Translate this page into:
Solitary asymptomatic nodule on the leg
2 Department of Pathology, San Cecilio University Hospital, Granada, Spain
Correspondence Address:
Ana Almodovar-Real
Department of Dermatology, San Cecilio University Hospital, Avenida Doctor Olóriz 16, 18012 Granada
Spain
| How to cite this article: Almodovar-Real A, Aneiros-Fernandez J, Diaz-Martinez MA, Naranjo-Sintes R. Solitary asymptomatic nodule on the leg. Indian J Dermatol Venereol Leprol 2016;82:109-111 |
A 58-year-old man presented with an asymptomatic skin nodule on the left leg for several months. Physical examination showed a well-defined, erythematous nodule (2 cm × 1.5 cm) with a lobulated surface [Figure - 1]. Differential diagnoses of squamous cell carcinoma, basal cell carcinoma and cutaneous lymphoma were considered. An excisional biopsy was performed. Histopathology showed pseudoepitheliomatous hyperplasia [Figure - 2]. There was a dense, irregular, lymphoid infiltrate with admixture of neutrophils, eosinophils and large, atypical Reed-Sternberg-like cells in the dermis [Figure - 3]. Immunohistochemical analysis revealed strong positivity for CD30 [Figure - 4]a. Tumor cells were also positive for the cytotoxic marker T-cell intracellular antigen-1 [Figure - 4]b, CD3, CD7 and CD4 [Figure - 4]c. On the other hand, AE1-AE3, CD8, CD56, CD20, ALK-1, CD5, CD15 and CD25 were all negative. Routine investigations and positron emission tomography-computed tomography study were normal. There was no recurrence after 1 year of follow-up.
 |
| Figure 1: Asymptomatic nodule on leg |
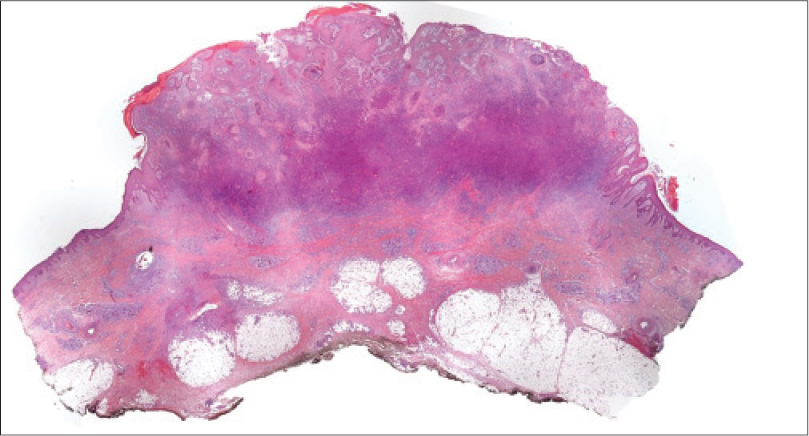 |
| Figure 2: Pseudoepitheliomatous epidermal hyperplasia (H and E, ×10) |
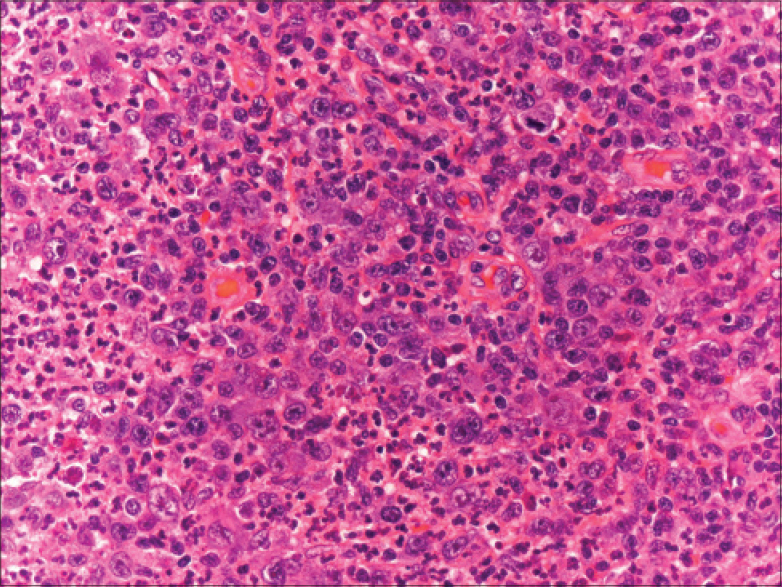 |
| Figure 3: Dense infiltrates of atypical lymphocytes in dermis; large and atypical Reed–Sternberg-like cells (H and E, ×200) |
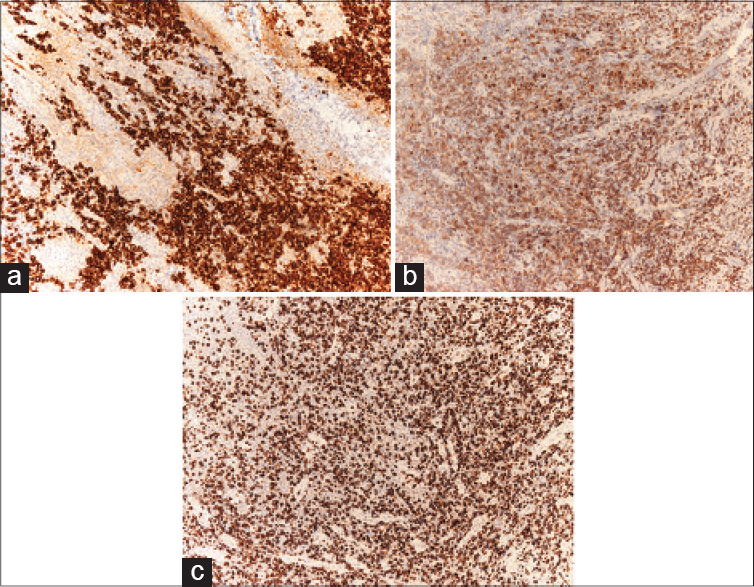 |
| Figures 4: Neoplastic cells positive for (a) CD30 (×100), (b) cytotoxic marker T-cell intracellular antigen-1 (×100) and (c) CD4 (×100) |
What Is Your Diagnosis?
| 1. |
Szpor J, Dyduch G, Galazka K, Bahyrycz J, Stój A, Tomaszewska R. Primary cutaneous CD30+lymphoproliferative disorder – A 10-year follow-up. A case report and differential diagnosis. Pol J Pathol 2009;60:43-8.
[Google Scholar]
|
| 2. |
Ralfkiaer E, Willemze R, Paulli M, Kadin ME. Primary cutaneous CD30-positive T-cell lymphoproliferative disorders. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al., editors. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th ed. Lyon: IARC; 2008. p. 300-1.
[Google Scholar]
|
| 3. |
Quintanilla-Martinez L, Jansen PM, Kinney MC, Swerdlow SH, Willemze R. Non-mycosis fungoides cutaneous T-cell lymphomas: Report of the 2011 Society for Hematopathology/European Association for Haematopathology workshop. Am J Clin Pathol 2013;139:491-514.
[Google Scholar]
|
| 4. |
Querfeld C, Kuzel TM, Guitart J, Rosen ST. Primary cutaneous CD30+ lymphoproliferative disorders: New insights into biology and therapy. Oncology (Williston Park) 2007;21:689-96.
[Google Scholar]
|
| 5. |
Kadin ME. Primary cutaneous CD30-positive T-cell lymphoproliferative disorders. In: Jaffe ES, editor. Hematopathology: Expert Consult. 1st ed. Philadelphia, PA: Saunders/Elsevier; 2011. p. 604-16.
[Google Scholar]
|
Fulltext Views
2,628
PDF downloads
2,846






