Translate this page into:
Subcutaneous cystic swelling in a leprosy patient
2 Department of Pathology, Schieffelin Leprosy Research & Training Centre, Karigiri, Vellore, India
Correspondence Address:
Bikash Ranjan Kar
Department of Dermatology, SLR & TC, Karigiri, Vellore-632 106
India
| How to cite this article: Kar BR, Ebenezer G, Job C K. Subcutaneous cystic swelling in a leprosy patient. Indian J Dermatol Venereol Leprol 2005;71:305-306 |
 |
 |
 |
 |
 |
 |
A 45-year-old male attended the hospital with complaints of a subcutaneous swelling over the dorsum of the right hand since 6 months. He had been diagnosed as a case of lepromatous leprosy 4 years earlier and treated with the WHO multibacillary multidrug regimen for 24 months. After 6 months of starting MDT, the patient started getting recurrent erythema nodosum leprosum for which he received systemic prednisolone off and on. He developed the subcutaneous swelling while on oral corticosteroid treatment (Total cumulative dose of 12600 mg in last 2 years with maximum dose of 40 mg per day) for control of type II lepra reaction. There was no history of trauma preceding the onset of the lesion.
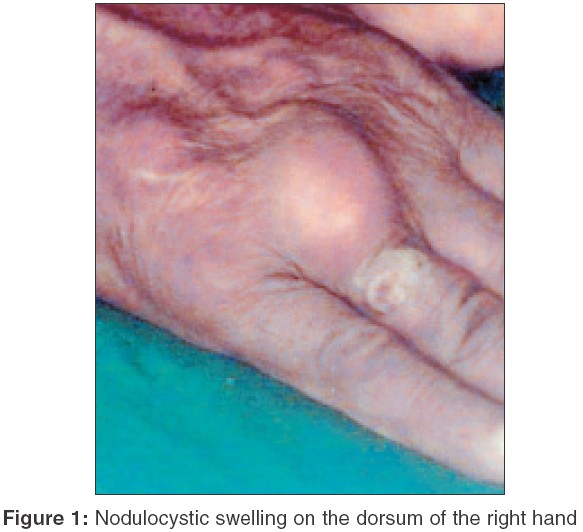
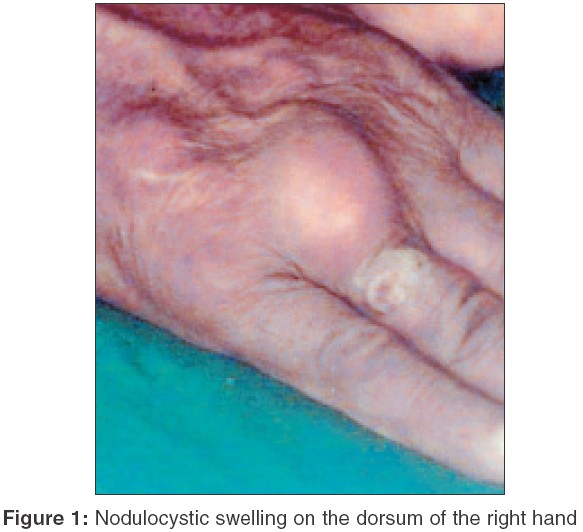
On examination, a single, well-defined, irregular swelling was found over the dorsal aspect of the right hand overlying the base of the right ring finger [Figure - 1]. It measured approximately 3 cm x 3 cm in size. The overlying skin was slightly erythematosus. An ulcerated lesion was present towards the distal end of the swelling . On palpation, the lesion was found to be a soft, slightly fluctuant, subcutaneous cyst, freely mobile in all directions, without any adherence to the underlying structures. The skin over the cyst was slightly warmer than the surrounding skin. There was no regional lymphadenopathy. Hemogram, urine routine and microscopy and chest X-ray revealed no abnormalities. Thick pus, which showed plenty of neutrophils without any bacteria, was aspirated from the cyst. Photomicrographs of H/E and PAS stained sections are shown in [Figure - 2] and [Figure - 3].
What is your diagnosis?
Diagnosis: Subcutaneous phaeohyphomycosis
Discussion
Histopathology revealed a cystic cavity containing necrotic material. The wall was composed of dense fibrous tissue, epithelioid cells, numerous Langhans and foreign body giant cells and lymphocytes [Figure - 2]. Numerous fungal hyphae were present in the inflammatory infiltrate. They were broad, haphazardly branched and the walls varied in shape and thickness. Periodic acid Schiff (PAS) stain clearly demonstrated the presence of fungal hyphae [Figure - 3]. Culture for fungus showed growth of Exophiala jeanselmei .
The term "phaeohyphomycosis" was coined in 1974 to describe infections with dematiaceous, septate mycelial elements in the tissue.[1] Though subcutaneous phaeohyphomycosis is more common in the tropics and in immunosuppressed patients on prolonged steroid therapy[2], it may also occur in immunocompetent persons.[3] Phaeohyphomycosis is a rare, and usually localized, subcutaneous or intramuscular infection, typically a cyst or abscess, caused by any one of over a 100 species[4] of dematiaceous fungi. Common causes are Exophiala jeanselmei , Exophiala dermatitidis and Bipolaris. Recently, Girard et al[5] reported a case of subcutaneous phaeohyphomycosis caused by Pyrenochaeta romeroi in a leprosy patient.
The pathogen is probably by implantated from an exogenous source. Infection begins with a firm, sometimes tender nodule, which may develop into a large cyst up to several centimeters in size. Histopathology with the help of special fungal stains like PAS and Grocott′s stains will help confirm the diagnosis. It is important to exclude other cystic structures such as Baker′s cysts. The fungi can be seen in the granulomatous lining of the cyst wall. The organisms are not usually difficult to grow from the lesion, but identification of the subspecies sometimes requires help from a specialist. The usual treatment is surgical excision. Itraconazole is often recommended after surgery to reduce the chances of recurrence, particularly in immunosuppressed patients.[6]
| 1. |
Chandler FW, Ajello L, Kaplan W. Color atlas and text book of the histopathology of mycotic diseases. London: Wolfe; 1980. p. 92-8.
[Google Scholar]
|
| 2. |
Fathizadeh A, Rippon JW, Rosenfeld SI, Fretzin DF, Lorincz DL. Phaeohypomycotic cyst in an immunosuppressed host. J Am Acad Dermatol 1981;5:423-7.
[Google Scholar]
|
| 3. |
Patterson JW, Warren NG, Kelly LW. Cutaneous phaeohyphomycosis due to Cladophialophora bantiana . J Am Acad Dermatol 1999;40:364-6
[Google Scholar]
|
| 4. |
Rinaldi MR. Phaeohyphomycosis. Dermatol Clin 1996;14:147-53.
[Google Scholar]
|
| 5. |
Girard C, Dereure O, Rispail P, Durand L, Guilhou JJ. Subcutaneous phaeohyphomycosis due to Pyrenochaeta romeroi in a patient with leprosy. Acta Derm Venereol 2004;84:154-5.
[Google Scholar]
|
| 6. |
Hay RJ, Moore M. Mycology. In : Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Textbook of dermatology. 6th edn. London: Blackwell Scientific; 1998. p. 1277-1376.
[Google Scholar]
|
Fulltext Views
2,498
PDF downloads
3,203





