Translate this page into:
Squamous cell carcinoma in long-standing chromoblastomycosis
Corresponding Author:
K Vivekanandh
Room No. 201, Metro Manorama Complex, Kathagola Road, Mangalabag, Cuttack - 753 001, Odisha
India
dr.vivekanandh@gmail.com
| How to cite this article: Mohanty P, Vivekanandh K, Mohapatra L, Dash G. Squamous cell carcinoma in long-standing chromoblastomycosis. Indian J Dermatol Venereol Leprol 2017;83:363-365 |
Sir,
Chromoblastomycosis is a slowly progressive mycosis affecting the skin and subcutaneous tissue.[1] It is caused by dematiaceous, naturally pigmented fungi, which exist as saprophytes in the soil and in decaying vegetation. Common etiologic agents are Cladophialophora carrionii and Fonsecaea pedrosoi.[2] The definite incidence is not known, as there are only sporadic reports in literature.[1] It usually occurs after penetrative trauma with vegetative matter and affects middle-aged male agricultural workers, usually, of the tropical and subtropical regions of the world. Long-standing cases can rarely undergo malignant change.[1],[2]
A 70-year-old male farmer presented with an asymptomatic atrophic crusted plaque, covering the entire dorsum of the left foot for the past 15 years. On examination, the non-tender plaque was approximately 10 cm × 12 cm in size, with black to brownish dots on a yellowish crusted surface with variable atrophy and depigmentation at most places [Figure - 1]. He, initially, had a nodule of about 0.5 cm2 size, which gradually progressed to the present size and was not associated with any constitutional features. The patient was otherwise well. He could not recall any history of trauma. Clinically, the differential diagnoses of chromoblastomycosis and lupus vulgaris were considered. Routine investigations were normal. Potassium hydroxide mount showed sclerotic bodies. Histopathology showed pseudoepitheliomatous hyperplasia, suppurative granulomas and sclerotic bodies, which was consistent with chromoblastomycosis [Figure - 2]. Fungal culture with lactophenol cotton blue preparation showed septate fungal hyphae with acropetal long chains of conidia suggestive of Cladosporium carrionii.
 |
| Figure 1: Pretreatment picture showing single atrophic, crusted plaque over left foot |
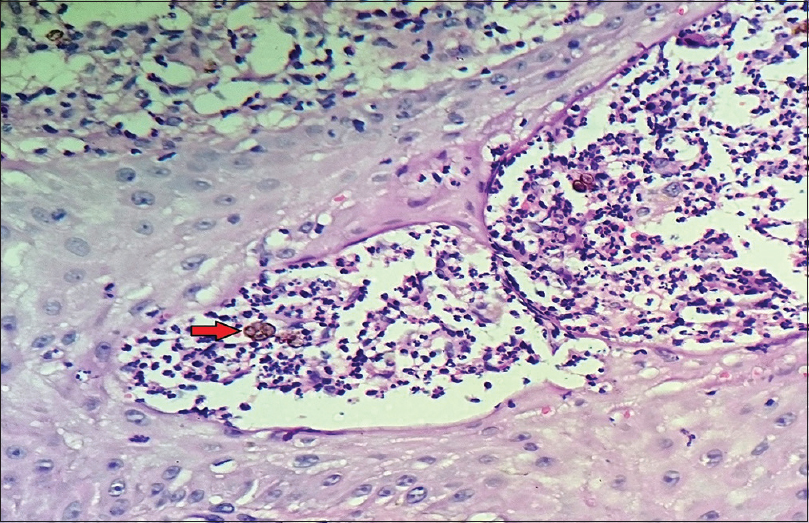 |
| Figure 2: Sclerotic bodies (arrow) (H and E, ×400) |
The patient was then treated with terbinafine 250 mg, one tablet twice daily and local heat therapy by applying hot water bag 2–3 times a day for 6 months. There was a significant decrease in size, verrucosity and clearing of the dots; however, in one part of the lesion, there was no improvement. Rather, there was a gradual development of an ulcer of size 10 cm × 7 cm with ill-defined margins, everted edges, a floor of poor granulation tissue, indurated base and normal surrounding skin with no evidence of any discharge or regional lymphadenopathy [Figure - 3]. As there was progression of the ulcer after 6 months of therapy, we suspected a malignancy and did an incisional biopsy which showed malignant squamous cells arranged in sheets and nests, infiltrating into the dermis, with pleomorphic cells with high nuclear-cytoplasmic ratio, keratin pearls and inflammatory cells in the background, consistent with squamous cell carcinoma [Figure - 4]. The patient was referred to oncosurgery department, where he was advised to undergo excision, after which the patient was lost to follow-up.
 |
| Figure 3: Ulcer with everted edges over the plaque after 6 months of treatment |
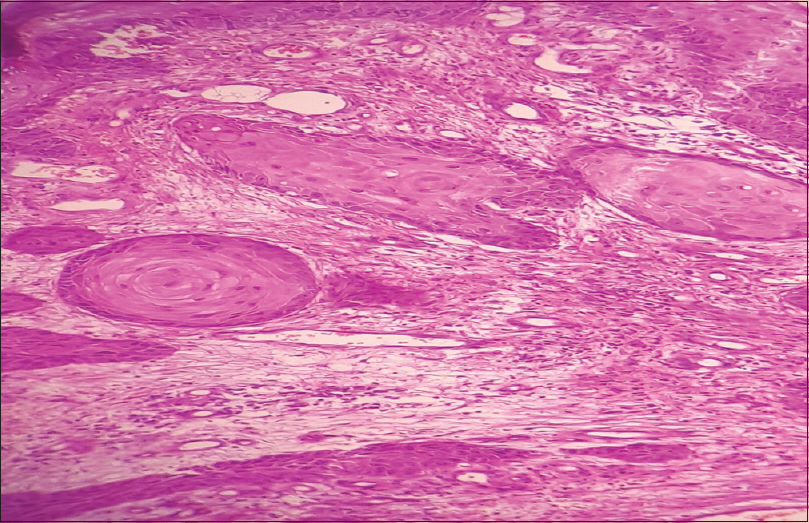 |
| Figure 4: Malignant squamous cells infiltrating into dermis (H and E, ×100) |
Chromoblastomycosis is a chronic granulomatous infection, usually of exposed areas. It usually presents as warty plaques, nodules or cauliflower-like growths. Six clinical variants have been identified: Nodular, verrucous or vegetative (53%), tumoral, plaque (41%), psoriasiform, cicatricial and elephantiasic; in addition to occasional other, atypical forms.[1] Infection occurs due to the introduction of organisms into tissues by a wooden splinter or abrasion of skin. In histologic sections, fungi are visible as dark brown, thick-walled spherical bodies of 5–15 μm diameter (sclerotic bodies).[3] Complications include hematogenous spread, secondary infection and rarely malignancy.[1] Malignancy is insidious in onset, arising between 20 and 30 years from the acquisition of infection. There have been reports that the presence of chronic inflammation and scarring may predispose to squamous cell carcinoma.[1] Limbs are most commonly affected by malignant transformation, as it is a common site for chromoblastomycosis.[2] In one study carried out in Brazil, among 100 patients who had chromoblastomycosis over a mean duration of 14 years, two patients developed squamous cell carcinoma. In a case report by Torres et al., malignancy developed after 30 years of the disease.[1] In another study carried out in Madagascar, malignant transformation was reported in 14 out of 1400 cases over 50 years. Only 17 such cases have been documented worldwide.[1] It is usually treated with itraconazole 200–400 mg/day or terbinafine 250–500 mg/day for a mean period of 6–12 months. In a study by Esterre et al., 6–12 months of terbinafine at a dosage of 500 mg/day was administered orally to 43 patients, with a diagnosis of chromomycosis. Mycological cure, as judged by skin scrapings, was observed in 41.4%, 74.1% and 82.5% of patients infected with F. pedrosoi after 4, 8 and 12 months of therapy, respectively. The efficacy of terbinafine in C. carrionii infected patients seemed even higher.[4] Other drugs include potassium iodide, amphotericin B, fluconazole and 5-fluorocytosine. Excision, cryosurgery, local heat therapy, curettage with electrodesiccation and laser are used as adjuncts to antifungals. In advanced cases, a combination of medical and surgical treatment is recommended.[2]
In our case, the patient had the lesion for 15 years, on the dorsum of the left foot. After treatment, there was a good response in one side of the lesion while the other side developed ulceration and squamous cell carcinoma. One has to suspect malignancy in the case of any suspicious change in the morphology of long-standing lesions, such as the development of ulceration or growth, along with poor response to treatment. High index of suspicion and early histological diagnosis helps in preventing complications. We found only one case previously reported in India.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | Torres E, Beristain JG, Lievanos Z, Arenas R. Chromoblastomycosis associated with a lethal squamous cell carcinoma. An Bras Dermatol 2010;85:267-70. [Google Scholar] |
| 2. | Jamil A, Lee YY, Thevarajah S. Invasive squamous cell carcinoma arising from chromoblastomycosis. Med Mycol 2012;50:99-102. [Google Scholar] |
| 3. | Mittal A, Agarwal N, Gupta LK, Khare AK. Chromoblastomycosis from a non-endemic area and response to itraconazole. Indian J Dermatol 2014;59:606-8. [Google Scholar] |
| 4. | Esterre P, Inzan CK, Ramarcel ER, Andriantsimahavandy A, Ratsioharana M, Pecarrere JL, et al. Treatment of chromomycosis with terbinafine: Preliminary results of an open pilot study. Br J Dermatol 1996;134 Suppl 46:33-6. [Google Scholar] |
| 5. | Jacob M, Mathal R, Prasad P, Bhaktaviziam A. Chromoblastomycosis with squamous cell carcinoma. Indian J Dermatol Venereol Leprol 1988;54:314-7. [Google Scholar] |
Fulltext Views
2,668
PDF downloads
1,393





