Translate this page into:
Skin coloured asymptomatic facial plaque in a woman
Corresponding author: Dr. Ruby Jain, Department of Dermatology, Skin Care Clinic, Dimapur, Nagaland, India. rubyjain75@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Jain R, Dhar S. Skin coloured asymptomatic facial plaque in a woman. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1088_2023
A 32-year-old woman presented with an asymptomatic slow-growing, skin-coloured elongated plaque that appeared finger-like on the right pre-auricular area [Figure 1] of 4-years duration. It started as a small lesion from the level of the earlobe ascending upwards and reached the tragus of the right ear. She was intermittently applying Betamethasone-neomycin combination cream on the whole face for hyperpigmentation for a few months.

- Single, well-defined, flat, translucent plaque looking like a finger on the right pre-auricular area.
On cutaneous examination, a single, soft, fleshy, well-defined, translucent, skin-coloured, elongated, finger-like, linear lesion measuring 3.5 × 1.5 cm was seen on the right pre-auricular area. The lesion showed two irregular depressions due to ulceration in the central part of the lesions near both ends. The ulceration occurred after the application of some herbal paste on the lesion. Prominent fine telangiectasias and skin thinning with dryness of the face were also observed. She had no other cutaneous findings, and systemic examination was unremarkable.
Routine haematological and biochemical investigations, hormonal assays, chest X-ray and echocardiogram were normal. Viral markers including hepatitis serology and HIV serology were negative. The lesion was completely excised, and the tissue was sent for histopathological examination.
Histopathology showed unremarkable stretched-out epidermis [Figure 2a]. The upper dermis showed the proliferation of variably sized blood vessels, almost uniformly distributed throughout the tumour and scattered fibroblasts lying in a loose myxoid stroma [Figures 2b and 2c].
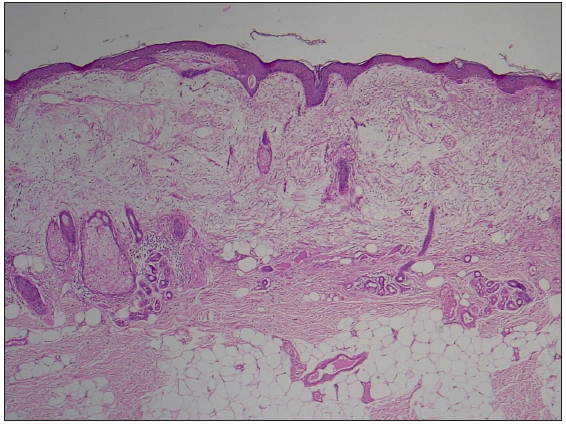
- Unremarkable epidermis and a loose myxomatous tumour in the dermis (Haematoxylin and eosin, 40x).
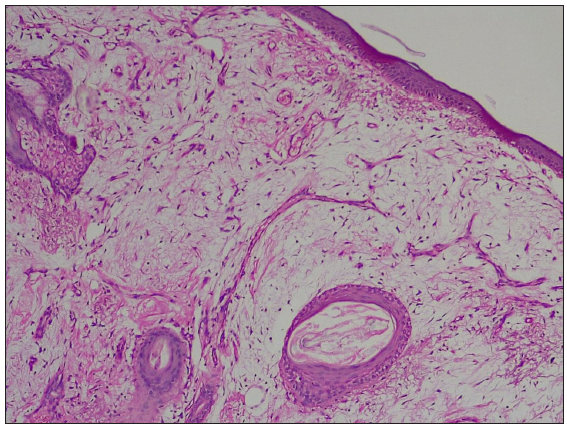
- Lobulated myxoid mass with thin-walled blood vessels (Haematoxylin and eosin, 100x).
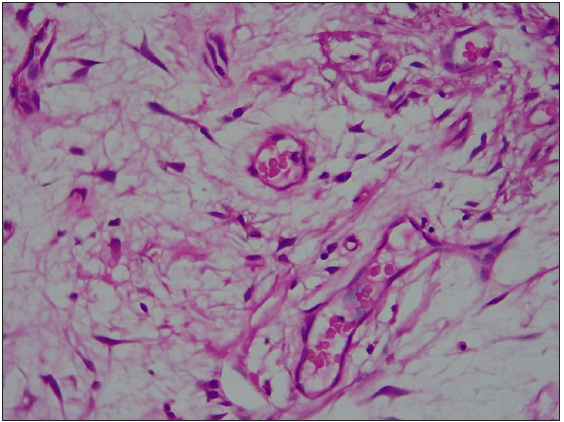
- Stellate fibroblasts surrounded by pools of mucin and dilated blood vessels (Haematoxylin and eosin, 400x).
No nuclear atypia or malignancy was seen. Combined Alcian blue and Periodic Acid Schiff stain (PAS) stain shows abundant mucin in the stroma [Figure 2d].
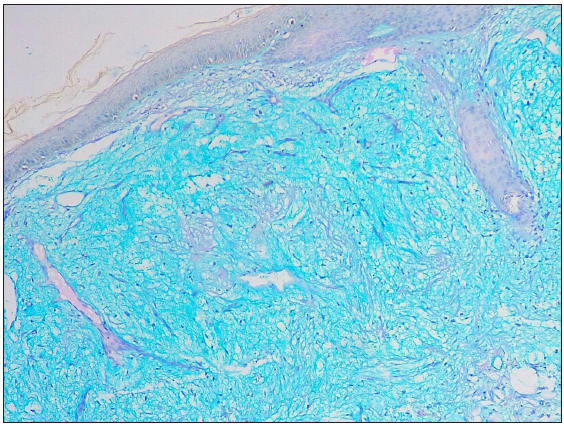
- Alcian blue and PAS stain 100x highlights mucin in the dermis.
Question
What is your diagnosis?
Answer
Diagnosis: Superficial angiomyxoma (SAM)
Discussion
SAM of skin, also referred to as cutaneous myxoma, is a rare benign soft tissue tumour which is poorly recognised.1 It is distinguished histologically by the presence of a prominent myxoid stroma and numerous blood vessels. SAM was first described by Carney et al. in 1985.2 It usually occurs as a solitary lesion, but multiple lesions occur when it is associated with the Carney complex.2 Carney complex is a multi-system autosomal dominant disorder due to mutations in the PRKAR1A gene located on chromosome17q22-24.3 The PRKAR1A is a tumour suppressor gene that encodes for the protein kinase A regulatory 1-alpha subunit. Carney complex includes myxomas, spotty pigmentation, endocrine overactivity and schwannomas.
SAM is one of the five mainstream soft tissue myxomas described in the literature.4 It affects all age groups, mainly between the third and fourth decades. It affects men more than women, with an incidence of 0.008–3%.3,4 Most cases present as papules, nodules or polypoid lesions. They occur more commonly in the head and neck regions but may arise in the trunk and lower limb.5 They usually measure less than 5 cm in diameter. In our case, the lesion was an elongated finger-like plaque on the right pre-auricular area, similar lesion was described by Nakayama et al in right inguinal region.6 It measured less than 5 cm. Epithelial components are present in 25% of tumours2,4 and they indicate the possibility of recurrence.
The definitive diagnosis of SAM is based on histology, and immunohistochemistry helps to differentiate it from other myxoid tumours. Typically, the tumour is positive for vimentin and CD34 and negative for desmin, smooth muscle actin, S100 and pan-cytokeratin. Histopathologically, the tumour is localised in the reticular dermis, but the involvement of the subcutis may occur in a few cases. These cases show the proliferation of the spindle to stellate-shaped cells in the prominent myxoid stroma with a thin arborising vascular network and mixed inflammatory cell infiltrate. Nuclear atypia and mitotic activity are generally absent.
Local recurrence was commonly seen in 3.6–38.1%4,5 of cases after incomplete excision, though distant metastases were not reported. Our patient was in complete remission after a year of follow-up.
The common differential diagnosis of SAM includes cutaneous mucinoses, dermal nerve sheath myxoma, trichodiscoma, trichofolliculoma and low-grade fibrosarcoma/fibromyxoid sarcoma. Cutaneous mucinosis appears as raised spots, often on the neck, face and scalp and histologically contains clefts and mucin pools, but very few vessels. SAM is generally larger than cutaneous focal mucinoses and cutaneous myxoid cysts and is not infiltrative but well circumscribed.5 Dermal nerve sheath tumours are rare benign peripheral nerve sheath tumours arising from the skin and subcutaneous tissues, especially on limbs with characteristic bland spindle cells and epitheloid Schwann cells, as seen histologically. SAM may need to be differentiated from trichodiscomas and fibro folliculomas5, which are hamartomatous tumours arising from pilosebaceous units and usually present as small facial papules. Furthermore, it should be differentiated histologically from the myxoid/mucin or spindle cell predominant variant of trichodiscomas, which can better be differentiated by immunohistochemical staining. Low-grade fibromyxoid sarcomas and low-grade myxofibrosarcoma have distinct clinical and histopathological features to distinguish them from SAM.
Early diagnosis and wide surgical excision are the treatments of choice to prevent recurrence. Our diagnosis of SAM was based on the clinico-histopathological features, that are in corroboration with observations made by Calonje E et al.1
We report this case because of the rare presentation of SAM as a finger-like elongated plaque lesion on the face, which is generally not reported in the literature.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Superficial angiomyxoma: Clinicopathologic analysis of a series of distinctive but poorly recognized cutaneous tumors with tendency for recurrence. Am J Surg Pathol. 1999;23:910-7.
- [CrossRef] [PubMed] [Google Scholar]
- The complex of myxomas, spotty pigmentation, and endocrine overactivity. Medicine.1985. ;64:270-83.
- [CrossRef] [Google Scholar]
- Novel PRKAR1A gene mutations in Carney complex. Int J Clin Exp Pathol. 2010;3:545-8.
- [PubMed] [PubMed Central] [Google Scholar]
- Myoxoma is not a single entity. A review of the concept of myxoma. Ann Diagn Pathol. 2000;4:99-123.
- [CrossRef] [PubMed] [Google Scholar]
- Morphological diversity of trichodiscomas and fibrofolliculomas. Am J Dermatopathol. 2014;36:734-40.
- [CrossRef] [PubMed] [Google Scholar]
- Superficial angiomyxoma of the right inguinal region: Report of a case. Jpn J Clin Oncol. 1997;27:200-3.
- [CrossRef] [PubMed] [Google Scholar]





