Translate this page into:
Skin camouflage therapy
Corresponding author: Dr. Jasleen Kaur Sandhu, Department of Dermatology, Venereology and Leprology, Government Medical College & Hospital, Chandigarh, India. jasleensandhu21@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Sandhu JK, Sharma P. Skin camouflage therapy. Indian J Dermatol Venereol Leprol 2022;88:717-23.
Abstract
Camouflage is defined as a combination of materials, colouration or illumination for concealing something. Skin camouflage therapy is the use of specially formulated products to conceal skin diseases and disfigurements, with the goal of giving a temporarily normal appearance. It gives immediate relief in various dermatological disorders, especially those affecting the visible areas, which are known to be associated with profound psychosocial impact. Despite considerable evidence for its emotional benefits, its utilisation among dermatologists in clinical practice remains low. This article is intended to familiarise dermatologists with the use of skin camouflage therapy including its availability, indications, contraindications, techniques, limitations and future trends.
Keywords
Cosmetic camouflage
skin camouflage therapy
medical makeup
visible skin lesions
disfigurement
Introduction
Physical appearance is an influential factor in personal, social and professional interactions. Dermatological diseases associated with altered skin appearance or disfigurement may cause social stigma, low self-esteem and reduced quality of life. The impact is more when these diseases involve visible areas of the body. Though advances in dermatology have immensely helped to tackle these, there are many conditions that still elude effective solutions. Further, all medical, surgical or laser treatments require time to show results. This lack of immediate and uniformly adequate clinical results with dermatological therapies poses a challenge, especially when patients expect quick and complete results with ‘modern’ therapies. Sometimes cosmetic complications like erythema, hyper- and hypo-pigmentation may arise because of dermatological procedures, adding to the distress of patients and dermatologists alike. Skin camouflage therapy is an effective tool to achieve instant relief in these scenarios and all dermatologists should have at least a basic knowledge of skin camouflage therapy.
Camouflage, derived from the French word ‘camoufler’ which means ‘to blind,’ is defined as a combination of materials, colouration, or illumination that alters or obscures appearance in order to conceal something.1 The goal of skin camouflage therapy is temporary normalisation of the appearance of patients disfigured by scarring or disease, with the help of specially formulated cosmetic preparations [Figures 1a and b].2 It is recognised as a sub-medical branch of dermatology and plastic surgery and has been given different names like ‘medical make-up’ and ‘cosmetic camouflage’ in the past. The term ‘skin camouflage therapy’ is recommended to decrease the reluctance to its use in men, as cosmetics and make-up have traditionally been associated with women.
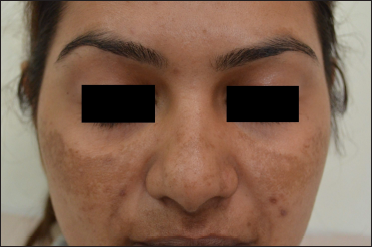
- Melasma, face (Before skin camouflage therapy)

- Melasma, face (After skin camouflage therapy)
History
Plastic surgeons associated with the British Royal Air Force first used skin-coloured preparations to conceal scars and thus improve the appearance of pilots who had sustained burn injuries during World War II.3 A patient support group, the ‘Guinea Pig Club’ was established by Sir Archibald McIndoe, who was a plastic surgery consultant to the Royal Air Force. Members of this group used to try camouflage creams prepared by Thomas Blake, a chemist from the company ‘Veil Cover Cream’.3 In 1954, Joyce Allsworth started the camouflage practice within the British Red Cross and established the British Association of Skin Camouflage.4 Over the years, the range of colours and shades of Veil Cover Cream products expanded and the market for cosmetic camouflage products grew tremendously with increased awareness and demand. Many countries have associations of camouflage therapists who are trained and licensed specifically for this work. For example, in the United Kingdom, camouflage services can be sought through the British Association of Skin Camouflage, the Skin Camouflage Network and organisations like the Red Cross Camouflage Service and Changing Faces.5 In some dermatology departments, camouflage lessons by volunteers who are specialists in camouflage are held to educate patients.6 Dermatologists there introduce patients with various dermatoses to the option of camouflage and motivate them to attend the special camouflage clinic for lessons on the precise procedure and to obtain a suitable colour match.
Indications in dermatology
Ideally, the option of skin camouflage should be offered to all patients with lesions in visible areas unless contraindicated. Table 1 lists common dermatological indications for skin camouflage. Camouflage therapy can be applied 7-10 days after most surgical procedures. However, premature use following epidermal damage may invite secondary infection, hence it should be used with caution in such situations.7
| Type of disorders | Indications |
|---|---|
| Pigmentary disorders | |
| Hyperpigmentary disorders | Melasma Acquired dermal macular hyperpigmentation Periorbital melanosis Freckles and lentigines Café-au-lait macules Nevi, e.g., Becker’s nevus, nevus of Ota, nevus of Hori, speckled nevus Tattoos Post-inflammatory hyperpigmentation Morphea |
| Hypopigmentary disorders | Vitiligo Idiopathic guttate hypomelanosis Post-inflammatory hypo/depigmentation Lichen sclerosus et atrophicus Leprosy |
| Vascular disorders | Capillary malformations, e.g., port-wine stain Hemangioma Rosacea Telangiectasias Post-procedure erythema |
| Scars and scarring disorders | Post-traumatic/post-surgical scars Post-inflammatory scars, e.g., acne scars Burns Discoid lupus erythematosus Striae Keloids/Hypertrophic scars |
| Miscellaneous | Acne Lupus erythematosus Systemic sclerosis Xeroderma pigmentosum Psoriasis vulgaris Pigmented purpuric dermatoses Dermatosis papulosa nigra Postoperative bruising |
Contraindications
Patients with hypersensitivity to camouflage products or their ancillary components such as fragrances or preservatives, open wounds or erosions, those with active dermatitis or infection at the camouflage site, undiagnosed skin rashes and suspicious, pre-malignant or malignant lesions form the contraindications to cosmetic camouflage.8
Cosmetic camouflage products
An ideal skin camouflage product should possess the following characteristics9:
Colour: Camouflage make-up must match all ethnic skin tones and nuances; thus it should be available in a multiplicity of shades.
Opacity: Camouflage make-up must veil all types of skin discolouration, giving a natural appearance.
Inertness: Camouflage products should ideally be non-allergenic, non-comedogenic and non-photosensitising.
Waterproof and sweat-resistant: Camouflage makeup must be impervious to water and should not get smudged due to sweating.
Longer wear: It must provide the convenience of being worn comfortably for long, with easy reapplication if needed.
Holding power: It must adhere to the skin without sliding off.
Ease of application/removal: It must be easy to apply without complicated colours and steps of application and easy to remove with non-alcohol/acetone-based products.
Sun-screening capacity: Ideally, a camouflage product should have a good, homogeneous sun-protection capacity. Because of their pigment content (iron oxide, titanium dioxide, kaolin) and opacity, camouflage products usually provide a sun protection factor (SPF) of 3-4, which can be further enhanced by increasing the pigment content.
Cost-effectiveness: This is an important factor influencing the regular use of a cosmetic product.
Commercially marketed camouflage products are available in different formulations like creams, liquids (both creamy and alcohol-based), roll-ons and sticks. There are a variety of skin tones to give an exact colour match and also colour correctors to give complete concealment. These products have up to 25% more pigment content than common make-up foundations, as well as fillers with optical properties; they are formulated so that a single application lasts at least a whole day.2 Their pigment content makes these products opaque and better able to disguise underlying abnormalities than normal make-up cosmetics can. Many patients with dermatoses in visible areas try to hide them with ordinary make-up cosmetics, with suboptimal results. It is the role of the dermatologist to introduce such patients to specially formulated camouflage products and to guide them in their use. Skin camouflage gives the patient the freedom to apply the product when required - this may be on a daily basis or just for special occasions. Table 2 lists the different brands of skin camouflage products available in India. Out of these, Dermacolor and Microskin are more easily available, with their products costing around INR 900 (12$) to 3000 (40$).
| Product | Manufacturer/company | Availability in India - offline | Availability in India - online |
|---|---|---|---|
| Dermacolor | Kryolan Professional Make-up | In select cities through company representative | https://in.kryolan.com/ |
| Microskin | Microskin Solutions | In select cities through company representative | http://microskinindia.com/ |
| Zanderm wide and precision applicators | Zanderm | No | https://zanderm.in/ |
| Veil Cover Cream | Thomas Blake Cosmetic Creams | No | Online retail websites |
| Dermablend Cover Creme Foundation | Dermablend | No | Online retail websites |
Pre-camouflage counselling
Patients need to be counselled about skin camouflage, its benefits and its limitations. While assessing their expectations, it is prudent to explain to the patient about the adjuvant nature of skin camouflage. It is important to note that camouflage is most effective when applied over skin with discolouration rather than surface abnormalities, irrespective of the size of the defect. In dermatoses with associated surface irregularities, the patient should be counselled that the appearance will improve but complete camouflage may not be possible. The patient should be taught the steps involved in camouflage, keeping in mind hobbies, occupation, usual outdoor activities and other topical agent use. Although the camouflage products contain sun protection by virtue of presence of titanium dioxide and zinc oxide, additional oil free sunscreen can be applied under and over the camouflage, when indicated. Normal make-up can be worn after application of camouflage and topical medication and emollients can be applied before the camouflage.
Pre- and post-camouflage photographic documentation should be a rule. The authors have found that only verbal information about this option may not convince patients to adopt it. But once a practical demonstration is provided and they see the immediate effect of the skin camouflage on their appearance, patients are more willing to accept it.
Technique
The technique of camouflaging is a pertinent factor affecting the final outcome. It is important that all shades are tested on the patient’s skin directly, as the colour in the container may not be the same as the perceived colour when the product is applied to the skin. The foundation colour must be selected in natural sunlight as artificial fluorescent lights alter colour perception, leading to choosing a shade darker than appropriate.10
Skin camouflage cream is applied on clean moisturised skin. It can be applied with sponges or with fingers. While teaching application it should be emphasised that camouflage creams are applied by dabbing or tapping and not by rubbing as the latter would result in removing the cream. Some brands advocate the use of airbrush devices that spray a thin mist uniformly over the skin.
The basic approach to camouflage includes concealing, colour correction, contour correction or a combination of all three methods.8 Concealing is a simple application of skin-matched camouflage product and it works well for light discolourations like epidermal melasma, freckles, faint erythema or scars. In deeper coloured dermatoses like vascular malformations, dermal/mixed melanoses and bruises, a preliminary step of colour correction is needed before concealing. Colour correction is the application of a neutralising colour corrector cream according to the type of discolouration. Application of only skin-matched cover creams without neutralisation may not give complete concealment, as is seen in vitiligo and other dermatoses with higher contrast to normal skin [Figures 2a and b]. Also, in dermal pigmentation and bluish vascular anomalies, just skin-coloured cover ends up giving unnatural ashy greyish hues. For colour correction, according to the colour of the dermatosis, an appropriate colour corrector is chosen using the complementary colour wheel [Figure 3]. According to colour theory, opposite colours on the wheel cancel each other out by an optical effect. The opposite colour of blue is orange and that of purple is yellow, therefore, bluish or purplish lesions like periorbital dark circles, bruises and veins are neutralised by an orange or yellow-hued corrector. An orange colour corrector also works to conceal many hyperpigmentary conditions like dermal/mixed melasma and other dermal facial melanoses which most often appear to be ashy or greyish brown because of the deep pigment and resultant Tyndall effect. It has to be ensured that the colour of the corrector used is of the same lightness or darkness of the skin, for example, a lighter orange for a lighter skin tone and a darker orange for darker skin tones. The opposite colour of red is green, thus a green colour neutraliser is used for reddish discolourations like vascular nevi, rosacea, post-acne or post-procedure erythema, recent scars and immature striae. White is not there on the wheel, but the opposite colour of white is black, therefore the neutralising colour corrector for the white skin of vitiligo is very dark brown, close to black [Figures 2c and d]. Once discolouration is disguised with the colour correction technique, the second step is the application of a skin-coloured camouflage cream matched to the patient’s tone over the affected area by the dabbing method. It is important to blend the outer edges to fade unnoticeably into the surrounding skin. On the face, it is sometimes needed to apply a thinner layer of camouflage cream over the whole face including the unaffected areas to give a uniform appearance.
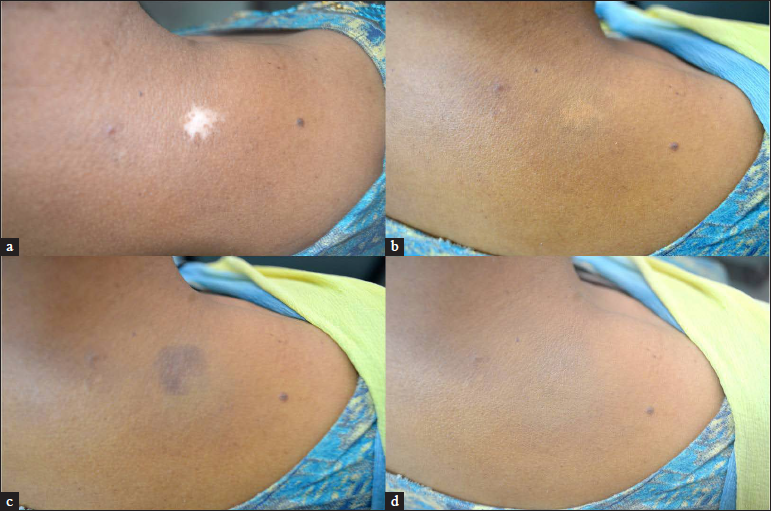
- (a and b) Vitiligo patch pre- and post-application of only matching skin tone giving partial concealment, (c and d) vitiligo patch with colour correction using a dark brown tone and then application of matching skin tone, providing complete concealment
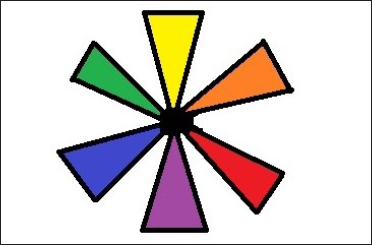
- Complementary colour wheel
Using colour correction as above with neutralising correctors is a controversial subject. Some experts think it helps neutralise undesirable skin discolouration while others believe that the use of colour corrector only adds a third colour.11,12 The authors have found that, while using the camouflage brand Dermacolor, the neutralisation step is needed and helps in giving a more natural result. But the authors concede that if the opacity of the camouflage product is increased, it may be possible to skip this step.
The third camouflage technique of contour correction is needed only when the dermatosis has surface irregularities. Contouring creates new dimensions using light and dark shades. For depressed lesions, a highlighter that is one to two shades lighter than the skin is utilised on the indented areas. Light colours give the illusion of pulling forward where applied, giving the indented areas the illusion of a shallower, smoother appearance. Highlight can be in the form of a cream concealer applied with a synthetic brush or a concealing pencil used to draw in the indented areas. Conversely, for raised areas, a shade of product slightly darker than the skin should be applied. Dark colours give the illusion of recession where applied, providing the raised areas with the illusion of a smoother appearance. The same technique may be used to camouflage puffy areas. Applying foundation with an airbrush is also very beneficial for patients with raised scars because an airbrush compressor blows an ultrafine mist onto the skin. This allows the textured skin areas to get a very even coat of colour, whereas old-fashioned ‘by hand’ application applies the most pressure to raised areas, which is counterproductive.
After camouflaging the skin abnormality by one or more of the above three techniques, the last step is the application of a translucent setting or fixing powder and fixing spray, when needed. This sets, waterproofs and prevents smudging of the camouflage. Fixing sprays make the camouflage more water-resistant and smudge proof. These are advised when using camouflage in warm humid conditions and while going for swimming.
Finally, removing the camouflage makeup should be taught to the patient, as it may be more difficult than removing regular makeup products. Water-soluble cream type makeup remover is best suited for this purpose. It is applied generously to emulsify the makeup, which is then removed by wiping with cotton pads. Alcohol or acetone-based removers should be avoided as they can cause excessive drying and irritation to sensitive skin. The last step is to wash the face with gentle soap and pat dry, followed by skin moisturisation. In the author’s experience, just washing thoroughly with gentle soap is sufficient for most cream-based formulations. Newer liquid formulations like Microskin are very water-resistant and may not be washed off, requiring specially formulated removers provided by the manufacturer. However, daily removal for such liquid formulations is not advocated by their manufacturers, as it is an advantage for the patient to not have to reapply them every day.
Adverse effects
Potential adverse effects of camouflage products include cutaneous reactions in the form of allergic contact dermatitis, irritation and photoallergic or phototoxic reactions. Allergic reactions due to cosmetics are usually attributed to fragrances, p-phenylenediamine, lanolin and its derivatives, glyceryl monothioglicolate, propylene glycol or preservatives such as formaldehyde, imidazolidinyl urea, Quaternium-15 and parabens.13-15 The possibility of these adverse effects can be minimised by using standardised products formulated with non/hypoallergenic components.
Benefits of camouflage
Though most skin disorders and disfigurements are downplayed as not being associated with direct physical impairment or mortality, the psychosocial and emotional impact on patients may be significant enough to affect work, inter-personal/social relationships and leisure activities, resulting in depression, anxiety and even suicidal ideation.16 Female patients tend to experience greater social distress than their male counterparts. The intensity of the impact of skin disease may also depend on associated social stigmas as has been seen in cases of vitiligo and leprosy.17-19
The most important benefit of skin camouflage is the immediate result. This instancy may help even in some of the treatable dermatoses till the effect of medical therapy takes over. Camouflage, by giving freedom from the onslaught of prying eyes and questions, makes daily life and socializing a lot easier, thus leading to a more positive outlook in users. Similar feelings have been echoed by a patient after using camouflage, in a first-hand account.20 The emotional benefits of camouflage have been well documented in the literature, with reported improvement in quality of life indices.21-35 A multi-centre study, assessing the effect of camouflage in disorders of pigmentation, scarring and vascular lesions, showed a significant improvement in Dermatology Life Quality Index scores after one month of cosmetic camouflage use.21 Its role in patients with vitiligo has been studied and found to be of significant benefit.22,23 Its benefits in leprosy were found to exceed those for vitiligo in a recent study.24 A systematic review indicated significant improvement in quality of life after the use of cosmetic camouflage in patients with disfiguring skin diseases, with mean reductions in Dermatology Life Quality Index scores ranging from 1.4 to 6 in various disorders, signifying improvements in psychosocial parameters.29
Limitations of camouflage
Skin camouflage is most effective when applied over skin with abnormal colour without any textural changes; raised or depressed lesions are not disguised completely. Special techniques in the application procedure, as described earlier, are needed to make the latter less conspicuous. Similarly, rough scars are more difficult to conceal than smooth ones because sometimes after the application of camouflage creams, the irregularity is exaggerated. A relative limitation is that with very large surface areas camouflage may be difficult, cumbersome and costly.36
Another limitation of these products is smudging. Camouflage creams are formulated in such a way that when properly applied they achieve a fairly good waterproof effect, remaining effective up to 8 hours. But these creams do tend to rub off in areas of constant friction such as the hands, feet, cuffs and neckline. Tanioka et al. described a camouflage technique using the Cavilon™ 3M No Sting Barrier Film (3M, St. Paul, MN) as a spray, which contains a siliconized material.37 It is commonly prescribed to provide a long-lasting waterproof barrier for damaged skin in patients with stoma sites or sore skin caused by incontinence of urine or feces. When applied over skin camouflage, it was found to help in both increasing the waterproof effect and preventing rubbing off. Certain camouflage product providers like DermacolorR also market camouflage fixing sprays containing film-forming agents like acrylates/t-butylacrylamide copolymer to decrease smudging. Additionally, liquid formulations marketed nowadays are much more water- and smudge-resistant, even without the use of fixing sprays.
Considering these limitations, it is important to set realistic expectations while recommending skin camouflage.
Hurdles in skin camouflage
Despite its benefits, the use of skin camouflage therapy among dermatologists in clinical practice remains low.38 There are multiple hurdles against its more extensive use. Foremost is the lack of acceptance of camouflage by both dermatologists and patients. From the dermatologist’s perspective, their role seems to end where the role of camouflage begins. On the other side, the patient comes to the dermatologist hoping for a cure rather than a palliative measure. Further, there are many practical problems in its utilisation. The cost of good-quality camouflage products is one limiting factor, especially when use over a larger area is needed. The availability of these products is also a major concern as there are only a few medical camouflage brands available, at limited departmental stores or mass merchandisers [Table 2]. Online access to these products, which is an alternative, may not be feasible for all patients. Moreover, access to education for patients, which is the most important step for successful adoption is lacking. Steps to integrate skin camouflage therapy with dermatology residency training, along with setting up dedicated skin camouflage clinics at least in all teaching dermatology departments may help in alleviating these problems. More widespread use will create demand and that should lead to better supply chains and decreased costs.
Recent and future trends
Lately, the concept of camouflage clinics and therapists has been gaining traction in some countries. Camouflage therapists educate the patients thoroughly in camouflage techniques and assist them in coping constructively with the psychological trauma of their skin condition.3,39 Camouflage clinics may be attached to dermatology or cosmetology clinics and are of great help in settings with high patient loads and paucity of time to counsel and educate the patients regarding camouflage therapy. In the USA, camouflage therapists are state-licensed and trained skincare professionals, while in others, no such license is needed to run a camouflage clinic, and a trained nurse is well qualified for this purpose.36
As regards products, with the advent of nanotechnology, there is a possibility of finer camouflage products being manufactured that can be applied as a thin layer and yet give the desired results.40
Conclusion
Skin camouflage is not a cure, but it provides an immediate natural skin appearance and has immense emotional benefits. All patients eligible for camouflage therapy should be made aware of the availability of this option as an adjunctive therapy, preferably with a practical demonstration. Efforts should be made to set up skin camouflage clinics in dermatology departments to meet the needs of patients with skin imperfections as well as to help in teaching camouflage techniques to budding dermatologists.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Dictionary.com [Internet]. Available from: http://dictionary.reference.com/browse/camouflage [Last cited on 2011 Aug 15]
- Camouflage and makeup preparations. Clin Dermatol. 2001;19:406-12.
- [CrossRef] [PubMed] [Google Scholar]
- History of skin camouflage. The British association of Skin Camouflage. Skin-camouflage.net[Internet] [Last accessed on 2022 Mar 29]. Available from:
- [Google Scholar]
- Camouflage Techniques In: Draelos ZD, ed. Cosmetic Dermatology: Products and Procedures (2nd ed.). Oxford, UK: John Wiley & Sons, Ltd; 2015. p. :186-92. In: eds.
- [Google Scholar]
- Medical makeup for concealing facial scars. Facial Plast Surg. 2012;28:536-40.
- [CrossRef] [PubMed] [Google Scholar]
- Make-up as an adjunct and aid to the practice of dermatology. Dermatol Clin. 1991;9:81-8.
- [PubMed] [Google Scholar]
- Prospective study of cosmetic reactions: 1977-1980. J Am Acad Dermatol. 1982;6:909-17.
- [CrossRef] [PubMed] [Google Scholar]
- A five-year study of cosmetic reactions. J Am Acad Dermatol. 1985;13:1062-9.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic contact dermatitis to preservatives and fragrances in cosmetics. Skin Ther Lett. 2011;16:1-4.
- [PubMed] [Google Scholar]
- The potential psychological impact of skin conditions. Dermatol Ther. 2017;7:53-7.
- [CrossRef] [PubMed] [Google Scholar]
- Stigma experience in skin disorders: An Indian perspective. Dermatol Clin. 2005;23:635-42.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life in patients with vitiligo. Health Qual Life Outcomes. 2003;1:58.
- [CrossRef] [PubMed] [Google Scholar]
- A patient’s journey: Facial disfigurement. BMJ. 2011;343:d5203.
- [CrossRef] [PubMed] [Google Scholar]
- Decorative cosmetics improve the quality of life in patients with disfiguring skin diseases. Eur J Dermatol. 2002;12:577-80.
- [PubMed] [Google Scholar]
- Quality of life and stigmatization profile in a cohort of vitiligo patients and effect of the use of camouflage. Dermatology. 2005;210:279-85.
- [CrossRef] [PubMed] [Google Scholar]
- Camouflage for patients with vitiligo vulgaris improved their quality of life. J Cosmet Dermatol. 2010;9:72-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cosmetic camouflage of visible skin lesions enhances life quality indices in leprosy as in vitiligo patients: An effective stigma reduction strategy. Lepr Rev. 2020;91:343-52.
- [CrossRef] [Google Scholar]
- Cosmetic camouflage advice improves quality of life. Br J Dermatol. 2002;147:946-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of skin care and makeup under instructions from dermatologists on the quality of life of female patients with acne vulgaris. J Dermatol. 2006;33:745-52.
- [CrossRef] [PubMed] [Google Scholar]
- Make-up improves the quality of life of acne patients without aggravating acne eruptions during treatments. Eur J Dermatol. 2005;15:284-7.
- [PubMed] [Google Scholar]
- Cosmetic camouflage improves quality of life among patients with skin disfigurement: A systematic review. Body Image. 2018;27:98-108.
- [CrossRef] [PubMed] [Google Scholar]
- Corrective cosmetics are effective for women with facial pigmentary disorders. Cutis. 2005;75:181-7.
- [PubMed] [Google Scholar]
- Psychological and psychosocial functioning of children with burn scarring using cosmetic camouflage: A multi-centre prospective randomised controlled trial. Burns. 2014;40:135-49.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of cosmetic camouflage on the quality of life of children with skin disease and their families. J Cutan Med Surg. 2016;20:211-5.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of quality of life after a medical corrective make-up lesson in patients with various dermatoses. Dermatology. 2012;224:374-80.
- [CrossRef] [PubMed] [Google Scholar]
- Emotional benefit of cosmetic camouflage in the treatment of facial skin conditions: Personal experience and review. Clin CosmetInvestig Dermatol. 2012;5:173-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Waterproof camouflage age for vitiligo of the face using Cavilon 3M as a spray. Eur J Dermatol. 2008;18:93-4.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, attitude, and practice of cosmetic camouflage among dermatology residents. Pigment International. 2021;8:166-72.
- [CrossRef] [Google Scholar]
- Camouflage for patients with vitiligo. Indian J Dermatol Venereol Leprol. 2012;78:8.
- [CrossRef] [PubMed] [Google Scholar]
- Nanotechnology: A new paradigm in cosmeceuticals. Recent Pat Drug Deliv Formul. 2007;1:171-82.
- [CrossRef] [PubMed] [Google Scholar]






