Subcutaneous dirofilariasis in a Tunisian patient
Corresponding author: Dr. Safa Idoudi, Department of Dermatology, Fattouma Bourguiba University Hospital, Farhat Hached Street, Monastir 5000, Tunisia. safaa.idoudi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Idoudi S, Youssef M, Soua Y, Achour A, Babba H, Zili J. Subcutaneous dirofilariasis in a Tunisia patient. Indian J Dermatol Venereol Leprol 2021;87:390-2
Sir,
Human subcutaneous dirofilariasis is a rare helminthic infection caused by filarial worms of the genus Dirofilaria species, common in the southern USA. Its diagnosis is always challenging, especially in nonendemic regions, where most cases are diagnosed retrospectively.
A 19-year-old girl, a dog owner from East Central Tunisia, presented with two-month history of asymptomatic swelling of the lumbar area. There was no history of trauma, insect bite or foreign body. Examination revealed a single, soft, mobile, skin-colored subcutaneous nodule of 1 cm large size in the right lumbar region, simulating lipoma. She had no other skin or systemic abnormalities. Hematological findings were within normal range, with no evidence of eosinophilia or hepatocellular dysfunction. An ultrasound scan showed a well-defined complex cystic structure containing an echogenic continuously moving structure, highly suggestive of a living worm [Figure 1]. By local excision under anesthesia, the encapsulated nodule was removed [Figure 2]. A thin, cylindrical, white worm, about 20 mm in length was found embedded in the subcutaneous fatty tissue. Parasitological examination identified a thick laminated cuticle with prominent longitudinal ridges, fitting with a filarial worm of the species Dirofilaria repens [Figure 3]. After the surgery, the patient did not present any clinical evidence of recurrence within a follow-up period of three years.
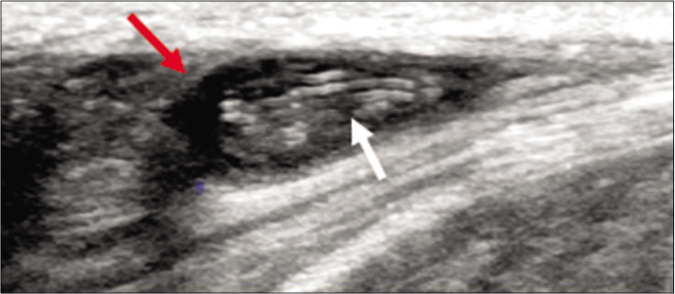
- A well-defined complex cystic structure (red arrow) containing an echogenic moving structure highly suggestive of a living worm (white arrow)
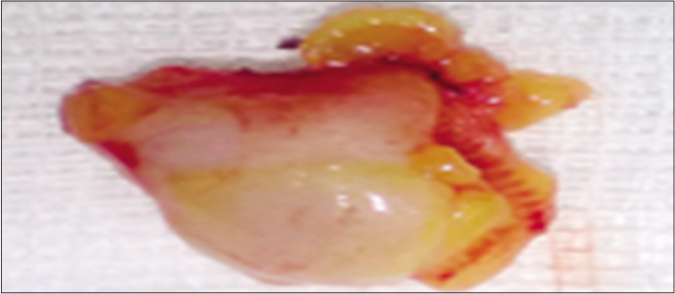
- Excision of the worm with adjacent subcutaneous fat
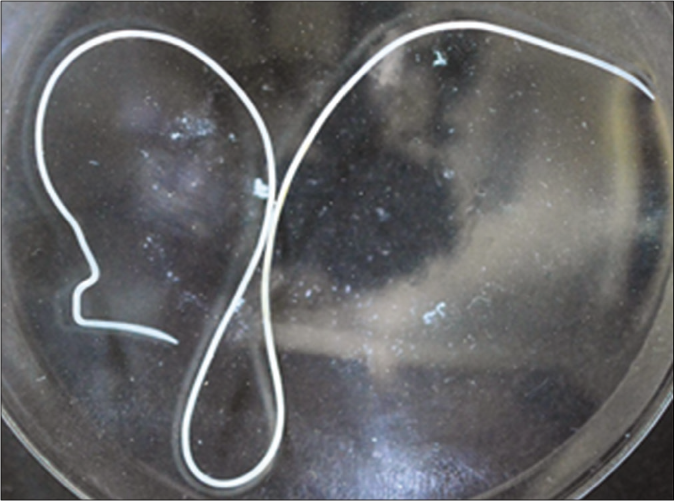
- Thin, cylindrical, white worm at about 20 mm in length highly suggestive of Dirofilaria repens
Dirofilariasis is a zoonotic infection that accidentally affects humans. This emerging helminthic disease is caused by filarial nematodes of the genus Dirofilaria, which are transmitted by female mosquitoes of the Culicidae family, including Aedes, Culex and Anopheles1. Two species of filarial nematodes are the cause of human dirofilariasis: D. repens and D. immitis. The latter is particularly endemic in tropical regions and responsible for pulmonary dirofilariasis, whereas D. repens causes subcutaneous nodules in Africa, Europe and Asia. We found only 16 previous reports of dirofilariasis to D. repens in Tunisia since 1990. Of these, six cases presented with subcutaneous nodules; four had conjunctival involvement in the form of orbital cellulite-like lesion and conjunctival cyst); three presented in the form of breast lumps; two in the form of abscess-like nodule in the scrotum; and one had lesion in the labial area, resembling a sebaceous cyst-like tumor.2
Worldwide, 300 cases of visceral dirofilariasis and over 800 cases of cutaneous dirofilariasis are reported in literature. In the Mediterranean countries, particularly, asymptomatic infection in the dogs and the warm climate could explain the continuous spread of the disease.3 Clinically, cutaneous dirofilariasis caused by D. repens commonly appears as a solitary, erythematous, slowly growing subcutaneous nodule, localized to the exposed areas of the body. Its common differential diagnoses, include insect bites, infections, post inflammatory granuloma, sarcoidosis, and immune system mediated disorders.4 The peculiarity of this case is due to the localization of the lesion in the covered area and its presentation with no inflammatory reaction.
Diagnosis is based on the isolation of the worm in the cutaneous lesion. Further investigations including biological test are unnecessary, as peripheral blood eosinophilia is commonly missed. If found, it suggests circulation of the filaria in the blood, which is mainly observed in case of preexistent malignant neoplasia or immunodeficiency.5 Diagnosis could be confirmed by imaging, like high-resolution ultrasonography, which is considered as the imaging modality of choice to visualize the worm in vivo. Magnetic resonance imaging, though expensive, is more efficient in diagnosing the condition compared to ultrasonography.6 The serological diagnosis of species Dirofilaria repens and Dirofilaria immitis is currently possible, but remains nonspecific in practice. In our case, parasitological study of the isolated worm identified the species. Morphologically, cuticular ridges in D. repens are spaced at twice the height of each ridge, while D. immitis presents a smooth cuticle.7 There is no need for further screening of hidden infection because of its indolent nature. Surgical removal of the nodule or the worm presents the treatment of choice with no need to use anthelmintic treatment.
In conclusion, dirofilariasis is considered an emerging zoonotic disease mainly in the Mediterranean region and the eastern parts of the European continent. We do believe that it is not considered a threat to the public health system. We present this case to increase awareness about its cutaneous localization and suggest an approach for its diagnosis and its management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Human dirofilariosis of buccal mucosa First molecularly confirmed case and literature review. Parasitol Int. 2019;73:101960.
- [CrossRef] [PubMed] [Google Scholar]
- Dirofilariasis of the breast: Two new cases in Tunisia. Med Sante Trop. 2015;25:327-30.
- [CrossRef] [PubMed] [Google Scholar]
- Dirofilarial infections in Europe. Vector Borne Zoonotic Dis. 2011;11:1307-17.
- [CrossRef] [PubMed] [Google Scholar]
- Human subcutaneous dirofilariasis due to Dirofilaria (Nochtiella) repens: Clinically suspected as Cutaneous Fascioliasis. Iran J Public Health. 2010;39:105-9.
- [Google Scholar]
- Dirofilaria repens infection as a cause of intensive peripheral microfilariemia in a polish patient: Process description and cases review. Acta Parasitol. 2018;63:657-63.
- [CrossRef] [PubMed] [Google Scholar]





