Translate this page into:
Spectrum of periorbital dermatoses in South Indian population
Correspondence Address:
Rashmi Kumari
Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry 605 006
India
| How to cite this article: Besra L, Jaisankar TJ, Thappa DM, Malathi M, Kumari R. Spectrum of periorbital dermatoses in South Indian population. Indian J Dermatol Venereol Leprol 2013;79:399-407 |
Abstract
Background: Periorbital dermatoses are very common dermatological disorders which pose a diagnostic and therapeutic challenge for the treating dermatologist due to the similarity of symptoms in this area. Aims: To study the spectrum of periorbital dermatoses and to assess the association of systemic diseases with periorbital dermatoses. Methods: This was a hospital based descriptive study done on 250 consecutive patients irrespective of their age and sex who attended the Dermatology out patient department (OPD), with dermatological conditions pertaining to the periorbital area over a period of 2 years from October 2010 to September 2012. Results: The most common dermatological conditions seen in the periorbital region were benign and malignant skin tumors observed in 63 (25.2%) cases, followed by the disorders of pigmentation in 51 (20.4%) and eczema in 44 cases (17.6%), infections in 33 (13.2%) cases and nevoid conditions in 26 (10.4%) cases. Certain periorbital dermatoses were significantly more in females than in males in the present study like skin tags, connective tissue diseases, and periorbital melanosis (POM). Some periorbital dermatoses were significantly more common in older age group such as seborrheic keratoses, skin tags and airborne contact dermatitis whereas infections, syringomas, allergic contact dermatitis and atopic dermatitis were more prevalent in younger age group. Syringomas and POM were more common in middle-aged women. Conclusions: The most common dermatological condition seen in the periorbital region in this study are benign skin tumors (keratosis and skin tags), followed by the disorders of pigmentation and eczema, infections and nevoid conditions.Introduction
Periorbital dermatoses are dermatological manifestations of the area around the eyes including the eyelids. These are common disorders posing both diagnostic and therapeutic challenge for dermatologists. The similarity of symptoms in this area causes the diagnostic dilemma and the anatomic features like thin skin of the eyelids and proximity to the eyeball results in a therapeutic challenge. [1] It is also a vexing problem for the patient owing to the easy visibility of the region which is cosmetically distressing. Moreover, the anatomical differences pertaining to the area predisposes it to multiple dermatoses which sometimes localize specifically to the periorbital region.
Most of the literature regarding periorbital dermatoses is in form of case reports and few studies related to specific dermatoses. As there is lack of adequate data about the frequency and distribution of periorbital dermatoses in India, this study was undertaken in our institute with the aim of characterizing the spectrum of periorbital dermatoses and to assess the association of systemic diseases with periorbital dermatoses.
Methods
This was a hospital based descriptive study done in 250 consecutive patients who attended the Dermatology OPD, with dermatological conditions pertaining to the periorbital area over a period of 2 years from October 2010 to September 2012 after clearance obtained from institute ethical committee vide (SEC/2011/1/50; Dated: 24/2/2011).
The study group consisted of 250 consecutive patients with skin lesions in and around the orbit of varied etiology of both genders and all ages who attended the Dermatological OPD of our hospital. Non consenting patients with periorbital dermatoses were excluded from the study. A detailed history was taken after consent followed by localized cutaneous and general physical examination. Diagnosis was made after consensus opinion of two dermatologists in the OPD and relevant investigations were done. Relationship if any with occurrence of dermatoses and underlying systemic diseases were studied.
The collected data was tabulated in Microsoft Excel 2010 Worksheet and computer-assisted analysis was performed using IBM SPSS 20.0 (Chicago, IL, USA). Fisher′s exact test was used to assess the relationship between gender and periorbital dermatoses and to look for the association between skin tags and diabetes ANOVA was used to find the relation between age and occurrence of periorbital dermatoses.
Results
A total of 250 patients with periorbital dermatoses were included in the study. Among them, 156 (62.4%) were females and 94 (37.6%) were males with a male to female ratio of 1: 1.65. The most common age group affected by periorbital dermatoses in our study was 31-40 years (50 cases, 20%).
Most of the patients with periorbital dermatoses were asymptomatic (117 cases, 44%) and the most common symptom reported was itching seen in 111 (42%) patients.
Periorbital dermatoses encountered
The most common dermatological condition distributed in the periorbital region was benign and malignant skin tumors [Figure - 1] and [Figure - 2], pigmentary disorders, eczemas, infections and nevoid conditions. The various periorbital dermatoses encountered in our study are shown in [Table - 1].
 |
| Figure 1: Basal cell carcinoma overlying bilateral medial canthi and nasal bridge |
 |
| Figure 2: Extensive angiofibromas including upper eyelids |

Relationship between age and periorbital dermatoses
Periorbital tumors, dermatitis and pigmentation were more common among the middle and older age group when compared to periorbital infections which were common in the younger age group and this difference was statistically significant as seen in [Table - 2].

Periorbital tumors
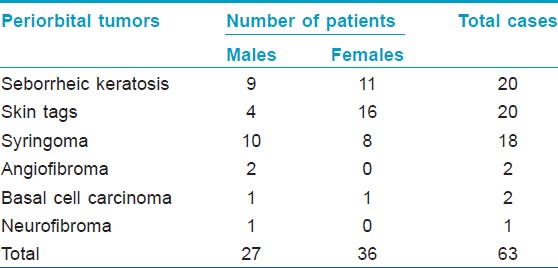
The most common periorbital tumors encountered in our study were seborrheic keratosis (SK) and skin tags observed in 20 patients each followed closely by syringoma in 18 patients. The distribution of periorbital tumors in our study is provided in [Table - 3]. Benign tumors (61 cases) were more in number than the malignant tumors (two cases).
Seborrheic keratosis
SK was the commonest periorbital tumor seen in our study along with skin tags in 20 patients. The mean age of patients was 56.3 ± 29.3 years. It was more common in females (11 cases) with a ratio of 1.2:1. The commonest type of SK in the elderly (51-60 years) was classical SK seen in 14 patients. Dermatosis papulosa nigra (DPN) was more common in the middle age group (31-40 years) seen in eight cases. Most of the cases (14) were asymptomatic and six cases had associated pruritus. The most commonly involved site by SK was bilateral periorbital area (10 cases), followed by bilateral infraorbital area (six cases). Rarely, forehead was involved (three cases).
Periorbital SK coexisted with periorbital skin tags and acanthosis nigricans in 12 patients each. Ten patients with SK had diabetes and eight patients were obese. SK in the periorbital region were more common in diabetics when compared to non-diabetics and this difference was statistically significant (p value by Fisher′s exact test < 0.0001)
Skin tags
Periorbital skin tags were seen in 20 patients in the study population. The mean age of the patients with periorbital skin tags was 51.1 ± 17.3 years. Skin tags in the periorbital region were more common in females (16 cases) when compared to males (four cases) with a male to female ratio of 1:4. Skin tags were most commonly found over the bilateral upper and lower eyelids seen in 10 patients followed by involvement of bilateral upper eyelid alone seen in five patients, lateral aspect of bilateral periorbital region in three patients, and lower eyelid alone in two patients. Periorbital skin tags coexisted with periorbital SK in 12 patients and with acanthosis nigricans in nine patients. Six patients were diabetics and 12 patients were obese. Skin tags in the periorbital region were more common in diabetics when compared to non-diabetics and this difference was statistically significant (p value by Fisher′s exact test = 0.001).
Syringoma
Syringoma was the second most common tumor in our study observed in 18 cases. The mean age of patients with syringoma was 35.6 ± 17.3 years. It was more common in males (10 cases) with a male to female ratio of 1.25:1. The commonest site of occurrence of syringoma in our study population was bilateral infraorbital areas (nine cases) followed by bilateral periorbital areas (nine cases). One male patient had extensive syringomas involving the entire face.
Relationship between age and gender and periorbital tumors
SK and skin tags were common in the elderly age group (50-60 years) and syringomas were more common in the middle age group (30-40 years) and this difference was statistically significant using ANOVA as given in [Table - 4]. Among the periorbital tumors encountered in the study population, female preponderance was more with skin tags when compared to the other tumors and this difference was statistically significant (p value by Fisher′s exact test < 0.015).

Periorbital pigmentation
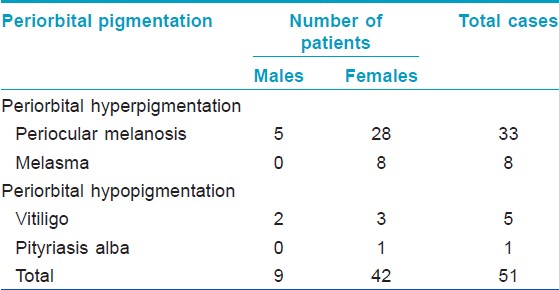
Periorbital pigmentation was the second common type of dermatosis encountered in our study observed in 55 patients. Hyperpigmentation in the periorbital region was more common (45 cases) compared to hypopigmentation in the periorbital region (10 cases). The different types of periorbital pigmentations observed in our study are shown in [Table - 5].
Periorbital hyperpigmentation
Out of the 41 patients who presented with hyperpigmentation in the periorbital area, majority (33 cases) were having periocular melanosis. The rest eight had melasma in the periorbital region.
Periocular melanosis
Among patients with periocular melanosis [Figure - 3], majority of our patients had excessive pigmentation in the periorbital distribution as a post inflammatory process secondary to dermatitis. The various types of periocular melanosis are shown in [Table - 6].
 |
| Figure 3: Infraorbital dark circles due to sagging and tear troughs |
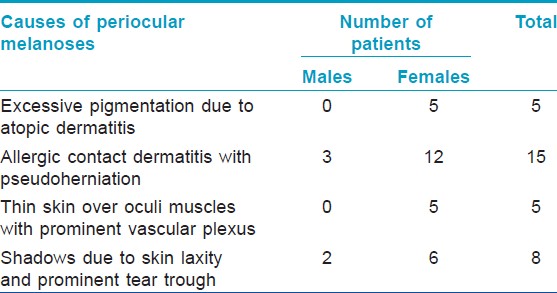
Periocular melanoses comprised the majority of periorbital pigmentary disorders seen in 33 cases. The mean age of the population with periocular melanoses was 34.1 ± 17.6 years. Females were more commonly affected (28 cases) than males (5 cases) with female to male ratio of 5.6:1. Periorbital melanosis (POM) had a female preponderance when compared to the other periorbital dermatoses and this difference was statistically significant (P value by Fisher′s exact test = 0.004).
Melasma
Melasma was exclusively seen in 8 females of all periorbital pigmentation. Mean age of the patients with melasma was 35.6 ± 18.2 years. Most common type of melasma seen was centrofacial with pigmentation over cheeks, nose and infraorbital area. Five patients had epidermal type, two had mixed type and one patient had dermal melasma.
Periorbital hypopigmentation
Hypopigmentation in the periorbital region consisted of only 10 cases. Five cases had vitiligo. The other causes of periorbital hypopigmentation included tinea versicolor, Hansen′s disease and pityriasis alba.
Periorbital dermatitis
Dermatitis in the periorbital area was the third most common cause of periorbital dermatoses observed in 44 patients. Exogenous eczema (31 cases) were more common causes compared to endogenous eczema (13 cases) in the periorbital region. Airborne contact dermatitis (ABCD) (20 cases) was the most common cause of exogenous eczema. The commonly implicated allergens by history were parthenium and cement. Patch test was carried out in five cases of which only two patients showed positivity to parthenolide and only one was positive to potassium dichromate. The various other causes of periorbital dermatitis are tabulated in [Table - 7].
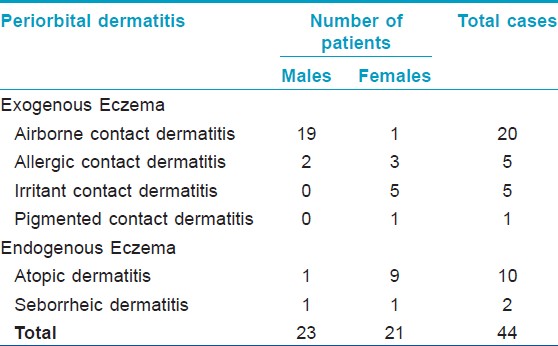
In our study, periorbital dermatitis was common in males when compared to the other periorbital dermatoses and this difference was statistically significant (p value by Fisher′s exact test = 0.04).
ABCD presenting in the periorbital region was more common in the elderly and in males (M: F = 19:1) when compared to allergic contact dermatitis (ACD) and atopic dermatitis and this difference was statistically significant (p value by Fisher′s exact test < 0.005 and p < 0.001 respectively) as given in [Table - 8].

Five patients, three females and two males, presented with ACD mainly involving lower eyelid. The allergens implicated were ophthalmic preparations - timolol eye drops, gentamicin sulfate ophthalmic ointment, and ciprofloxacin eye ointment in one patient each and nail polish and eye makeup in one female patient each. Irritant contact dermatitis comprised of five cases of periorbital dermatitis and all five were female patients. The various irritants implicated were hair dye, mascara, surma, phenylephrine eye drops and atropine eye drops in one patient each. Out of the twelve patients with endogenous eczema involving the periorbital region, isolated nonspecific eyelid dermatitis as part of atopic dermatitis was the most common cause seen in 10 patients and two patients had seborrheic dermatitis. There was a female preponderance in atopic dermatitis (F: M =9:1).
Periorbital infections
Infectious dermatoses involving the periorbital region included equal number of viral and bacterial infections (15 each) followed by two cases of tinea versicolor [Table - 9].
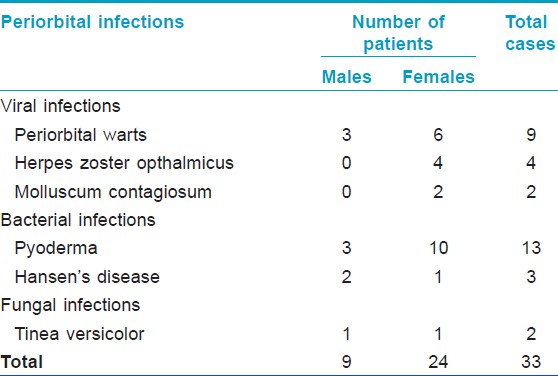
The commonest viral infection in the periorbital area was viral warts seen in nine patients, followed by herpes zoster ophthalmicus seen in four patients and molluscum contagiosum seen in two patients. The most common type of wart in the periorbital region was filiform warts seen in (six cases) followed by verruca vulgaris (three cases). Out of the twelve patients with pyoderma, impetigo was the most common seen in 11 patients and two patients had furuncle. Three patients with borderline tuberculoid Hansen′s disease were seen [Figure - 4].
 |
| Figure 4: Borderline tuberculoid Hansen's disease over left periorbital region |
Periorbital nevoid conditions
A total of 26 nevoid conditions were encountered in the study. Twenty one patients who presented to us for different periorbital dermatoses were found to have melanocytic nevi. The other six cases presented primarily for their nevoid condition which included nevus of Ota (3), port wine stain as part of Sturge Weber syndrome (1), verrucous epidermal nevus (1) [Figure - 5], café-au-lait macule (1) [Figure - 6]. All 3 patients with nevus of Ota were females.
Other miscellaneous periorbital dermatoses [Figure - 7], [Figure - 8], [Figure - 9] seen in our study are as shown in [Table - 10].
 |
| Figure 5: Verrucuous epidermal naevus |
 |
| Figure 6: Periorbital café au lait macule (left side) |
 |
| Figure 7: Alopecia universalis affecting eyebrows and eyelashes |
 |
| Figure 8: Cutaneous horn over left upper eyelid |
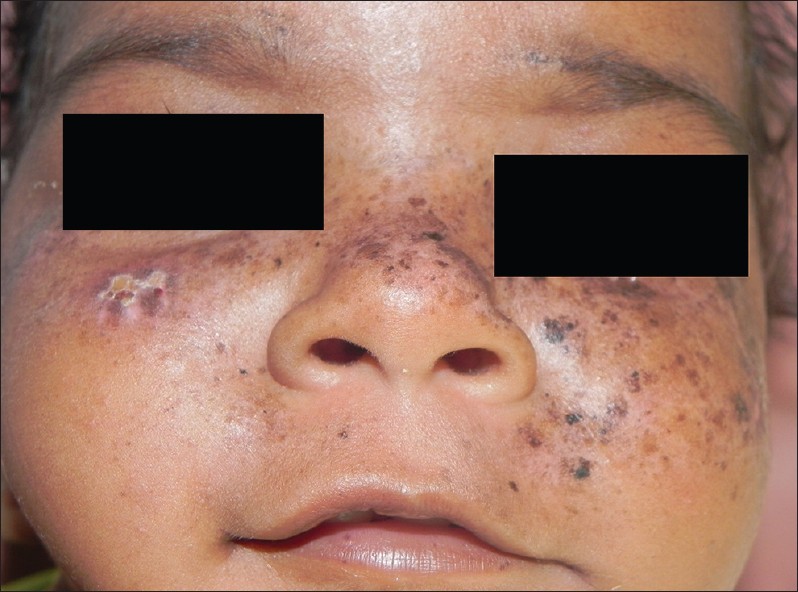 |
| Figure 9: Xeroderma pigmentosum in a child |

Discussion
Periorbital region is predisposed to multiple dermatoses and all types of skin disorders will affect this region. The periorbital area owing to its easy visibility makes the condition psychologically distressing to the patient. There are various ways to classify them of which the most reliable one is according to their nature and morphology. [1]
The common periorbital disorders encountered in decreasing order of frequency in the present study include tumors, pigmentary disorders, eczematous conditions, infections and nevoid conditions. Surprisingly, there were no similar previous studies regarding the prevalence of the spectrum of periorbital dermatoses in Indian scenario and world literature to compare our data.
Certain dermatoses in this study of various skin diseases in periorbital area were significantly more commonly seen in females than in males in our study like skin tags, (16/20) connective tissue diseases (10/10) and periorbital pigmentation. (28/34) Similarly, certain dermatoses were significantly more in older age groups, like seborrheic keratoses (56 ± 29.3 years), skin tags (51.1 ± 17.3 years) and ABCD (50.7 ± 13.7 years). Syringomas (35.6 ± 17.3 years) and periocular melanosis (34.1 ± 17.6 years) were found to be prevalent among middle age group. ACD was common among younger age group (26.8 ± 17.3 years).
In our study, tumors were the commonest dermatoses encountered in the periorbital area probably due to the fact that 50% of our study population comprised of patients belonging to middle age group. As expected, benign tumors were more common as compared to malignant tumors. In a retrospective study of 80 patients with benign eyelid and conjunctival tumors, the most frequent tumor was intradermal nevus (44.6%), SK (16.1%), and compound nevus (10.7%) in eyelid tumors. [2] However, in our study SK were the most common benign tumours encountered in the periorbital region. SK are more common with increasing age and DPN, a genetic form of SK is common in blacks, seen even in young and middle-aged people. [2],[3] In our study also, DPN was more common among the younger age group and classical SK was common among the elderly.
Skin tags or acrochordons, are common benign connective tissue tumors of the dermis, frequently found on the eyelids, but may also be found anywhere on the body, particularly in women with advancing age. [2],[4] , Bhargava and Mathur [5] in their study on 100 patients with acrochordons, reported neck to be the most common site for skin tag in 90%, followed by axilla in 38% and eyelid in 34%. They also observed that skin tags were most commonly associated with obesity and diabetes mellitus and pseudoacanthosis nigricans. In present study skin tags were the second common benign tumor affecting the periorbital region and were more common in females and in the elderly age group. We also observed SK to be commonly associated with skin tag in concordance with the view that acrochordons, pseudoacanthosis nigricans and seborrhoeic keratosis represent proliferative skin conditions where growth factors are involved. [5]
Syringomas are common benign eccrine ductal adnexal tumors with no malignant potential, commonly found on the lower eyelids and malar area but may also be present on the forehead, chest, and abdomen. [2],[6] They are found at any age but occur more commonly in the third and fourth decades [2] and in women. [7] Al Aradi et al., [7] in their study found females to be affected more often than males. In the present study, syringomas were more common in the third and fourth decade but, in contrast to Al Aradi′s study, [7] syringomas were more common in males. Palpebral syringomas are a common cutaneous pathology in Downs syndrome [4] but we did not observe any such association in the present study.
Basal cell carcinoma (BCC) is the most common malignancy affecting the periorbital area worldwide accounting for 80-90% of all eyelid cancers in Western literature. [2],[8] It presents more commonly on the lower eyelid and medial canthus. [2] Becher et al. [9] also found that the lower eyelid to be the commonest site of linear BCC. Including their three patients, 14 of 42 reported cases (33%) have been located in this anatomical location. In the present study, BCC was the only malignant tumor seen in the periorbital location in two patients and both of them had BCC involving the medial canthus-one was noduloulcerative BCC and the other was morpheaform BCC.
POM, also known as "dark circles," "infraorbital skin discoloration," "infraorbital darkening," "some darkening of the skin around the eyes," is an ill-defined entity and is of common cosmetic concern. POM can be due to four major causes: Dermal melanin deposition, post inflammatory hyperpigmentation from atopic or contact allergic dermatitis, shadowing from lax skin and infraorbital swelling. [10],[11] Stretching the skin is an easy test to differentiate post inflammatory hyperpigmentation from other causes due to vascularity, lax skin, tear trough etc., which occur as part of ageing changes. Because various factors cause infraorbital dark circles, it is essential to identify the cause before appropriate treatment can be initiated. In our study, the most common cause of POM was post inflammatory pigmentation secondary to atopic or ACD.
Periorbital dermatitis is often of multifactorial origin. It may be acute or chronic and it may be the dominating skin problem or part of a more wide spread skin disorder. Endogenous and exogenous factors are often involved. [12] Patients presenting with eyelid dermatitis are often a challenge to diagnose and treat despite an extensive history and physical examination. Potential causes of eyelid dermatitis include ACD, irritant contact dermatitis, atopic dermatitis, seborrhoeic dermatitis, psoriasis, dermatomyositis, infections, rosacea, and others. Eyelid dermatitis may be the result of a combination of many factors like ACD superimposed on a primary non-allergic dermatitis such as atopic eczema or seborrhoeic dermatitis.
The eyelids are susceptible to ACD owing to their very thin, pliable and soft skin which allows for easier penetration of both contact and airborne allergens. [1],[2],[13] The eyelids are particularly predisposed to ABCD because they are exposed and materials may lodge and get deposited on the upper eyelids. Hence there is also ABCD, caused by things such as pollen, dust mites, animal dander, and chemicals suspended in the air. [2] ABCD was by far the most common type of exogenous dermatitis occurring in the periorbital region in the present study with the commonly implicated allergens being parthenium and cement.
ACD as the etiology of eyelid dermatitis in various studies ranges from 46-65% and in the present study it was the cause in 11.36% of cases of eyelid dermatitis. It has been noted that elderly patients had a higher tendency for contact dermatitis to be allergic rather than irritant in nature and women were affected more commonly. In the present study, also women were more commonly affected with ACD and ICD. The common allergens implicated in eyelid dermatitis from various studies include topical pharmaceutic products (antibiotics, corticosteroids), cosmetics (fragrance components, preservatives, emulsifiers, hair care and nail products), metals (nickel), rubber derivatives, resins (e.g., epoxy resin), and plants. In the present study, the allergens implicated based on history were ophthalmic preparations (timolol eye drops, gentamicin ointment and ciprofloxacin ointment), eye makeup and nail polish but we could not confirm it by patch testing. ACD can also exist "ectopically" on the eyelids, with allergens spread beyond the primary site of contact as observed in the present study wherein one patient had ACD to nailpolish manifesting as eyelid dermatitis. Irritant contact dermatitis as a cause of eyelid dermatitis from various studies [2] ranges from 15-24% and in the present study, it was 11.36%. The various irritants implicated were hair dye, mascara, surma, phenylephrine eye drops and atropine eye drops.
Atopic dermatitis as a cause of eyelid dermatitis from various studies ranges from 14-39% [2] and in the present study it was 22.72%. The eyelids are commonly involved in atopic dermatitis because they are thin, exposed to irritants, and more easily traumatized by scratching. Constant rubbing leads to chronic changes and inflammation of the eyelid. The upper eyelids were more commonly involved than the lower eyelids. The more chronic the eruption, the darker and more lichenified the lesions become. Many eye changes occur in association with atopic dermatitis like conjunctivitis, keratoconjunctivitis, loss of eyelashes, lid edema, tearing, chemosis, and mucoid discharge. But these changes were not observed in our patients as most of the patients presented in the chronic stage when lichenification had set in. The presence of an extra fold under the lower eyelids called the Dennie-Morgan fold is a clue to the presence of atopy which was observed in 8 of our patients. "Allergic shiners" are dark circles around the eyes secondary to venous congestion is one of the minor criteria for diagnosis of atopic dermatitis and was present in 20 patients in the present study.
When seborrheic dermatitis involves periocular tissue (the eyebrows and eyelids), it is known as seborrheic blepharitis. Ocular complications of chronic seborrhea of the eyelids include hordeola (styes) and inflammation of the meibomian glands (meibomianitis) with secondary conjunctivitis (blepharoconjunctivitis). In the present study, only two patients presented with seborrheic blepharitis as most of the patients are managed by ophthalmologists in our hospital.
In the present study, we had an equal number of bacterial and viral infections occurring in the periorbital area probably because most of the common bacterial infections like stye, chalazion are commonly managed by ophthalmologists in our hospital and not referred to us. Flat warts are often seen on the face and eyelids whereas the more hyperkeratotic common warts do not normally occur on the eyelids. [2] In the present study, most of the patients of periorbital verrucae were filiform in morphology and a few had common warts but none of them had plane warts.
The periorbital region is a common site for the occurrence of certain specific nevoid conditions like nevus of Ota, port wine stain along the distribution of trigeminal nerve occurring as a component of Sturge Weber syndrome occur on the face is also seen in this study. [14]
Certain dermatoses have a specific predilection for the periorbital area like tumors (benign like SK, skin tags, acquired melanocytic nevi and malignant like BCC), allergic and ABCD, POM, as seen in the present study. Due to easy visibility over the face most patients present to dermatologist for cosmetic concerns or itching. While prescribing any topical medication the dermatologist has to keep in mind the ocular complications owing to the thin and sensitive nature of the skin in the periorbital area and close proximity to the eye. Certain specific periorbital lesions aid in diagnosing the underlying systemic conditions like heliotrope rash in dermatomyositis, malar rash in systemic lupus erythematosus (SLE), beading of eyelids in lipoid proteinosis, xanthelasma in hyperlipidemia, Dennie Morgan fold in atopic dermatitis, etc., Hence, examination of the periorbital area has both diagnostic and therapeutic implications and should be an essential component of all dermatological examinations.
To conclude, the most common dermatological condition seen in the periorbital region are benign and malignant skin tumors (seborrhoeic keratosis and skin tags), followed by the disorders of pigmentation and eczema, infections and nevoid conditions. In future, more focused studies elucidating the causes of eyelid dermatitis may be more productive and meaningful.
| 1. |
Rebora A. Periorbital lesions. Clin Dermatol 2011;29:151-6.
[Google Scholar]
|
| 2. |
Peralejo B, Beltrani V, Bielory L. Dermatologic and allergic conditions of the eyelid. Immunol Allergy Clin North Am 2008;28:137-68.
[Google Scholar]
|
| 3. |
Yeatman JM, Kilkenny M, Marks R. The prevalence of seborrhoeic keratoses in an Australian population: Does exposure to sunlight play a part in their frequency? Br J Dermatol 1997;137:411-4.
[Google Scholar]
|
| 4. |
Ellis DL, Kafka SP, Chow JC, Nanney LB, Inman WH, McCadden ME, et al. Melanoma, growth factors, acanthosis nigricans, the sign of Leser-Trélat, and multiple acrochordons. A possible role for alpha-transforming growth factor in cutaneous paraneoplastic syndromes. N Engl J Med 1987;317:1582-7.
[Google Scholar]
|
| 5. |
Bhargava P, Mathur SK, Mathur DK, Malpani S, Goel S, Agarwal US, et al. Acrochordon, diabetes and associations. Indian J Dermatol Venereol Leprol 1996;62:226-8.
[Google Scholar]
|
| 6. |
Patrizi A, Neri I, Marzaduri S, Varotti E, Passarini B. Syringoma: A review of twenty-nine cases. Acta Derm Venereol 1998;78:460-2.
[Google Scholar]
|
| 7. |
Al Aradi IK. Periorbital syringoma: A pilot study of the efficacy of low-voltage electrocoagulation. Dermatol Surg 2006;32:1244-50.
[Google Scholar]
|
| 8. |
Margo CE, Waltz K. Basal cell carcinoma of the eyelid and periocular skin. Surv Ophthalmol 1993;38:169-92.
[Google Scholar]
|
| 9. |
Becher GL, Affleck A, Fleming C, Evans A. Linear basal cell carcinoma occurs most commonly on the lower eyelid. Clin Exp Dermatol 2011;36:311-2.
[Google Scholar]
|
| 10. |
Malakar S, Lahiri K, Banerjee U, Mondal S, Sarangi S. Periorbital melanosis is an extension of pigmentary demarcation line-F on face. Indian J Dermatol Venereol Leprol 2007;73:323-5.
[Google Scholar]
|
| 11. |
Roh MR, Chung KY. Infraorbital dark circles: Definition, causes, and treatment options. Dermatol Surg 2009;35:1163-71.
[Google Scholar]
|
| 12. |
Borch JE, Elmquist JS, Bindslev-Jensen C, Andersen KE. Phenylephrine and acute periorbital dermatitis. Contact Dermatitis 2005;53:298-9.
[Google Scholar]
|
| 13. |
Ayala F, Fabbrocini G, Bacchilega R, Berardesca E, Caraffini S, Corazza M, et al. Eyelid dermatitis: An evaluation of 447 patients. Am J Contact Dermat 2003;14:69-74.
[Google Scholar]
|
| 14. |
Dart JK, Leonard JN. The skin and the eyes. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8 th ed. Oxford: Blackwell Publishing; 2010; p. 67.1-67.37.
th ed. Oxford: Blackwell Publishing; 2010; p. 67.1-67.37.'>[Google Scholar]
|
Fulltext Views
9,742
PDF downloads
2,934





