Translate this page into:
Subcutaneous Saksenaea vasiformis infection presenting as disfiguring facial plaques
2 Department of Medicine, Division of Infectious Diseases, King Chulalongkorn Memorial Hospital, Thai Red Cross Society, Bangkok, 10330; WHO-CC for Research and Training on Viral Zoonoses, Bangkok, 10330, Thailand
3 Department of Microbiology, Faculty of Medicine, Chulalongkorn University, Bangkok, 10330, Thailand
Corresponding Author:
Pawinee Rerknimitr
Department of Medicine, Division of Dermatology, Faculty of Medicine, Chulalongkorn University, Bangkok 10330
Thailand
pawineererk@yahoo.co.th
| How to cite this article: Nitinawarat J, Putcharoen O, Chindamporn A, Rerknimitr P. Subcutaneous Saksenaea vasiformis infection presenting as disfiguring facial plaques. Indian J Dermatol Venereol Leprol 2017;83:346-348 |
Sir,
A 51-year-old Thai labourer presented with painless masses on the forehead, around both eyes and nose for 2 months. Four months earlier, he had a shallow abrasion on the forehead after an accident. Some weeks later, an infiltrative mass gradually developed. Despite the treatment with antibiotics and serial wound debridement, the mass slowly enlarged. He was afebrile and had no systemic symptoms. He was otherwise healthy with no underlying disease.
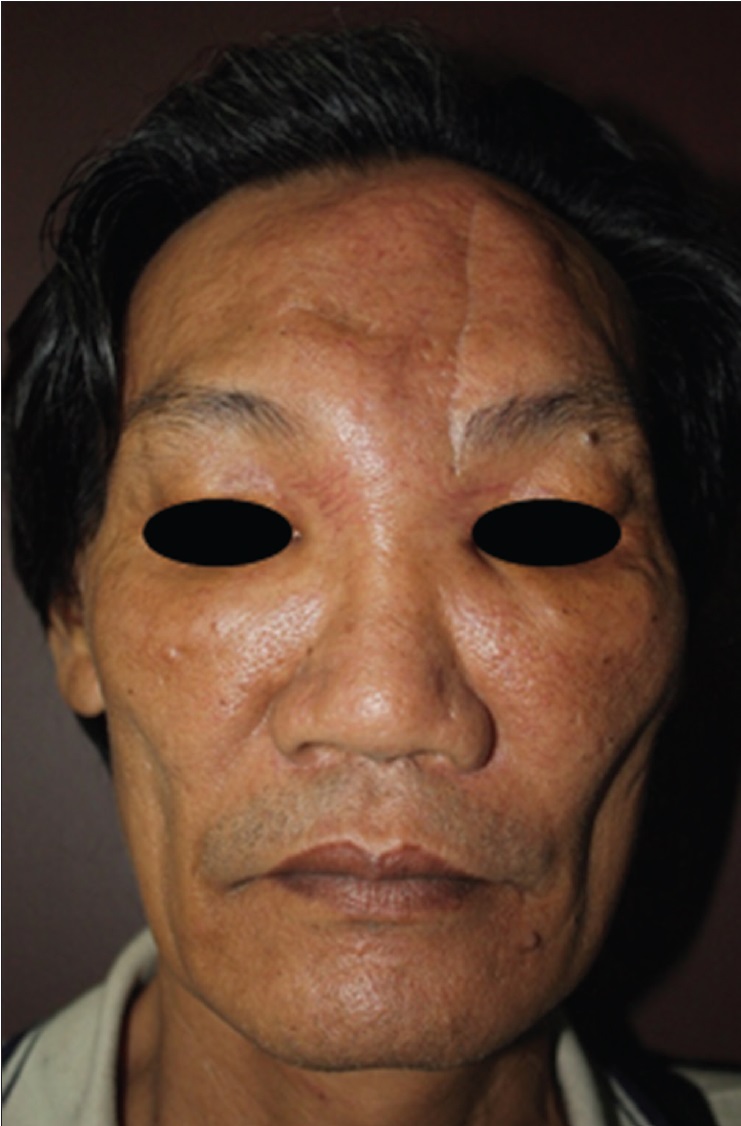
Physical examination revealed painless, firm, infiltrative plaques in centrofacial area involving the forehead, upper and lower eyelids as well as the nose [Figure 1a]. There was a limitation of bilateral upward gaze. Nasal cavity and nasopharyngeal mucosa were normal. Serology for HIV infection was negative.
 |
| Figure 1a: Diffuse erythematous infiltration with skin thickening over the forehead, both eyelids and the nose, causing facial disfigurement |
Skin biopsy specimen was taken from the forehead. Hematoxylin and eosin stain revealed diffuse granuloma formations composed of multinucleated giant cells and lymphohistiocytes in the reticular dermis and subcutaneous tissue [Figure 2a]. Periodic acid-Schiff and Gomori's methenamine silver stain revealed broad, non-septate hyphae with right angle branching [Figure 2b] and [Figure 2c].
To identify the fungus, tissue culture was carried out on Sabouraud dextrose agar and white cottony growth was revealed [Figure 2d]. Wet preparation showed broad, non-septate hyphae without sporulation. Culture with distilled water method to induce sporulation has been attempted without success. Nevertheless, molecular analysis using universal fungal primers: ITS1 (5'-TCCGTAGGTGAACCTGCGG-3') and ITS4 (5'-TCCTCCGCTTATTGATATGC-3') amplified the internal transcribed sequence region of ribosomal DNA as previously described and blasted with GenBank database showed 99.9% identity with Saksenaea vasiformis from the biopsied tissue.[1]
Treatment with amphotericin B (1.2 mg/kg/day) and itraconazole (600 mg/day) was administered for 40 days. A total dose of 2800 mg of amphotericin B was given. His facial plaque markedly improved [Figure 1b]. He was discharged with itraconazole (600 mg/day) as home medication but unfortunately was lost to follow-up.
 |
| Figure 1b: Improvement in lesions after two months of therapy |
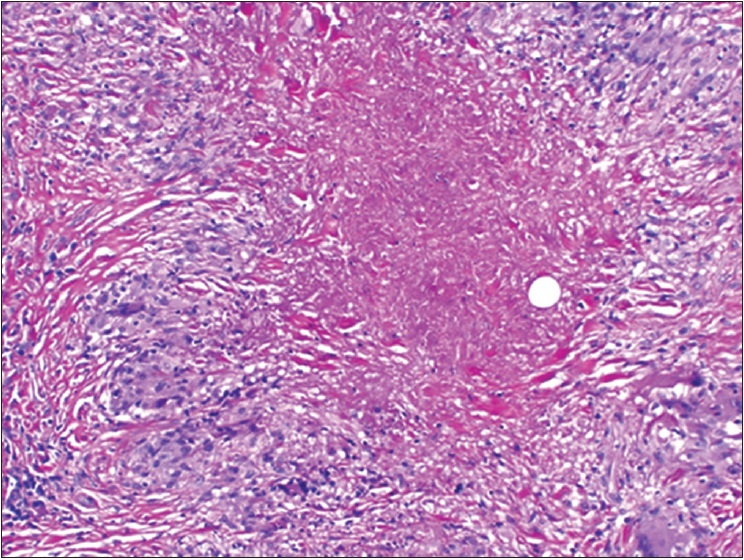 |
| Figure 2a: Diffuse granulomas in the reticular dermis and subcutaneous tissue with necrobiotic collagen (H and E, ×200) |
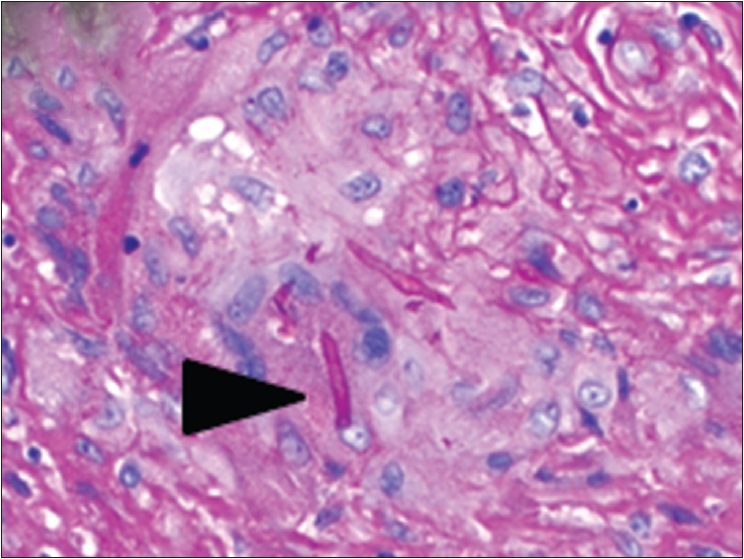 |
| Figure 2b: Broad, non-septate hyphae in multinucleated giant cells (PAS, ×200) |
 |
| Figure 2c: Broad, non-septate hyphae in multinucleated giant cells (GMS, ×200) |
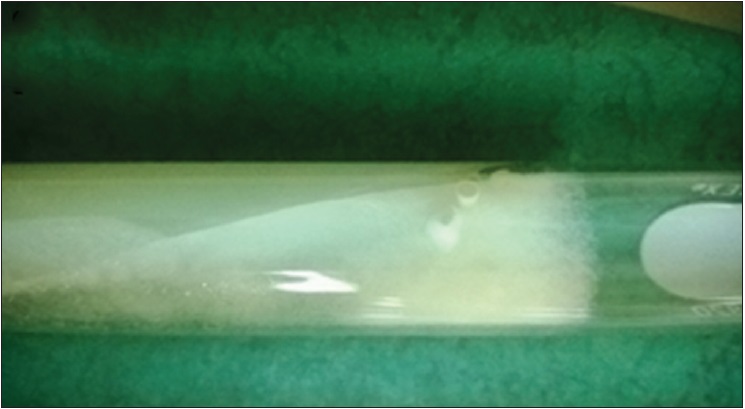 |
| Figure 2d: White cottony colony of Saksenaea vasiformis, 3 days old on SDA, incubated at 35°C |
Zygomycosis is an infection caused by fungi of class Zygomycetes. Broadly, there are two groups of fungi with medical importance in this class, Mucorales and Entomophthorales. Stereotypically both yield distinct clinical manifestations. Mucormycosis, an acute, rapidly progressive infection, caused by Mucorales tend to involve rhinocerebral, pulmonary, cutaneous, gastrointestinal tract with angioinvasive property and capability of systemic spread. On the other hand, entomophthoramycosis, an infection caused by Entomophthorales, is a chronic, indolent skin and soft tissue infection, usually present with masses, induration and disfigurement with rare systemic spread.[2],[3]
Saksenaea vasiformis is a Mucorales member that can be found ubiquitously in soil from tropical and subtropical area.[4] Since its first report as a human pathogen in 1977,[5] there are approximately only 45 cases reported till date.[6],[7] Seventy to eighty percent of the infection occurs in immunocompetent individuals with a history of trauma. Twenty percent of the patients are immunocompromised with an underlying condition such as diabetes mellitus, hematologic or solid organ malignancy. Unlike other mucormycosis, 73.8% of the infection is usually limited to soft tissue. However, less frequent rhino-orbito-cerebral, renal and disseminated infections have been reported.[6]
Cutaneous and subcutaneous infections caused by Saksenaea vasiformis primarily present with cellulitis, necrotizing fasciitis, abscess, papules and nodules that lead to ulceration as the pathogen is angioinvasive and triggers tissue necrosis.[6] Only some cases present with subcutaneous masses without ulceration [8] or mycetoma-like lesions.[9] Interestingly, our patient presents with diffuse infiltration with skin thickening at the centrofacial area, causing severe disfigurement. This finding is distinctive for a rare cutaneous fungal infection, rhinofacial entomophthoramycosis due to Conidiobolus coronatus.[10] We were unable to find any previous report of Saksenaea vasiformis causing this specific lesion. Hence, our case highlights overlapping clinical features among zygomycosis.
Treatments of Saksenaea vasiformis infections include surgical procedures and/or systemic antifungal therapy, e.g., amphotericin B, liposomal amphotericin B and posaconazole.[6],[11] A recent in vitro study reported that itraconazole was active against Saksenaea vasiformis isolates.[4] Therefore, itraconazole was included in our treatment regimen. Clinical improvement was observed; however, long-term outcome of the treatment cannot be evaluated since the patient was lost to follow-up.
In summary, we report this case of subcutaneous Saksenaea vasiformis infection mimicking rhinofacial entomophthoramycosis. Clinical manifestations and histopathology are impossible to distinguish between the two types of zygomycosis. Definite diagnosis relies on fungus culture or molecular techniques to identify the causative organisms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Acknowledgment
We would like to express our gratitude to Drs. Ratchathorn Panchaprateep and Jade Wititsuwannakul, for their excellence care for the patient and Ms. Navaporn Worasilchai, for the molecular identification.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | Chowdhary A, Randhawa HS, Gaur SN, Agarwal K, Kathuria S, Roy P, et al. Schizophyllum commune as an emerging fungal pathogen: A review and report of two cases. Mycoses 2013;56:1-10. [Google Scholar] |
| 2. | Gonzalez CE, Rinaldi MG, Sugar AM. Zygomycosis. Infect Dis Clin North Am 2002;16:895-914, vi. [Google Scholar] |
| 3. | Chayakulkeeree M, Ghannoum MA, Perfect JR. Zygomycosis: The re-emerging fungal infection. Eur J Clin Microbiol Infect Dis 2006;25:215-29. [Google Scholar] |
| 4. | Alvarez E, Garcia-Hermoso D, Sutton DA, Cano JF, Stchigel AM, Hoinard D, et al. Molecular phylogeny and proposal of two new species of the emerging pathogenic fungus Saksenaea. J Clin Microbiol 2010;48:4410-6. [Google Scholar] |
| 5. | Ajello L, Dean DF, Irwin RS. The zygomycete Saksenaea vasiformis as a pathogen of humans with a critical rewiew of the etiology of zygomycosis. Mycologia 1976;68:52-62. [Google Scholar] |
| 6. | Gomes MZ, Lewis RE, Kontoyiannis DP. Mucormycosis caused by unusual mucormycetes, non-Rhizopus, -Mucor, and -Lichtheimia species. Clin Microbiol Rev 2011;24:411-45. [Google Scholar] |
| 7. | Kaushik R, Chander J, Gupta S, Sharma R, Punia RS. Fatal primary cutaneous zygomycosis caused by Saksenaea vasiformis: Case report and review of literature. Surg Infect (Larchmt) 2012;13:125-9. [Google Scholar] |
| 8. | Lye GR, Wood G, Nimmo G. Subcutaneous zygomycosis due to Saksenaea vasiformis: Rapid isolate identification using a modified sporulation technique. Pathology 1996;28:364-5. [Google Scholar] |
| 9. | Padhye AA, Koshi G, Anandi V, Ponniah J, Sitaram V, Jacob M, et al. First case of subcutaneous zygomycosis caused by Saksenaea vasiformis in India. Diagn Microbiol Infect Dis 1988;9:69-77. [Google Scholar] |
| 10. | Choon SE, Kang J, Neafie RC, Ragsdale B, Klassen-Fischer M, Carlson JA. Conidiobolomycosis in a young Malaysian woman showing chronic localized fibrosing leukocytoclastic vasculitis: A case report and meta-analysis focusing on clinicopathologic and therapeutic correlations with outcome. Am J Dermatopathol 2012;34:511-22. [Google Scholar] |
| 11. | Vega W, Orellana M, Zaror L, Gené J, Guarro J. Saksenaea vasiformis infections: Case report and literature review. Mycopathologia 2006;162:289-94. [Google Scholar] |
Fulltext Views
2,659
PDF downloads
1,384





