Translate this page into:
Solitary asymptomatic papule on cheek
2 Medical College and Hospital, West Bengal, India
3 Consultant Dermatologist, Cutaneous Lymphoma and Cutaneous Oncology, Tata Medical Centre, Kolkata, India
4 Consultant Pathologist, Tata Medical Centre, Kolkata, India
Correspondence Address:
Piyush Kumar
Dermatology, Katihar Medical College and Hospital, Katihar - 854 105, Bihar
India
| How to cite this article: Kumar P, Parveen A, Das A, Raychaudhury T, Arun I. Solitary asymptomatic papule on cheek . Indian J Dermatol Venereol Leprol 2014;80:481-482 |
A 25-year-old girl presented to us with solitary asymptomatic papule over the left cheek for the last 6 years. At the outset, it was a pin-head sized elevation but gradually increased to a size of around 1 cm after which it had been static for the last 2 years. Physical examination revealed a single flesh-colored, firm to rubbery papule over the left cheek [Figure - 1]a and b. The remainder of the muco-cutaneous examination including hair, nails, and mucosae was non-contributory. Routine investigations including serum biochemistry panel, urine examination, chest X-ray and ultrasonography of the abdomen were non-contributory. An excision biopsy of the lesion revealed a nodular lesion in the dermis, composed of tightly woven fascicles of slender spindle cells with bland nuclei [Figure - 2]a-c. Immunohistochemical staining showed the neoplastic cells to be positive for S-100 protein [Figure - 3]a and negative for glial fibrillary acid protein (GFAP) [Figure - 3]b.
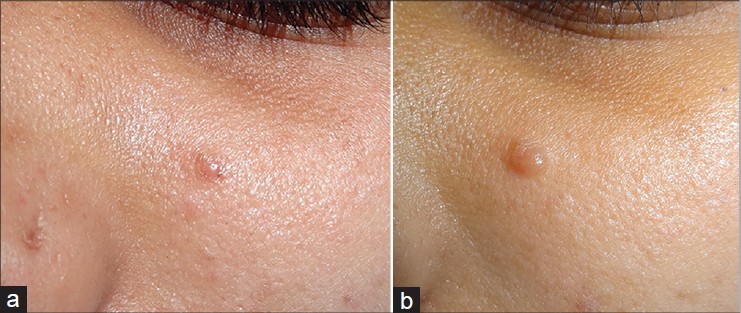 |
| Figure 1: (a) Solitary flesh-colored papule on left cheek. (b) Close up of the lesion |
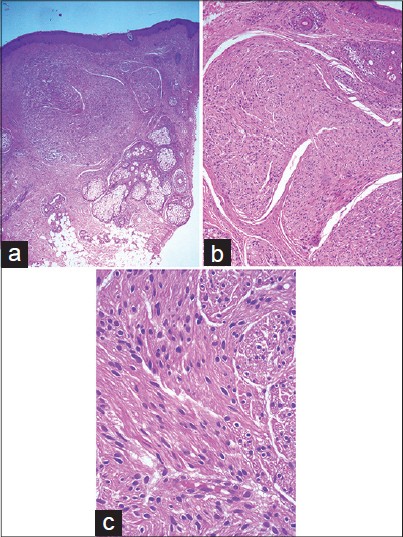 |
| Figure 2: (a) There is a nodular lesion in the dermis composed of fascicles of spindled Schwann cells with bland nuclei (H and E, ×40). (b) Fascicles of spindled Schwann cells in the dermis showing vague palisading, narrow gaps separating fascicles, and clefting from the adjacent dermis (H and E, ×100). (c) No mitotic activity or nuclear atypia is seen in the neoplastic cells (H and E, ×400) |
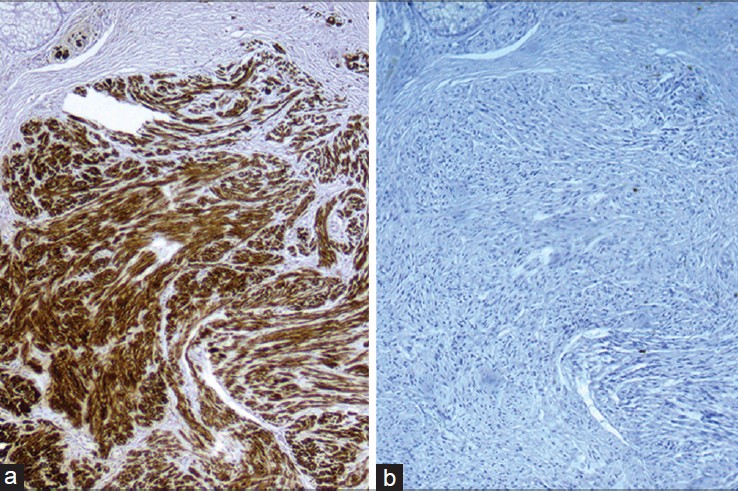 |
| Figure 3: (a) Neoplastic cells are diffusely positive for S100 (H and E, ×400). (b) An immunostain for GFAP is negative in the neoplastic cells (×400) |
What is your diagnosis?
Diagnosis
Palisaded encapsulated neuroma (also known as solitary circumscribed neuroma).
DISCUSSION
Palisaded encapsulated neuroma (PEN), first described by Reed et al., in 1972, is classified as a primary hyperplasia of nerve fibers (axons and their sheath cells). [1] It typically presents with a solitary, sessile, immobile, asymptomatic skin-colored papule or nodule, commonly affecting the "butterfly area" of the face of a middle-aged person. Atypical sites of involvement include the trunk, oral mucosa, shoulder and eyelids. It does not have any sex predilection. Clinically, it may be confused with neurofibroma, melanocytic nevus, appendageal tumors and basal cell carcinoma. The firmness of the lesion and absence of button-hole sign are important clinical findings that distinguish it from neurofibroma. [2] The nodular presentation is most common, but fungating, plexiform, multinodular, epithelioid, vascular and myxoid variants have been reported. [3] Atypical presentations include multiple lesions on palms and soles, [4] and dermatomal distribution on the face. [5]
The histological appearance lies between neurofibroma and schwannoma. [2] It shows a well-circumscribed, ovoid, or rounded nodule in the dermis, which is actually a bulbous expansion of the peripheral nerve. Within the nerve, there is collection of axons and Schwann cells in interlacing fascicles along with characteristic cleft-like spaces. Nuclear pleomorphism and mitoses are absent. Electron microscopy demonstrates a substantial number of class C fibers (mostly non-myelinated), partially enveloped by Schwann cell cytoplasm. [2],[3]
The histological differential diagnoses include neurofibroma (which is non-capsulated, and shows presence of mucopolysaccharide ground substance); schwannoma (which shows Antoni A and B bodies); traumatic neuroma (which has abundant Schwann cells, axons, inflammatory cells and scarring) and leiomyoma (which has spindle cells that are muscle cells and are stained by smooth muscle actin). It must be differentiated from neurofibromas, because the latter may be a marker of neurofibromatosis. Immunohistochemical staining shows positivity for S100 protein, collagen type IV and vimentin. The capsule may stain with epithelial membrane antigen. [2],[5]
Palisaded encapsulated neuroma is essentially a benign tumor without any association with neurofibromatosis or multiple endocrine neoplasia, type II. Excision is the treatment of choice. Even after incomplete excision the solitary circumscribed neuroma does not recur, a fact supporting a reactive rather than a neoplastic origin. [2],[3]
| 1. |
Reed RJ, Fine RM, Meltzer HD. Palisaded, encapsulated neuromas of the skin. Arch Dermatol 1972;106:865-70.
[Google Scholar]
|
| 2. |
Golod O, Soriano T, Craft N. Palisaded encapsulated neuroma-A classic presentation of a commonly misdiagnosed neural tumor. J Drugs Dermatol 2005;4:92-4.
[Google Scholar]
|
| 3. |
Koutlas IG, Scheithauer BW. Palisaded encapsulated ("solitary circumscribed") neuroma of the oral cavity: A review of 55 cases. Head Neck Pathol 2010;4:15-26.
[Google Scholar]
|
| 4. |
Omori Y, Tanito K, Ito K, Itoh M, Saeki H, Nakagawa H. A Pediatric Case of Multiple Palisaded Encapsulated Neuromas of the Palms and Soles. Pediatr Dermatol 2014;31:E107-9.
[Google Scholar]
|
| 5. |
Halder C, Sen S, Gangopadhyay A, Bala S. Zosteriform palisaded encapsulated neuroma: An unusual presentation. Indian J Dermatol 2013;58:492.
[Google Scholar]
|
Fulltext Views
9,815
PDF downloads
2,449





