. 2021;38:967-9.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular anomalies classification: Recommendations from the international society for the study of vascular anomalies. Pediatrics. 2015;136:203-14.
- [CrossRef] [PubMed] [Google Scholar]
- Rapamycin: Something old, something new, sometimes borrowed and now renewed. Clin Pharmacol Ther. 2007;82:381-8.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term sirolimus treatment in blue rubber bleb nevus syndrome: Case report and review of the literature. Pediatr Dermatol. 2021;38:464-8.
- [CrossRef] [PubMed] [Google Scholar]
- Topical use of mammalian target of rapamycin inhibitors in dermatology: A systematic review with meta-analysis. J Am Acad Dermatol. 2019;80:735-42.
- [CrossRef] [PubMed] [Google Scholar]






