Translate this page into:
Skull vault erosion and cerebral venous sinus thrombosis as a manifestation of actinomycosis: An uncommon presentation
Corresponding author: Dr. Swastika Suvirya, Department of Dermatology, Venereology and Leprosy, King George’s Medical University, Lucknow, India. swastika.p@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Priyadarshi D, Karunanithi E, Batrani M, Verma P, Suvirya S. Skull vault erosion and cerebral venous sinus thrombosis as a manifestation of actinomycosis: An uncommon presentation. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1054_2024
Dear Editor,
A 41-year-old man presented to the dermatology outpatient with multiple discharging swellings on the left side of his face and scalp for six months. He also complained of mild intermittent headache in the last two months. There was no associated fever, weight loss, or mental obtundation. A year ago, the patient had suffered craniofacial trauma in a road traffic accident, leading to scalp lacerations that required 14 stitches, though his computed tomography (CT) head study was normal. A month later, during a fight, his head was banged against a wall leading to the reopening of the wound. This led to a secondary infection requiring repeated debridement and resuturing. Four months after this incident, he began to develop unilateral pustular lesions on the face and scalp, which worsened progressively. He was prescribed multiple short courses of antibiotics, without relief.
Physical examination revealed a large plaque approximately 20×15 cms, on the left side of his face and scalp studded with papules, cysts, and nodules. Multiple discharging sinuses draining minimal serosanguinous fluid was present over the lesion [Figure 1]. Suture marks were seen on the scalp vault around 10 cm in length on the left parieto-occipital region. Mucosal and systemic examinations were non-contributory.

- Nodules, cysts, and sinuses on the left side of the face and scalp.
We considered differential diagnoses of tuberculosis, eumycetoma, nocardiosis, and actinomycosis. Gram staining from the discharge showed few gram-positive cocci while acid-fast bacilli (AFB) smear, cartridge-based nucleic acid amplification test (CBNAAT), and potassium hydroxide (KOH) mount from pus were negative. Culture from skin tissue for aerobic/anaerobic bacteria, mycobacteria, and fungus were negative. Contrast-enhanced magnetic resonance imaging (CEMRI) with 3D (three-dimensional) MRV (magnetic resonance venography) of the brain showed enhanced soft tissue scalp thickening over the left temporo-occipital region with focal areas of erosion of the underlying calvaria, enhanced dural thickening suggestive of pachymeningitis [Figure 2a] and associated thrombosis of the left transverse and sigmoid sinuses, which were reconstituted by collaterals [Figure 2b].
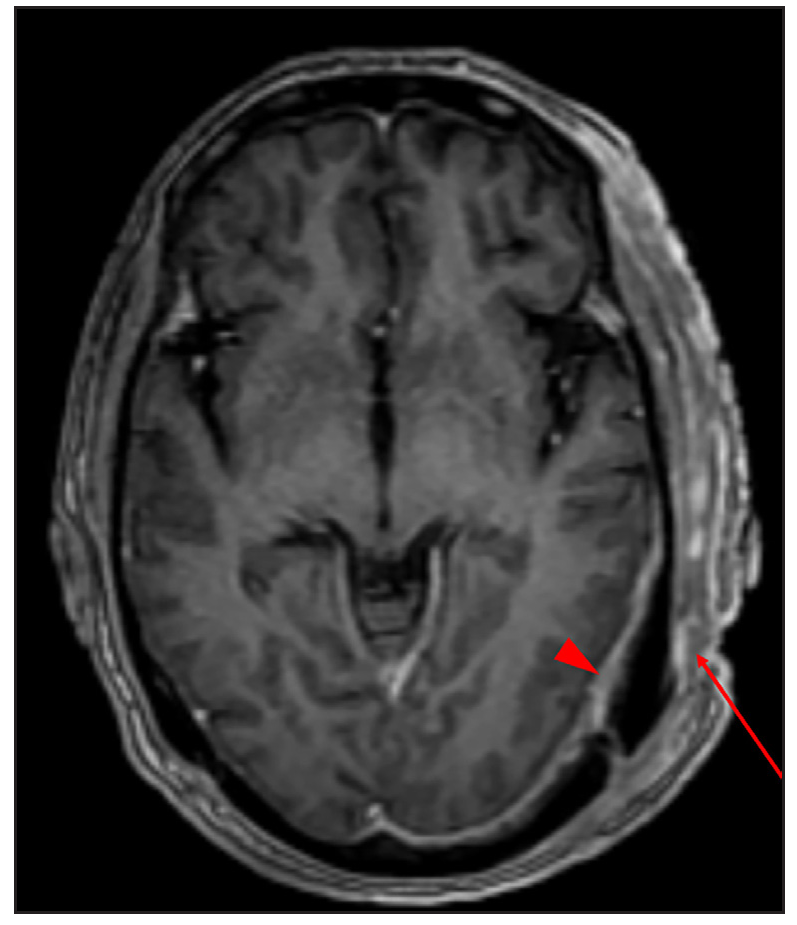
- Axial T1W CEMRI showing a heterogeneously enhancing soft tissue thickening involving the scalp over the left temporo-occipital region (red arrow), with focal areas of erosion of the underlying calvaria enhancing dural thickening suggestive of pachymeningitis (red arrowhead).
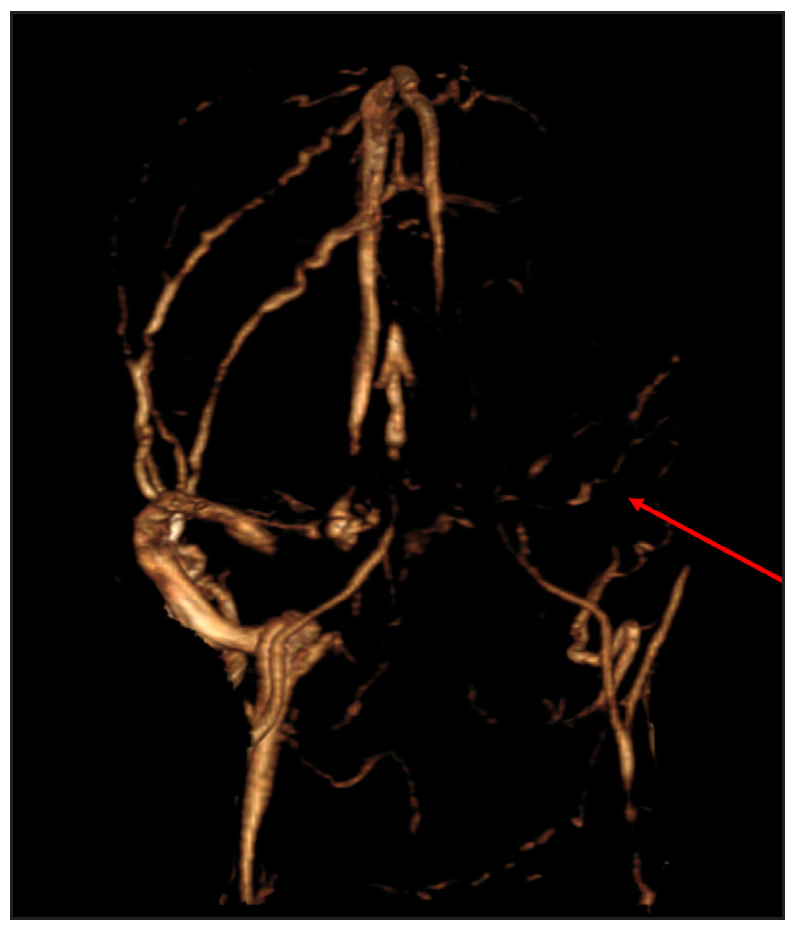
- 3D reconstructed Magnetic Resonance (MR) venogram showing involvement of the left transverse and sigmoid sinuses which are reconstituted by collaterals (red arrow).
Histopathological examination from the nodule revealed a neutrophilic abscess cavity containing two granules surrounded by haemorrhagic granulation tissue and inflammatory cells, including neutrophils, lymphocytes, plasma cells, and macrophages occupying the upper half of the dermis while the lower half of dermis was replaced by dense fibrosis. The granules were composed of thin basophilic filaments with a radiating eosinophilic fringe in a larger granule [Figure 3a]. Periodic acid-Schiff (PAS) and Grocott methenamine silver (GMS) positively stained the granules [Figure 3b]. Filaments comprising the grain were non-acid-fast on Fite stain. A final diagnosis based on clinical, radiological, and histopathological findings was suggestive of skull vault actinomycosis with unilateral transverse and sigmoid sinus thrombosis.
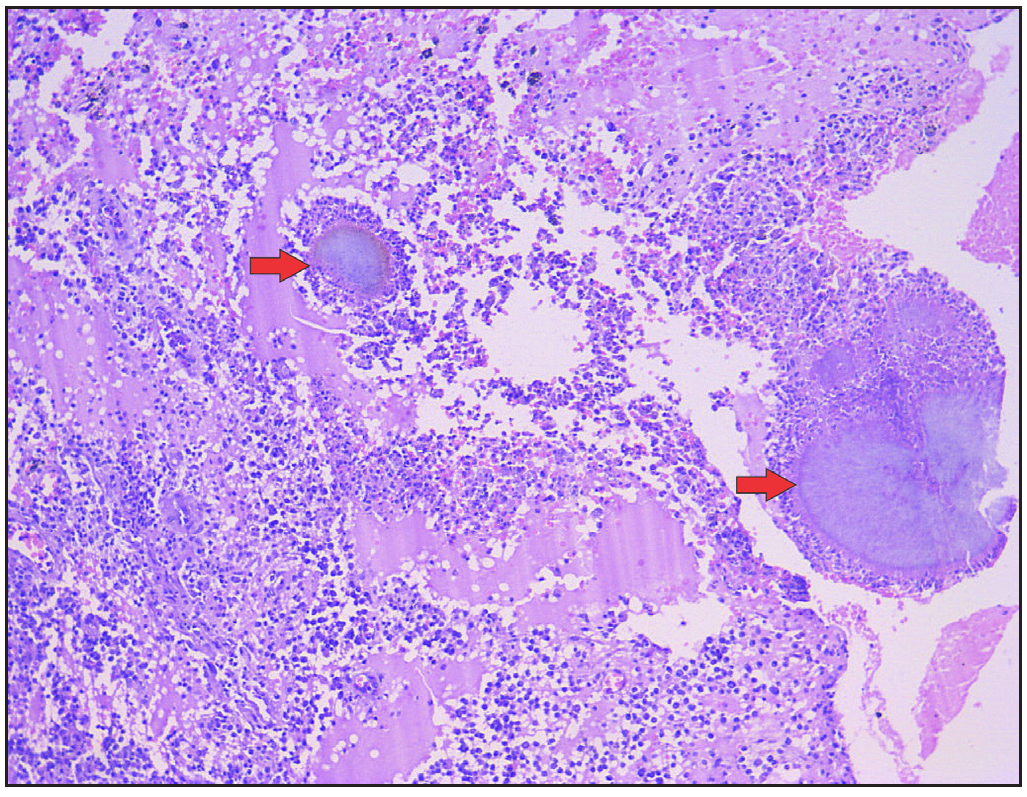
- Abscess cavity containing two grains (red arrows) surrounded by neutrophils (Haematoxylin and eosin, 100x).
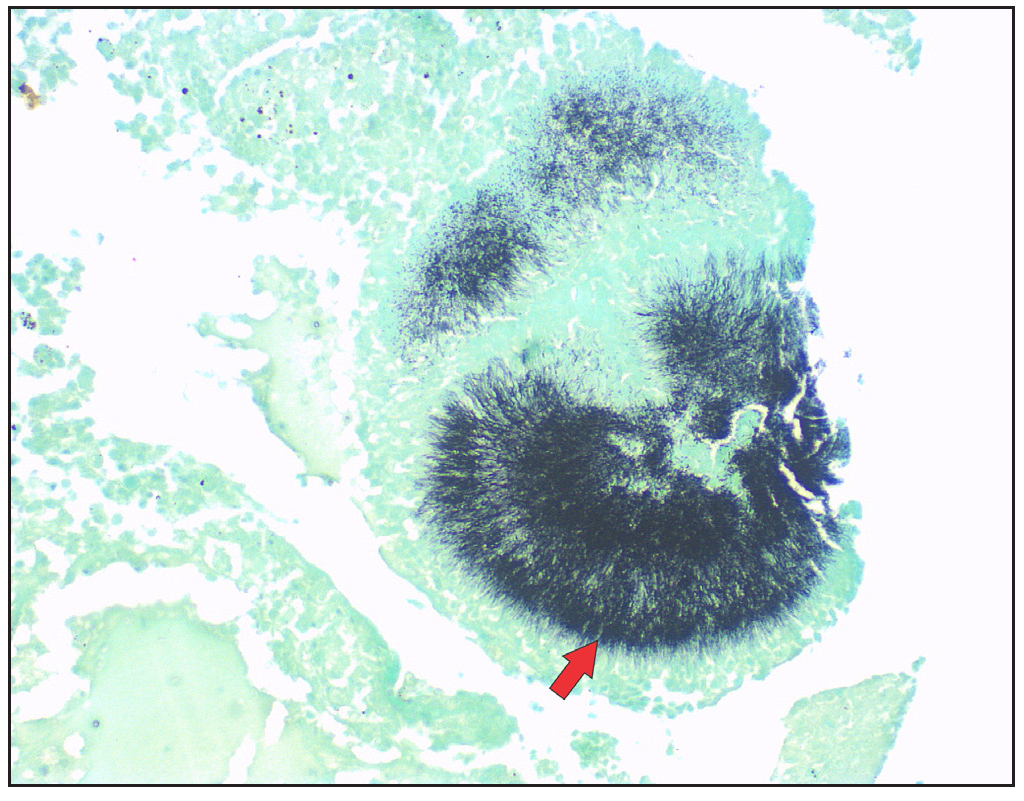
- Thin filamentous Grocott Methenamine Silver (GMS) positive hyphae comprising the grain (red arrow) (GMS, 200x).
In consultation with the neurologist, patient was treated with oral doxycycline 100 mg and clarithromycin 500 mg, twice a day, with regular monitoring for signs of any increased intracranial pressure. No additional treatment for cerebral venous sinus thrombosis was suggested as imaging revealed the formation of collaterals, and there were no signs of increased intracranial pressure. At 6-months, profound improvement with the healing of cutaneous lesions and remission of headache was observed without any therapy-related adverse effects [Figure 4]. We plan to continue a single antimicrobial, doxycycline, as clarithromycin becomes ineffective in actinomycosis after six months and also because skin lesions exhibited a good treatment response. A radiological re-evaluation is scheduled at 12 months.

- Healing of cutaneous lesions post six months of treatment.
Actinomycosis is an indolent infection caused by anaerobic or microaerophilic bacteria, primarily of the genus Actinomyces, presenting as abscesses and sinus discharging sulphur granules and serosanguinous fluid. It commonly affects the cervicofacial regions, needing mucosal disruption to invade.1 Diagnosis is often based on clinical suspicion, gram staining findings from tissue or aspirated pus, and histopathology, as skin cultures can be negative in 50% of the cases.2 Treatment includes prolonged (6–12 months) antimicrobial agents including penicillin G, amoxycillin, and less often ceftriaxone, doxycycline, macrolides, and carbapenems. Surgery may be required sometimes for abscess drainage, sinus tract marsupialisation, and necrotic tissue debridement for diagnostic and therapeutic purposes.
Skull vault actinomycosis manifests as calvarial osteomyelitis or epidural/subgaleal abscess. This contrasts with the relatively more common central nervous system (CNS) actinomycosis, which generally involves the brain parenchyma, presenting as brain abscess.3 In this case, there was a clinico-radiological association, in the sense that despite such florid involvement on radiology, the patient had minimal neurological symptoms. Also, in this case, unusually, the occipital region was mainly involved, unlike the more typical frontotemporal region. To the best of our knowledge, we could not find any case of skull vault actinomycosis with simultaneous involvement of sigmoid and transverse sinus.3,4 The cerebral sinuses could have been affected either via emissary veins or through direct contiguous infiltration into the sinuses. Despite extensive disease, the patient was successfully managed medically with the right choice of antimicrobials, eliminating the need for surgical intervention.
This case stresses the need for a high degree of suspicion for skull vault/CNS dissemination of actinomycosis even with minimal neurological symptoms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Actinomycosis: Etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014;7:183-97.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A case series of actinomycosis from a single tertiary care center in Saudi Arabia. IDCases. 2019;15:e00521.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Recurrent skull vault actinomycosis: A case report and review of literature. IDCases. 2021;25:e01215.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A Rare case of central nervous system actinomycosis presenting with moyamoya syndrome. CNS Neurosci Ther. 2022;28:1139-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





