Translate this page into:
Subcutaneous phaeohyphomycosis caused by cladophialophora boppii
2 Department of Microbiology, T.N. Medical College and B.Y.L. Nair Ch. Hospital, Mumbai Central, Mumbai, India
Correspondence Address:
Chitra S Nayak
302 Arun, 6th road, Santacruz (East), Mumbai-400055
India
| How to cite this article: Pereira RR, Nayak CS, Deshpande SD, Bhatt KD, Khatu SS, Dhurat RS. Subcutaneous phaeohyphomycosis caused by cladophialophora boppii. Indian J Dermatol Venereol Leprol 2010;76:695-698 |
Abstract
Subcutaneous phaeohyphomycosis is an infection of the skin and subcutaneous tissue, caused by dematiaceous fungi. An adult male presented with a history of multiple reddish nodules over the face and hands. Histopathological examination of the skin biopsies showed a dense granulomatous infiltrate of macrophages, containing intracytoplasmic basophilic bodies throughout the dermis. Gomori methenamine-silver stained sections revealed yeast cells within macrophages. Multiple cultures on Sabouraud's dextrose agar grew Cladophialophora boppii. The patient was treated with oral itraconazole for a year and the response monitored with dermal ultrasound. This is the first case report of subcutaneous phaeohyphomycosis caused by Cl. boppii in India.Introduction
Dematiaceous fungi are characterized by their dark pigmentation derived from the melanin complex in their cellular wall. The major infection patterns, typically based on histological findings, are grouped into three broad classes: chromoblastomycosis, phaeohyphomycosis, and eumycotic mycetoma. Phaeohyphomycosis is an umbrella term for all those mycoses where the fungus is present in host tissues with melanized filaments, and represents a broad range of primary and opportunistic mycoses by Fonsecaea, Exophiala, Cladophialophora and others. [1] Subcutaneous phaeohyphomycosis involves skin and subcutaneous tissue. We present this case of subcutaneous phaeohyphomycosis due to the rarity of the etiological agent and the unusual clinical manifestation. This is the first case report of subcutaneous phaeohyphomycosis caused by Cladophialophora boppii in India. Also, another interesting aspect of this case is the use of ultrasound biomicroscopy with 50 MHz ultrasound in monitoring the treatment response which helped us to decide the duration of therapy, in the absence of established guidelines for the same.
Case Report
A 23-year-old Indian man, software engineer by occupation, with no medical history, presented with a 2-month history of slowly growing multiple asymptomatic reddish nodules which appeared simultaneously on the face and right hand. He was otherwise well. The patient denied any apparent antecedent trauma, arthropod bite, family history or contact with a person with similar lesions or foreign travel. He had not sought any treatment previously.
Physical examination revealed multiple erythematous, non-tender, firm nodules ranging in size from 0.5 to 0.8 cm on the right lower eyelid [Figure - 1]a and right hand, and a tumid plaque about 1 Χ 1 cm on the chin [Figure - 1]b. The nodule on the eyelid showed surface crusting. Regional lymph nodes were not enlarged. There was no thickening of peripheral nerves or loss of sensations. A review of systems revealed no abnormalities.
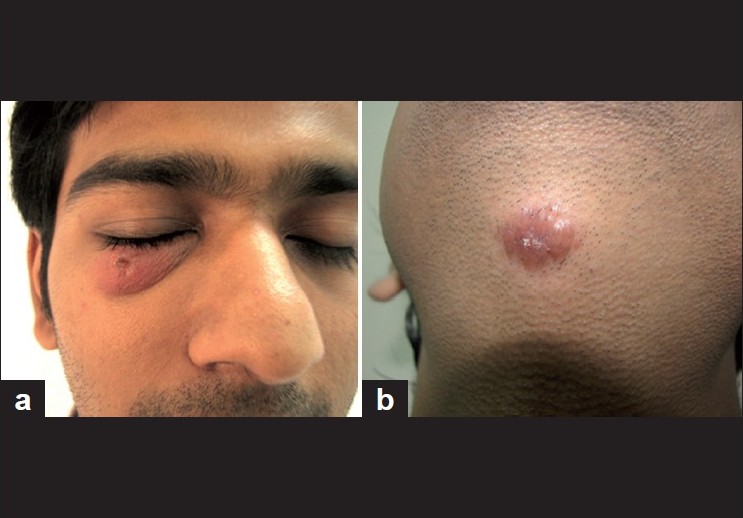 |
| Figure 1 :(a) Erythematous nodule on right lower eyelid; (b) erythematous plaque on chin |
The clinical differential diagnoses of leprosy, cutaneous leishmaniasis, deep fungal infection and sarcoidosis were considered. Results of the following laboratory studies were normal or negative: complete hemogram, blood chemistry analysis, Venereal Disease Research Laboratory (VDRL) test and Human Immunodeficiency Virus (HIV) antibody. Radiography of the chest and skull revealed no abnormality.
An excision biopsy of the hand lesion and punch biopsy from the chin lesion was obtained for histological examination and culture. Histopathological study of hematoxylin and eosin stained sections demonstrated an atrophic epidermis with a dense infiltrate throughout the dermis composed of macrophages, lymphocytes and a few plasma cells; the macrophages showed intracellular basophilic bodies. Acid-fast stained sections for bacilli were negative. Culture and imprint smears were negative for leishmania. Gomori methenamine-silver stained sections showed yeast cells within macrophages [Figure - 2]. Cultures on Sabouraud′s dextrose agar grew olivaceous-green, woolly fungal colonies which on microscopic examination revealed septate, brown hyphae and long chains of smooth-walled globose conidia suggestive of Cl. boppii [Figure - 3]. These findings were consistent with subcutaneous phaeohyphomycosis caused by Cl. boppii, a dematiaceous fungus.
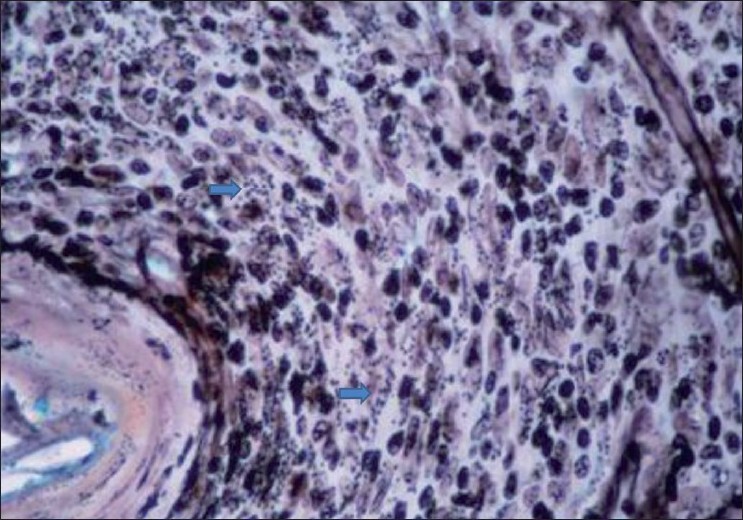 |
| Figure 2 :Yeast cells within macrophages (Gomori methenamine silver, ×40) |
 |
| Figure 3 :Cl. boppii showing unbranched, very long chains of smooth-walled globose conidia (slide culture of tissue on Sabouraud's dextrose agar) |
The patient was treated orally with itraconazole 200 mg and 30 drops of supersaturated solution of potassium iodide per day. The hand lesion did not recur following excision. At 4 months of therapy, the chin lesion was excised due to absence of clinical improvement; however, histology and cultures were negative for Cl. boppii. The potassium iodide was discontinued and oral itraconazole continued. At 9 months of therapy, there was noticeable reduction of the eyelid swelling with minimal erythema and post-inflammatory hyperpigmentation. The chin lesion did not recur following excision. However, ultrasound biomicroscopy in the region of the affected eyelid using a 50 MHz probe revealed a normal epidermal entry echo, a well-defined oval hypoechoic mass lesion (granuloma) measuring 2.5 Χ 1.5 mm in the dermis with normal underlying subcutaneous tissue [Figure - 4].
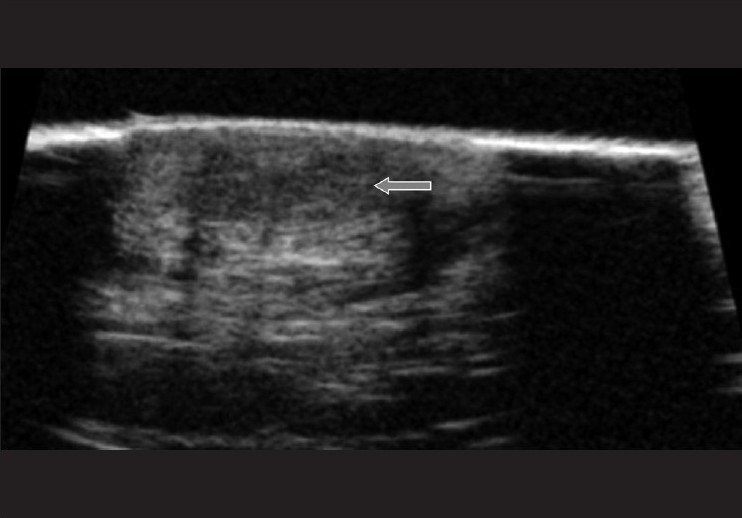 |
| Figure 4 :UBM image of lesional skin showing a hypoechoic mass (arrow) measuring 2.5 × 1.5 mm in the dermis |
Hence, therapy was continued to a total duration of 1 year at the end of which the lesion healed with post-inflammatory hyperpigmentation [Figure - 5], and a repeat ultrasound biomicroscopy showed healing of the dermal granulomas. Five months after completion of the therapy, there was no recurrence of lesions.
 |
| Figure 5 :Resolution of the lesion with post-inflammatory hyperpigmentation at 1 year of therapy |
Discussion
Dematiaceous fungi are characterized by their dark pigmentation derived from the melanin complex in their cellular wall. They are ubiquitous in nature, found mostly in soil and vegetation. Infection is probably introduced by traumatic inoculation or inhalation of the etiologic agent. Trivial unnoticed trauma may be responsible for initiating infection in this case. Chromoblastomycosis, eumycetoma and phaeohyphomycosis are the distinct clinical syndromes. [1],[2],[3],[4]
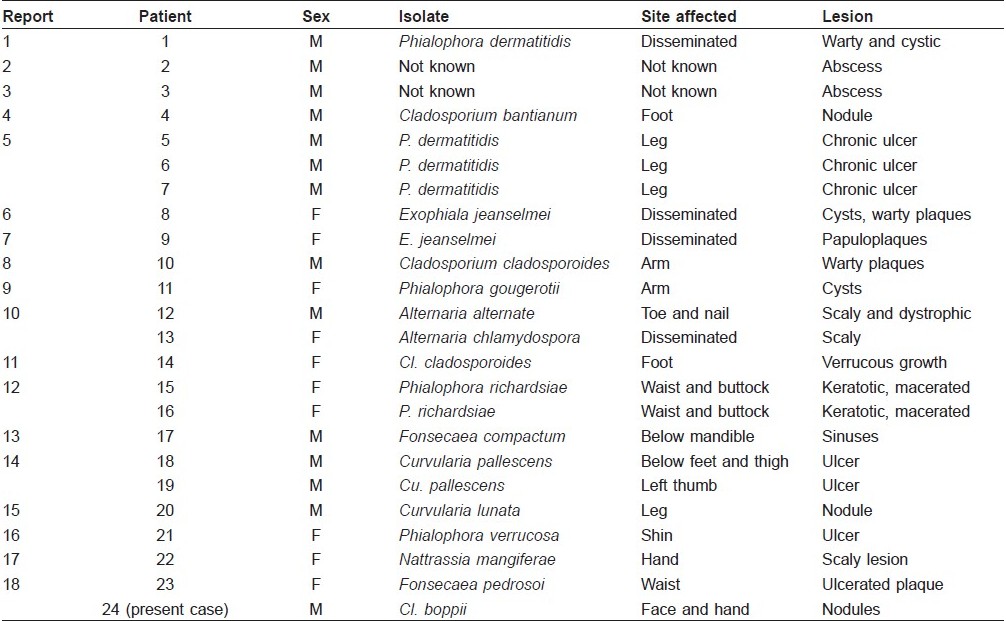
Phaeohyphomycosis is a rare infection caused by dematiaceous fungi, involving the skin and subcutis, paranasal sinuses, eyes, bones or central nervous system. Skin and subcutaneous tissue involvement is termed subcutaneous phaeohyphomycosis, and is characterized by papulonodules, verrucous, hyperkeratotic or ulcerated plaques, cysts, abscesses, pyogranuloma, non-healing ulcers or sinuses. In India, commonly associated genera are Exophiala, Phialophora, Cladosporium, Curvularia, Fonsecaea and Alternaria [Table - 1]. [1],[2]
Laboratory diagnosis includes isolation of fungal hyphae on potassium hydroxide mounts and culture on Sabouraud′s dextrose agar. [4] Histopathologically, the lesions show brown-walled septate hyphae or yeast or a combination of both in tissue. The Fontana-Masson stain (specific for melanin), periodic acid-Schiff and Gomori methenamine-silver stains can be used to confirm the diagnosis. [4],[5]
Cladophialophora spp. may cause phaeohyphomycosis, chromoblastomycosis, and mycetoma. Cl. boppii has been isolated from cases of chromoblastomycosis, phaeohyphomycosis and lung infections. Species identification is important in cases of phaeohyphomycosis as other species such as Cladophialophora bantiana are neurotropic, causing brain abscess which is frequently fatal. Cladophialophora colonies are powdery to woolly with olivaceous-green to black on the obverse and black on the reverse. Cl. boppii produces unbranched, very long chains of smooth-walled globose conidia. No shield cells are observed and the conidia directly emerge from the conidiophores. [6]
Local infection may be cured with excision or cryotherapy alone, or in combination with antifungals. [2] Dematiaceous fungi are most susceptible to itraconazole, voriconazole and posaconazole. Ketoconazole and fluconazole have limited activity. Amphotericin-B and 5-flucytosine may be used. Systemic disease is often refractory to therapy. [4],[7] The precise duration of therapy is not established, and it may range from 1 to 48 months. Hence, non-invasive techniques like ultrasound biomicroscopy can be useful in delineating the dermal lesions and monitoring response to therapy.
Ultrasound biomicroscopy (UBM) is high frequency ultrasonography performed using a 50-MHz probe (resolution of 40 ΅m and depth of penetration 4 mm). Dermatological ultrasound is usually performed using a 20-MHz probe (resolution of 80 ΅m and depth penetration 8-10 mm). However, UBM gives a much superior resolution of the dermis and epidermis, compared with lower-frequency probes. It can be used to measure skin thickness, axial and lateral extension of tumors and inflammatory processes. [8]
In our case, the duration of treatment was decided based on ultrasound findings in spite of apparent clinical resolution. As there are no conclusive guidelines regarding duration of antifungal therapy which may range widely, UBM can be a useful tool to guide duration of therapy.
| 1. |
Caligiorne RB, de Resende MA, Dias-Neto E, Oliveira SC, Azevedo V. Dematiaceous fungal pathogens: analysis of ribosomal DNA gene polymorphism by polymerase chain reaction-restriction fragment length polymorphism. Mycoses 1999;42:609-14.
[Google Scholar]
|
| 2. |
Sharma NL, Mahajan V, Sharma RC, Sharma A. Subcutaneous pheohyphomycosis in India--a case report and review. Int J Dermatol 2002;41:16-20.
[Google Scholar]
|
| 3. |
Somani VK, Razvi F, Sharma VK, Sita V, Suc. Primary cutaneous phaeohyphomycosis. Indian J Dermatol Venereol Leprol 1996;62:363-4.
[Google Scholar]
|
| 4. |
Revankar SG. Dematiaceous fungi. Mycoses 2007;50:91-101.
[Google Scholar]
|
| 5. |
Rinaldi MG. Phaeohyphomycosis. Dermatol Clin 1996;14:147-53.
[Google Scholar]
|
| 6. |
de Hoog, Kwon-Chung, McGinnis. Cladophialophora boppii. In: Sutton DA, Fothergill AW, Rinaldi MG, editors. Guide to clinically significant fungi, 1 st ed. Baltimore: Williams and Wilkins; 1998;124-7.
[Google Scholar]
|
| 7. |
Sharkey PK, Graybill JR, Rinaldi MG, Stevens DA, Tucker RM, Peterie JD, et al. Itraconazole treatment of phaeohyphomycosis. J Am Acad Dermatol 1990;23:577-86.
[Google Scholar]
|
| 8. |
Bhatt KD, Fernandes R, Dhurat R. Ultrasound biomicroscopy of the skin to detect a subclinical neuroma of the proximal nail-fold. Indian J Dermatol Venereol Leprol 2006;72:60-2.
[Google Scholar]
|
Fulltext Views
4,085
PDF downloads
1,261





