Translate this page into:
Subungual exostosis on index finger in a child
Correspondence Address:
Piyush Kumar
Department of Dermatology, Katihar Medical College, Katihar, Bihar
India
| How to cite this article: Kumar P, Alam G. Subungual exostosis on index finger in a child. Indian J Dermatol Venereol Leprol 2018;84:232-233 |
A 7-year-old boy presented with a slow growing painful swelling under the nail of right index finger for 3 years. There was no history of prior trauma or chronic infection. The subungual nodule of around 1 cm in size was well-defined, bony hard, slightly tender, with a hyperkeratotic surface. Overlying nail plate was separated from nail bed and showed features of dystrophy [Figure - 1]a and [Figure - 1]b. Radiographs of the hand revealed an outgrowth of trabeculated bone projecting from and in continuity with distal phalanx of the right index finger on the dorsal aspect, with intact well-defined cortical margins. No destructive changes were noted in the distal phalanx [Figure - 1]c. These radiological findings confirmed the diagnosis of subungual exostosis. The patient was referred to the department of orthopedics for further management.
 |
| Figure 1a: Dorsal view of bony hard nodule on dorsal aspect of terminal phalanx. Overlying nail plate is dystrophic and separated from nail bed |
 |
| Figure 1b: Lateral view of nodular growth on dorsal aspect of terminal phalanx |
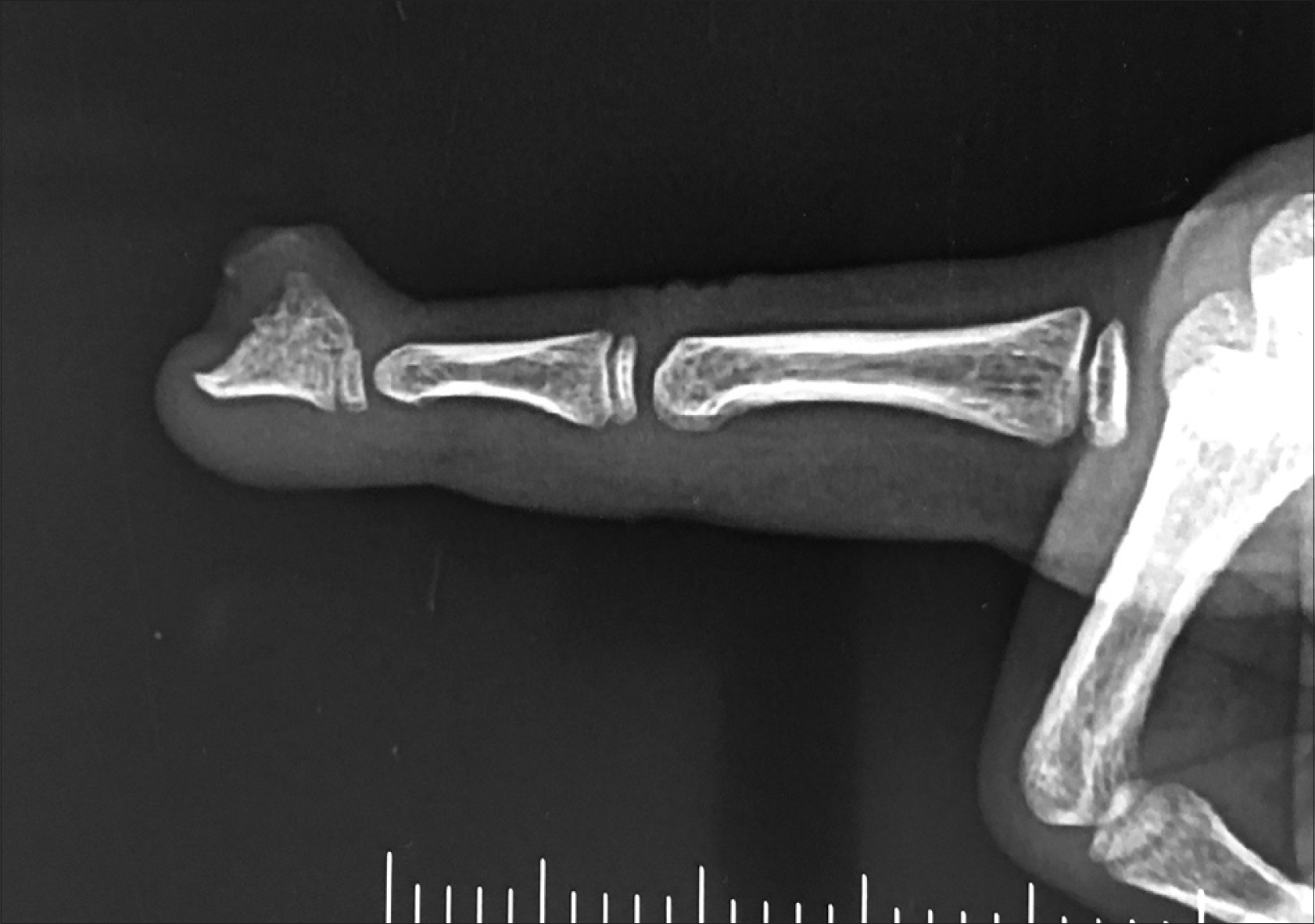 |
| Figure 1c: Radiograph showing radio-opaque mass overlying and in continuity with terminal phalanx of index finger |
Subungual exostosis is more common on toes and develops mostly during adolescence. Subungual exostosis is considered rare in young children and on fingers. Differentials include subungual verruca, carcinoma of the nail bed, keratoacanthoma, subungual epidermoid inclusions and Koenen tumor. All these entities are radiolucent. Enchondroma presents in a similar manner clinically, but it is radiolucent and causes expansion of phalanx itself. Subungual exostosis is treated surgically by excision and it needs to be excised up to the normal bone tissue, to prevent recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Fulltext Views
4,238
PDF downloads
2,554





