Translate this page into:
Squamous cell carcinoma of the nail fold masquerading as pyogenic granuloma
2 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
3 Department of Virology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Saurabh Singh
Department of Dermatology, Venereology and Leprology, Employees' State Insurance Corporation Medical College and Hospital, NH-3, NIT, Faridabad, Haryana
India
| How to cite this article: Khullar G, Singh S, Saikia UN, Kumar A, Singh MP, Kanwar AJ. Squamous cell carcinoma of the nail fold masquerading as pyogenic granuloma. Indian J Dermatol Venereol Leprol 2016;82:555-557 |
Sir,
Squamous cell carcinoma involving the nail unit is rare, and diagnosis may be delayed as it may mimic benign dermatoses. In view of its varied clinical manifestations, a high index of suspicion and a low threshold for histopathological examination are vital for making an early diagnosis. We report a case of squamous cell carcinoma of the lateral nail fold of the left thumb, that simulated pyogenic granuloma.
A 65-year-old man presented with a 0.5 mm sized pinkish nodule located on the lateral nail fold of the left thumb for the past 2 months. He related his current symptoms to minor trauma sustained while clipping his nails, 18 years earlier; this was followed by pain and redness, which had a waxing and waning course. Intermittent use of oral antibiotics and topical antibiotic-steroid combination creams gave him temporary relief. With differential diagnoses of pyogenic granuloma and hypertrophic granulation tissue, the nodule was treated with silver nitrate (1%) cautery every 2 weeks for almost 2 months. Two months later, he noticed a relatively rapid increase in the size of the growth which had expanded into an 1.5 cm × 1 cm erythematous moist plaque that covered the adjoining lateral one-third of the nail plate [Figure - 1]a. The plaque showed mild serous ooze on pressure and yellowish-brown crusting. There was no history of bleeding or pus discharge. Regional lymphadenopathy was absent. A skin biopsy was performed from the lateral nail fold with the differential diagnoses of pyogenic granuloma, hypertrophic granulation tissue and squamous cell carcinoma. The biopsy showed features of squamous cell carcinoma in situ. X-ray of the left thumb was unremarkable. Consequently, the thumb was disarticulated at the interphalangeal joint (at the plastic surgery department) [Figure - 1]b and the excised specimen showed features of moderately differentiated squamous cell carcinoma [Figure - 2], with free margins. Genotypic analysis with polymerase chain reaction using primers targeting upstream regulatory region for human papillomavirus 16 and E6 region for human papillomavirus 18 was negative.[1] No recurrence was evident after 4 years of follow-up.
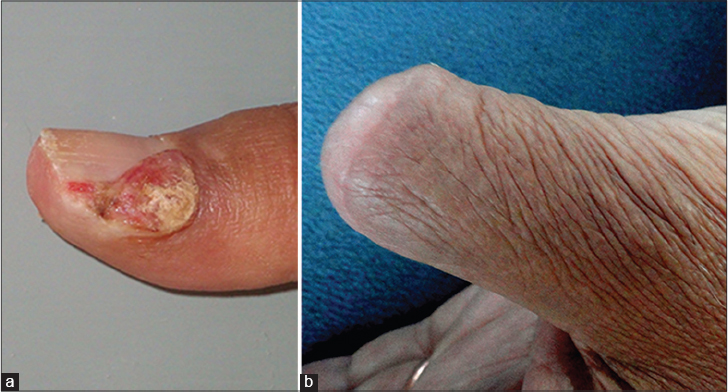 |
| Figure 1: (a) Erythematous moist plaque arising from the lateral nail fold of the left thumb and covering the adjoining lateral one-third of the nail plate with crusting at multiple sites, (b) disarticulated thumb at interphalangeal joint after excision of carcinoma |
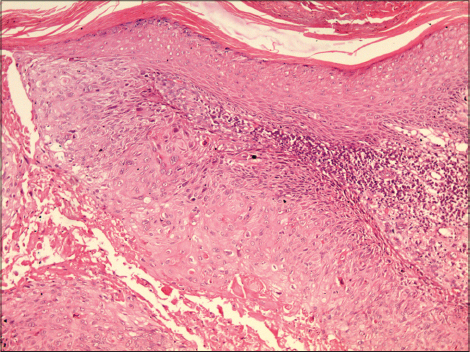 |
| Figure 2: Bulbous dermal extension from the epidermis showing pleomorphic keratinocytes with vesicular nuclei and prominent nucleoli, apoptotic bodies and architectural disarray. The underlying dermis has a moderate lympho-mononuclear infiltrate (H and E, ×200) |
Squamous cell carcinoma of the nail unit is exceedingly uncommon; the reported incidence ranges from 0.0012% of hospital admissions to 0.028% of dermatologic outpatients.[2] It is the most common malignant tumor of the nail apparatus and is usually slow growing; the mean delay in diagnosis was found to be 6 years and 4 months in a study.[3] The nail fold lies unprotected by the nail plate making it susceptible to trauma as observed in our patient. The other predisposing factors for digital squamous cell carcinoma include infection, chemical carcinogens, chronic inflammation, arsenic exposure, ionizing radiation, actinic damage and immunosuppression. Digital squamous cell carcinoma has been associated with α-human papillomavirus infection, most commonly human papillomavirus 16 in 89% of the cases and less commonly, other high-risk strains.[4],[5]
Our case was unusual as the majority of squamous cell carcinomas of the nail unit originate from the nail bed and primary involvement of the lateral nail fold is less frequent.[6] In a Belgian study evaluating 54 squamous cell carcinomas of the nail unit, 57.4% were localized to the nail bed, 31.5% to the periungual area and 11.1% to both the sites on histopathology.[3] Kreuter et al. reported periungual lesions in 24% of patients with squamous cell carcinoma/squamous cell carcinoma in situ of the hands.[5] The clinical resemblance of the tumor to pyogenic granuloma in our patient was also unusual. Squamous cell carcinoma of the lateral nail fold may have diverse clinical presentations; it most commonly presents as a verrucous plaque with scaling or erosion, or an ulcerated lesion with crusting; rarer presentations include granulomatous swelling, paronychia, oozing, hyperpigmented flat plaque, granulation tissue or pyogenic granuloma-like. Lecerf et al. reported a pyogenic granuloma-like presentation in 15.7% cases of squamous cell carcinoma of the nail complex.[3]
Bone invasion has been reported in 18–60% of cases of squamous cell carcinoma of the nail apparatus.[3] Although traditionally, distal amputation has been performed for all squamous cell carcinomas of the nail unit, of late, tissue-conserving Moh's micrographic surgery is being increasingly encouraged in the absence of radiographic evidence of bone involvement.[7],[8],[9] The general recommendation is to do conservative surgery if <50% of the nail surface is involved [10] but in view of the non-availability of micrographic surgery, long-standing nature of the disease in an elderly individual and uncertainty of long-term follow-up, distal amputation was performed in our case.
Squamous cell carcinoma must, therefore, be included in the differential diagnoses of benign looking nail fold lesions that do not respond to conservative therapies. Although biopsy in some cases may reveal squamous cell carcinoma in situ, they should still be treated on the lines of squamous cell carcinoma as invasion may be missed in superficial biopsies due to the complex three-dimensional structure of nail.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Shukla S, Bharti AC, Mahata S, Hussain S, Hedau S, Sharma R, et al. Application of a multiplex PCR to cervical cells collected by a paper smear for the simultaneous detection of all mucosal human papillomaviruses (HPVs) and typing of high-risk HPV types 16 and 18. J Med Microbiol 2010;59(Pt 11):1303-10.
[Google Scholar]
|
| 2. |
High WA, Tyring SK, Taylor RS. Rapidly enlarging growth of the proximal nail fold. Dermatol Surg 2003;29:984-6.
[Google Scholar]
|
| 3. |
Lecerf P, Richert B, Theunis A, André J. A retrospective study of squamous cell carcinoma of the nail unit diagnosed in a Belgian general hospital over a 15-year period. J Am Acad Dermatol 2013;69:253-61.
[Google Scholar]
|
| 4. |
Alam M, Caldwell JB, Eliezri YD. Human papillomavirus-associated digital squamous cell carcinoma: Literature review and report of 21 new cases. J Am Acad Dermatol 2003;48:385-93.
[Google Scholar]
|
| 5. |
Kreuter A, Gambichler T, Pfister H, Wieland U. Diversity of human papillomavirus types in periungual squamous cell carcinoma. Br J Dermatol 2009;161:1262-9.
[Google Scholar]
|
| 6. |
Figus A, Kanitkar S, Elliot D. Squamous cell carcinoma of the lateral nail fold. J Hand Surg Br 2006;31:216-20.
[Google Scholar]
|
| 7. |
Lumpkin LR 3rd, Rosen T, Tschen JA. Subungual squamous cell carcinoma. J Am Acad Dermatol 1984;11(4 Pt 2):735-8.
[Google Scholar]
|
| 8. |
Attiyeh FF, Shah J, Booher RJ, Knapper WH. Subungual squamous cell carcinoma. JAMA 1979;241:262-3.
[Google Scholar]
|
| 9. |
Peterson SR, Layton EG, Joseph AK. Squamous cell carcinoma of the nail unit with evidence of bony involvement: A multidisciplinary approach to resection and reconstruction. Dermatol Surg 2004;30 (2 Pt 1):218-21.
[Google Scholar]
|
| 10. |
Dalle S, Depape L, Phan A, Balme B, Ronger-Savle S, Thomas L. Squamous cell carcinoma of the nail apparatus: Clinicopathological study of 35 cases. Br J Dermatol 2007;156:871-4.
[Google Scholar]
|
Fulltext Views
3,995
PDF downloads
1,596





