Translate this page into:
Storiform pattern in dermatopathology
Corresponding author: Dr. Biswanath Behera, Department of Dermatology and Venereology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. biswanathbehera61@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gowda SK, Behera B, Sethy M, Ayyanar P, Garg S. Storiform pattern in dermatopathology. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_791_2024
Introduction
The diagnosis of skin and soft tissue tumours can be challenging at times. The pattern in dermatopathology represents a specific arrangement of tumour cells, stroma, or both within the tumour mass. Various patterns described in dermatopathology are pagetoid pattern, storiform, interstitial, palisading, petaloid, rosette, ripple, and others. The term ‘storiform’ was derived from the Latin word ‘storea’, which means ‘matting’, and was coined by Bednar in the year 1957. It depicts a typical pattern of a star-like ‘spiral nebula’, spoke-like ‘whorling’, and ‘rosette’ arrangement of cells and fibres [Figure 1a-1d].1 It is better appreciated under low magnification and with silver impregnation. This paper attempts to summarise the dermatological conditions, where the storiform pattern is visualised, and additional clues in arriving at a diagnosis.
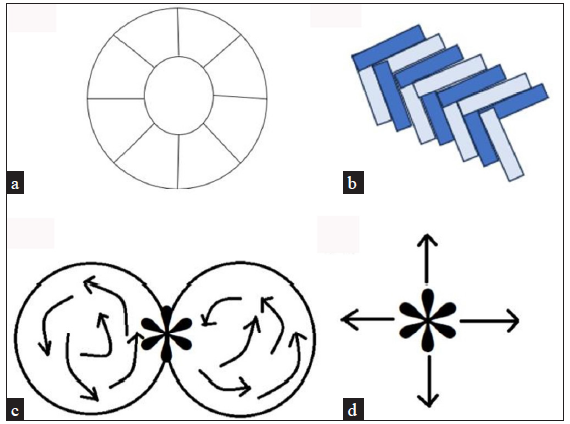
- Schematic diagram of various storiform patterns; a) Cartwheel pattern radiating from a central hub, b) Woven pattern with right angle bundles/fascicles, c) Whorl-like pattern, d) Pinwheel pattern radiating from a central point.
Dermatofibroma
Early lesions of dermatofibroma are more cellular and later become sclerotic. It is a circumscribed non-encapsulated dermal tumour with a Grenz zone. It comprises spindled fibroblasts and histiocytes, classically arranged in a storiform pattern [Figures 2a, 2b and 2c].1

- Dermatofibroma presenting as a brown firm nodule.
![Histopathology of dermatofibroma shows spindle cells in a storiform pattern [Haematoxylin and eosin, 50x].](/content/126/2024/0/1/img/IJDVL_791_2024-g3.png)
- Histopathology of dermatofibroma shows spindle cells in a storiform pattern [Haematoxylin and eosin, 50x].
![Histopathology of dermatofibroma shows fibroblasts and epithelioid-shaped histiocytes [Haematoxylin and eosin, 100x].](/content/126/2024/0/1/img/IJDVL_791_2024-g4.png)
- Histopathology of dermatofibroma shows fibroblasts and epithelioid-shaped histiocytes [Haematoxylin and eosin, 100x].
Dermatofibrosarcoma protuberans (DFSP)
Histopathological examination of DFSP reveals monomorphic spindle cells loosely scattered in the dermis in a storiform pattern [Figures 3a, 3b, and 3c] and extend into subcutis to form a honeycomb pattern.1

- Dermatofibrosarcoma protuberance presenting as a protuberant hypopigmented to skin-coloured nodule over the lower abdomen.
![Histopathology of dermatofibrosarcoma protuberance reveals spindled cells arranged in a storiform pattern. [Haematoxylin and eosin, 100x].](/content/126/2024/0/1/img/IJDVL_791_2024-g6.png)
- Histopathology of dermatofibrosarcoma protuberance reveals spindled cells arranged in a storiform pattern. [Haematoxylin and eosin, 100x].
![Immunohistochemistry of dermatofibrosarcoma protuberance demonstrates positive staining for CD34 [IHC, 100x].](/content/126/2024/0/1/img/IJDVL_791_2024-g7.png)
- Immunohistochemistry of dermatofibrosarcoma protuberance demonstrates positive staining for CD34 [IHC, 100x].
Cutaneous Rosai-Dorfman disease
Pathologically, cutaneous Rosai-Dorfman disease (cRDD) is characterised by nodular to diffuse infiltrates of polygonal to spindle-shaped histiocytes with feathery borders arranged in a storiform pattern, emperipolesis, lymphoid aggregate, and germinal centres at the periphery.2
Spindle cell xanthogranuloma variant of juvenile xanthogranuloma
Spindle cell xanthogranuloma variant of juvenile xanthogranuloma reveals well-defined nodular infiltrates of spindle cells in a storiform pattern, with Touton-like giant cells and lymphocytes.3
Sarcomatoid variant of anaplastic large cell lymphoma
Sarcomatoid type of anaplastic large cell lymphoma reveals plump spindle-shaped cells in a storiform pattern and diffuse interstitial mucinous degeneration with or without septal panniculitis.4
Superficial CD34-positive fibroblastic tumour
This is characterised by a circumscribed area of intersecting fascicles of bland spindled to pleomorphic epitheloid cells arranged in a storiform pattern, vascular ectasia, lymphoid cells, and collagenous stroma.5
Malignant peripheral nerve sheath tumours
Malignant peripheral nerve sheath tumours (MPNST) comprise of two tissue components; a majority displays dense monotonous proliferation of small- to -medium-sized angulated or round cells with hyperchromatic atypical nuclei and indistinct pale eosinophilic cytoplasm in a diffuse sheet-like fashion. The minor portion comprises of pleomorphic spindle cells with hyperchromatic, elongated wavy nuclei and eosinophilic, wispy cytoplasm arranged in a storiform pattern [Figure 4].6
![Histopathology of malignant peripheral nerve sheath tumour reveals epitheloid cell-like (red arrow) and spindled cells (black arrow) in a storiform pattern embedded in a mucinous stroma [Haematoxylin and eosin, 100x].](/content/126/2024/0/1/img/IJDVL_791_2024-g8.png)
- Histopathology of malignant peripheral nerve sheath tumour reveals epitheloid cell-like (red arrow) and spindled cells (black arrow) in a storiform pattern embedded in a mucinous stroma [Haematoxylin and eosin, 100x].
Erythema elevatum diutenum
Early erythema elevatum diutenum (EED) shows leukocytoclastic vasculitis features while late cases show perivascular onion skinning pattern of fibrosis, storiform fibrosis with clefting between collagen bundles, xanthomatisation with mixed inflammatory infiltrates composed of neutrophils, plasma cells, eosinophils and lymphohistiocytes.7
Granuloma faciale
Histopathology reveals grenz zone, eosinophilic vasculitis, and diffuse mixed inflammatory infiltrate composed of neutrophils, eosinophils, plasma cells, and lymphohistiocytes. Similar to EED, storiform fibrosis is described due to perivascular fibrosis with clefting.8
Fibrohistiocytic lipoma
Histopathology shows a well-circumscribed lipoma along with spindle cell features similar to DFSP, where an evenly distributed honeycomb or solid mass-like proliferation of plump spindle cells is seen in a storiform pattern or fascicular patterns.9
Superficial acral fibromyxoma
Histopathology depicts a dermal non-encapsulated soft tissue tumour containing spindle-shaped fibroblasts arranged in a fascicular or storiform pattern in the myxo-collagenous stroma.10
Granular cell tumour
This tumour is composed of oval- to spindle-shaped cells, primarily grouped in short fascicles or displaying a storiform pattern with desmoplastic stroma.11
Histoid Hansen
The classic histopathologic features here include epidermal atrophy, grenz zone, and underlying leproma composed of fusiform histiocytes organised in a storiform pattern.12
Pigmented storiform neurofibroma
Classically, neurofibroma (NF) does not have a storiform pattern, but one variant called pigmented storiform NF has been described in the literature, which shows a clear grenz zone and mid-dermis reveals spindle cells with bubblegum cytoplasm and wavy nucleus arranged in storiform pattern [Figures 5a, b and c].13

- Pigmented neurofibroma: Solitary brown dome-shaped papule.
![Histopathology of neurofibroma showing spindled tumour cells arranged in a storiform pattern. [Haematoxylin and eosin, 50x].](/content/126/2024/0/1/img/IJDVL_791_2024-g10.png)
- Histopathology of neurofibroma showing spindled tumour cells arranged in a storiform pattern. [Haematoxylin and eosin, 50x].
![Histopathology of neurofibroma reveals spindled cells with pale bubblegum cytoplasm and wavy nuclei in a storiform pattern (red arrow) and mast cells (black arrow) [Haematoxylin and eosin, 100x].](/content/126/2024/0/1/img/IJDVL_791_2024-g11.png)
- Histopathology of neurofibroma reveals spindled cells with pale bubblegum cytoplasm and wavy nuclei in a storiform pattern (red arrow) and mast cells (black arrow) [Haematoxylin and eosin, 100x].
Neurothekeoma
This presents as multiple nodules in the deep dermis and subcutis composed of a storiform arrangement of spindled and epithelioid mononuclear cells, variable nuclear atypia with myxoid stroma.14
Nodular fasciitis
Histopathology shows variable cellularity composed of spindled, star-shaped to plump fibroblasts that are arranged focally as vague storiform patterns or in a haphazard array (‘tissue culture appearance’), where mitotic figures, myxoid stroma, capillary proliferation and extravasated red blood cells with cleft-like spaces are seen.15
Perineurioma (storiform perineurial fibroma)
Histopathology reveals non-encapsulated, well-circumscribed spindle cells with elongated bipolar cytoplasmic processes and inconspicuous fusiform nuclei with pale eosinophilic cytoplasm in a storiform pattern.16
Progressive nodular histiocytosis
Histopathology of progressive nodular histiocytosis (PNH) shows an atrophic epidermis; the dermis shows spindle cells arranged in classical storiform pattern along with abundant histiocytes with large nuclei foamy cytoplasm along with hemosiderin-laden macrophages and Touton giant cells.17
Spitz naevus
Histopathology shows symmetrical, sharply demarcated, dome-shaped, regularly spaced nests of naevus cells. Limited pagetoid spread in the lower epidermis, junctional clefting, and coalescent eosinophilic globules known as Kamino bodies are seen. Naevus cells are epithelioid to spindle-shaped and arranged in a storiform pattern occasionally along with zonation.18
Storiform collagenoma
Histopathology demonstrates a circumscribed, hypocellular area of abundant collagen with plywood-like clefts between the collagen and fibroblasts revealing spindle-shaped nuclei in a storiform pattern [Figures 6a and b].19

- Storiform collagenoma: Solitary brown pedunculated hard nodule on the scalp.
![Histopathology of storiform collagenoma depicts the hypocellular area of abundant collagen in a storiform pattern [Haematoxylin and eosin, 100x].](/content/126/2024/0/1/img/IJDVL_791_2024-g13.png)
- Histopathology of storiform collagenoma depicts the hypocellular area of abundant collagen in a storiform pattern [Haematoxylin and eosin, 100x].
Keloid
On the histopathology of the keloid, the epidermis shows acanthosis, and loss of distinction between papillary and reticular dermis is noted. The abundance of eosinophilic collagen tissue is arranged in a whorled, storiform, or haphazard fashion, along with dense mucin deposits, fibroblast proliferation, and mast cells.20
Immunoglobulin G4 (IgG4)-related disease
This is characterised by lymphoplasmacytic infiltration, obliterative lymphocytic venulitis, and fibrosis in a storiform manner. Lymphoplasmacytic infiltration is characterised by lymphoid follicles with the germinal centre and dense plasma cell infiltration.21
Other rare conditions where the storiform pattern is described include solitary fibrous tumour, myofibroma, pseudomyogenic hemangioendothelioma, cutaneous histiocytic sarcoma, mycobacterial spindle cell tumour, angiomyofibrobastoma, cutaneous B-cell lymphoma with a storiform stromal reaction, synovial sarcoma, melanoma, neurofibrosarcoma, and gingival fibroma.
Overall, the storiform pattern is seen in neoplasms of spindle cell origin, such as fibroblast, fibrohistiocytic, neural, melanocytic, and smooth muscle origin, and also from disorders that show fibrosis. A summary of clinical presentation, immunohistochemistry (IHC), and special stains in dermatosis revealing a storiform pattern is represented in Tables 1 and 2.
| Conditions showing a storiform pattern | Type | Clinical presentation |
|---|---|---|
| Dermatofibroma | Benign fibro histiocytic tumour | Solitary skin-coloured firm papule over extremities with a characteristic dimple sign |
| Dermatofibrosarcoma protuberans | Locally aggressive malignant neoplasm of fibroblastic differentiation | Keloid-like protuberant plaque over the trunk and extremities |
| Cutaneous Rosai-Dorfman disease | Non-Langerhans histiocytic disease | Presents as papules and nodules in the head and neck region with cervical lymphadenopathy |
| Spindle cell xanthogranuloma variant of juvenile xanthogranuloma | Non-Langerhans cell histiocytosis | Solitary, well-circumscribed skin-coloured dark red nodule |
| Sarcomatoid variant of anaplastic large cell lymphoma | Anaplastic large cell lymphoma |
Generalised lymphadenopathy with extranodal involvement of skin, bone, bone marrow, liver, lungs and gastrointestinal tract Cutaneous lesions present as solitary or multiple skin-coloured papules and nodules |
| Angiomyofibroblastoma | Benign soft tissue tumour with unclear origin | Presents as a slow-growing asymptomatic nodule |
| Superficial CD34-positive fibroblastic tumour | Low-grade spindle cell neoplasm | Slow-growing asymptomatic subcutaneous mass |
| Malignant peripheral nerve sheath tumour | Soft tissue (neural) tumour | Presents as a soft tissue mass with pain and numbness along the nerve distribution |
| Erythema elevatum diutenum | Chronic fibrosing vasculitis | Presents as red-brown papules and plaques over the extensor aspect |
| Granuloma faciale | Chronic fibrosing eosinophilic vasculitis | Clinically presents as red-brown papules and nodules over the face with follicular prominence |
| Fibrohistiocytic lipoma | Tumour of fat origin | Presents as a soft mobile mass over the extremities |
| Superficial acral fibromyxoma | Fibrous tumour | Presents as a solitary papule over the periungual regions of hands and feet |
| Granular cell tumour | Neuroectodermal tumour | Presents as a solitary painless nodule over mucosa and skin |
| Cutaneous histiocytic sarcoma | Mature histiocytic malignant neoplasm | Presents as a localised solitary nodule or can have disseminated involvement of lymph nodes and gastrointestinal tract with constitutional symptoms |
| Histoid Hansen | Variant of leprosy | Multiple shiny skin-coloured, dome-shaped papules and nodules with a predilection to the extensor aspect |
| Pigmented storiform neurofibroma | Variant of neruofibroma | Solitary or rarely multiple skin-coloured to hyperpigmented soft papules at any site |
| Neurothekeoma | Nerve sheath tumour | Solitary skin-coloured, brown, well-circumscribed, asymptomatic to slightly painful papule or nodule |
| Nodular fasciitis | Benign self-limiting tumour of fibroblastic or myofibroblastic origin | Solitary superficially placed rapidly growing nodule |
| Perineuroma | Soft tissue neoplasm composed of perineural tissue | Solitary papule over extremities, which may be asymptomatic to weakness or numbness along the nerve distribution |
| Progressive nodular histiocytosis | Non-Langerhans cell histiocytosis | Discrete yellow-brown superficial papules and deep nodules |
| Pseudomyogenic (epithelioid sarcoma-like) hemangioendothelioma | Low-grade vascular tumour of endothelial origin | Indolent to painful ulcerative nodules |
| Spitz naevus | Benign tumour of epithelioid to spindle-shaped melanocytic cells | Presents as dome-shaped, skin-coloured to hyperpigmented papules, either solitary or eruption of multiple lesions over extremities |
| Storiform collagenoma. | Tumour of fibroblast origin | Solitary firm papule, mostly described in Cowden syndrome |
| Mycobacterial spindle cell pseudotumour | Tumour-like spindle cell proliferation engorged with mycobacterial species | Asymptomatic solitary mass |
| Myofibroma | Benign tumour of fibroblastic origin arising from soft tissue and bone | Pink to purplish soft nodule |
| Solitary fibrous tumour | Benign mesenchymal tumour | Clinically shows soft, painless, slowly progressive mass over the axilla, pelvis and thigh |
| Keloid | Asymptomatic to itchy, painful, firm, solitary or multiple plaques with crab-like extensions at the periphery of plaque at any sites, mostly described in ear lobule, presternal and joint areas | |
| IgG4-related disease | Itchy solitary or multiple erythematous papules, plaque and subcutaneous nodules over head and neck areas, but can involve any region and system |
IgG4: Immunoglobulin G4 related disease.
| Diseases | Pathological clue | Immunohistochemistry positivity | Immunohistochemistry negativity | Special stains |
|---|---|---|---|---|
| Dermatofibroma |
Circumscribed Grenz zone Collagen trapping Epithelial, follicular and sebaceous induction Hemosiderin |
Factor XIIIa, CD68 and CD163 | CD34 | Masson trichrome stain highlights fibrous tissue as blue |
| Dermatofibrosarcoma protuberans |
Infiltration and expansion of fibrous septa. Interdigitation of fat lobules in a honeycomb pattern Sparing of adnexal structures Herringbone pattern and significant atypia and mitotic figures in sarcomatous variant |
CD34 | Factor XIIIA, S 100, Melan A and SMA |
Pigmented DFSP stains for fontanna masson stain but not Prussian blue Myxoid DFSP stains with alcian blue, colloidal iron |
| Rosai-Dorfman disease | Emperipolesis | S100 and CD68 | CD1a | - |
| Spindle cell xanthogranulom is a variant of juvenile xanthogranuloma | Touton giant cells with vacuolated histiocytes | Factor XIIIa, Mac 387, lysozyme, CD 68 and vimentin | S100 protein, actin, desmin and keratin AE1.3 | Sudan III stain highlights intracytoplasmic fat granules |
| Sarcomatoid is a variant of anaplastic large cell lymphoma | Large, bizarre-looking, spindle-shaped cells | CD4, CD5, CD30, TIA-1 and ALK while CD3+/‒ | CD8, CD15, CD20, CD56, CD68, desmin and SMA | - |
| Angiomyofibroblastoma | Alternating areas of hypercellular and hypocellular region | Desmin, estrogen receptor, progesterone receptor and SMA | Masson trichrome stain smooth muscle cytoplasm as red and collagenous fibrous tissue as blue | |
| Superficial CD34-positive fibroblastic tumour |
Neoplastic cells with polymorphic nuclei Granular cytoplasm Intranuclear cytoplasmic pseudoinclusions Extremely low mitotic rate |
CD34 and focal positivity for keratin (AE1/AE3) | S-100 protein, EMA, SMA, myosin, desmin, myogenin, CD56 and FLI-1 | Masson trichrome stain for fibrous tissue, which highlights as blue |
| Malignant peripheral nerve sheath tumour | Elongated wavy nuclei and bubblegum or wispy cytoplasm with mitotic activity | CD34 and S100 | Silver impregnation (Bodian and Beilschowsky stain) highlights nerve cells | |
| Erythema elevatum diutenum | Leukocytoclastic vasculitis with onion ring fibrosis | - | EMA, CD34 and S100 | |
| Fibrohistiocytic lipoma | Honeycomb fat cells with spindle cells | Vimentin, calponin and CD34 | Sudan III stain highlights fat tissue | |
| Superficial acral fibromyxoma |
Prominent microvasculature Mast cells Multinucleated stromal cells |
EMA, CD34 and CD99 | Alcian blue and colloidal iron highlights mucin | |
| Granular cell tumour | Pustulo-ovoid bodies of Milian | S-100, CD31, CD56, CD68, CD117, inhibin, p53, calretinin, EMA and MIB-1 |
Periodic acid Schiff highlights granules and are resistant to diastase These granules also stain with Sudan black B Trichrome stain shows magenta colouration |
|
| Cutaneous histiocytic sarcoma | Signet-ring cell type tumour cells with areas of cellular cannibalism and emperipolesis | CD68, CD163 and lysozyme | S100 and CD1a | - |
| Neurofibroma | Elongated wavy nuclei and bubblegum or wispy cytoplasm | S100 | Glial fibrillary acidic protein | Silver impregnation (Bodian and Beilschowsky stain) highlights nerve cells |
| Neurothekeoma | Intranuclear pseudo inclusion | Strong positivity of S100A, MiTF, EMA, NSE, NKI/C3 and PGP 9.5 and focal positivity for claudin-1, Glut-1 and CD34 | Silver impregnation (Bodian and Beilschowsky stain) highlights nerve cells | |
| Nodular fasciitis | Tissue culture appearance | SMA, calponin, vimentin, KP-1 and HSP47 | Desmin, CD34, S100 and cytokeratin |
Masson trichrome stain smooth muscle cytoplasm as red and collagenous fibrous tissue as blue Alcian and colloidal iron stain for mucin |
| Perineuroma | Lamellar-like structures | CD34, EMA, vimentin, S-100 protein, desmoplakin and neurofilament | - | |
| Hybrid schwannoma and perineuroma | Well-circumscribed unencapsulated tumours | Alternating S100, EMA stain with no co-expression; Claudin 1, GFAP and CD34 | Silver impregnation (Bodian and Beilschowsky stain) highlights nerve cells | |
| Progressive nodular histiocytosis | Spindle-shaped, vacuolated, stellate, oncocytic (ground glass) and foamy cells | CD68, CD163, vimentin and fascin | S 100 and CD1a | - |
| Pseudomyogenic (epithelioid sarcoma-like) hemangioendothelioma | Cells with a rhabdomyoblast-like morphology may be seen | ERG with retained INI-1, pancytokeratin AE1/AE3 and CD31 | S100, CD34, desmin, EMA, MNF116, SMA, caldesmon, myogenin, MyoD1, HHV-8 and CD163 | |
| Spitz Naevus | Kamino bodies, zonation and absent pagetoid spread | S100, Melan A, HMB45, SOX 10, ALK, NTRK and ROS | SMA, EMA, BRAF and cytokeratin |
Masson’s fontana stain shows mild positivity in naevus cells Schmorl method stains melanin blue green |
| Storiform collagenoma | Hypocellular area of abundant collagen with ‘plywood-like’ clefts | CD34 | Masson trichrome stain to highlight collagenous fibrous tissue as blue and nuclei as black | |
| Myofibroma |
Biphasic pattern Spindle cells with eosinophilic cytoplasm and elongated nuclei Hemangiopericytoma like vascular pattern |
SMA, MSA, vimentin and calponin | P63, desmin and h-caldesmon | Masson trichrome stain smooth muscle cytoplasm as red and collagenous fibrous tissue as blue |
| Solitary fibrous tumour | Spindle-to-ovoid collagen with inconspicuous cytoplasm | CD 34, STAT 6 and vimentin | CD 99, CD 31, S100, AML, desmin and SOX 10 | - |
| IgG4-related disease | Lymphoid aggregates, plenty of plasma cells and fibroblast in storiform pattern | CD 138 and IgG4 | Elastin Van Gieson stain to highlight obliterative venulitis |
SMA: Smooth muscle actin, EMA: Epithelial membrane antigen, CD: Cluster of differentiation, SOX: SRY related HMG box 10, NTRK: Neurotrophic tropomyosin-receptor kinase, ROS: Repressor of Silencing, HMB 45: Human Melanoma Black 45, HSP: Heat shock protein, MSA: Muscle-specific actin, GFAP: Glial fibrillary acidic protein, MNF: Cytokeratin pan monoclonal antibody, HHV: Human herpes virus, ERG: Erythroblast transformation specific related gene, PGP: Pglycoprotein, HSP: Heat shock protein, ALK: Anaplastic lymphoma kinase, TIA: T cell intracellular antigen 1, AE: Anionic exchange, STAT: Signal transducer and activator of transcription, AML: acute myeloid leukemia, BRAF: V raf murine sarcoma viral oncogene homolog B, DFSP: Dermatofibrosarcoma protuberans, NKI/C3 doesnot have expansion.
To conclude, a storiform pattern can be associated with the histopathology of various cutaneous spindle and non-spindle cell tumours. This article enlists all the entities associated with a storiform pattern. Besides, we provide an overview of pathological characteristics, cellular morphology, and IHC that helps delineate various dermatoses demonstrating storiform patterns.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Clinical and histological patterns of dermatofibroma without gross skin surface change: A comparative study with conventional dermatofibroma. Indian J Dermatol Venereol Leprol. 2015;81:263-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous Rosai-Dorfman disease: Histopathological presentation as inflammatory pseudotumor. A literature review. Acta Derm Venereol. 2002;82:292-6.
- [CrossRef] [PubMed] [Google Scholar]
- Solitary spindle-cell xanthogranuloma of the eyelid. Ophthalmology. 2002;109:258-61.
- [CrossRef] [PubMed] [Google Scholar]
- Sarcomatoid variant of primary cutaneous anaplastic large cell lymphoma. Am J Dermatopathol. 2019;41:e164-7.
- [CrossRef] [PubMed] [Google Scholar]
- Superficial CD34-positive fibroblastic tumor: Report of two cases and review of literature. Int J Clin Exp Pathol. 2020;13:38-43.
- [PubMed] [PubMed Central] [Google Scholar]
- Malignant peripheral nerve sheath tumor of small round cell type with pleomorphic spindle cell sarcomatous areas. Pathol Int. 2003;53:478-82.
- [CrossRef] [PubMed] [Google Scholar]
- The late stage of erythema elevatum diutinum mimicking cutaneous spindle-cell neoplasms: A case report and review of the literature. J Cutan Pathol. 2019;46:551-4.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic localized fibrosing leukocytoclastic vasculitis associated with lymphedema, intralymphatic and intravascular lymphocytosis, and chronic myelogenous leukemia: A case report of unilateral erythema elevatum diutinum. Am J Dermatopathol. 2017;39:479-84.
- [CrossRef] [PubMed] [Google Scholar]
- Fibrohistiocytic lipoma: Twelve cases of a previously undescribed benign fatty tumor. Ann Diagn Pathol. 2000;4:354-60.
- [CrossRef] [PubMed] [Google Scholar]
- Superficial acral fibromyxoma. Int J Dermatol. 2015;54:499-508.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatofibroma-like granular cell tumour: A potential diagnostic pitfall. Pol J Pathol. 2016;67:291-94.
- [CrossRef] [PubMed] [Google Scholar]
- Histoid hansen’s with transepidermal elimination: Five cases. Int J Mycobacteriol. 2022;11:217-21.
- [CrossRef] [PubMed] [Google Scholar]
- A benign cutaneous plexiform hybrid tumor of perineurioma and cellular neurothekeoma. Am J Surg Pathol. 2013;37:845-52.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous nodular fasciitis with rare TPM4-USP6 fusion. J Cutan Pathol. 2022;49:196-9.
- [CrossRef] [PubMed] [Google Scholar]
- Perineurioma (storiform perineurial fibroma): Clinico-pathological analysis of four cases. Histopathology. 1994;25:261-7.
- [CrossRef] [PubMed] [Google Scholar]
- Progressive nodular histiocytosis: An unusual disorder. Dermatol Online J. 2021;27:13030/qt4t37r77d.
- [CrossRef] [PubMed] [Google Scholar]
- Spitz nevus, Spitz tumor, and spitzoid melanoma: A comprehensive clinicopathologic overview. Dermatol Clin. 2013;31:589-98, viii.
- [CrossRef] [PubMed] [Google Scholar]
- Storiform collagenoma (sclerotic fibroma) of the oral mucosa. Br J Oral Maxillofac Surg. 2020;58:231-3.
- [CrossRef] [PubMed] [Google Scholar]
- Functional histopathology of keloid disease. Histol Histopathol. 2015;30:1033-5.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25:1181-92.
- [CrossRef] [PubMed] [Google Scholar]





