Translate this page into:
Subungual glomus tumors of the finger in a patient with type 1 neurofibromatosis
2 Department of Plastic Surgery, Osaka Medical College, Osaka, Japan
3 Department of Radiology, Osaka Medical College, Osaka, Japan
Correspondence Address:
Hiroko Kuwabara
Department of Pathology, Osaka Medical College, 2 7, Takatsuki, Osaka, 569 8686
Japan
| How to cite this article: Kuwabara H, Hara M, Yuki M, Shibayama Y. Subungual glomus tumors of the finger in a patient with type 1 neurofibromatosis. Indian J Dermatol Venereol Leprol 2013;79:424-425 |
Sir,
A thirty five-year-old Japanese woman, who was diagnosed as type 1 neurofibromatosis (NF1) based on the clinical features (more than six cutaneous café au lait spots, multiple neurofibromas, axillary freckling and mother had NF1), presented with paroxysmal pain to cold exposure or pressure in the left second fingertip. Macroscopically, the fingernail and nail bed were almost normal. Coronal T1-weighted magnetic resonance imaging (MRI) revealed two hypo-intense demarcated nodules (5 and 3 mm in size) in the subungual soft tissue adjoining the distal phalanx of the left second finger, which became hyper-intense on fat-suppressive T2-weighted images [Figure - 1]. The two nodules were present in different MRI slices. Gadolinium enhancement was not performed. Clinically and radiologically, these tumors were compatible with glomus tumors. Surgical extirpation of the two subungual tumors was performed. Both tumors were red-blue, and showed the same microscopic findings, confirming the diagnosis of glomus tumors. The tumor cells were small and uniform with a centrally located rounded nucleus and eosinophilic cytoplasm, and surrounded the small blood vessels [Figure - 2]a. Immunohistochemically, the tumor cells were positive for α-smooth muscle actin [Figure - 2]b. A subcutaneous tumor of the back (1 cm in size) was also extirpated, and it was non-encapsulated, and located in the dermis. Histologically, the tumor was composed of delicate fascicles of cells with oval or spindle-shaped nucleus [Figure - 3]. Postoperative follow-up for two years was uneventful and the symptoms disappeared completely.
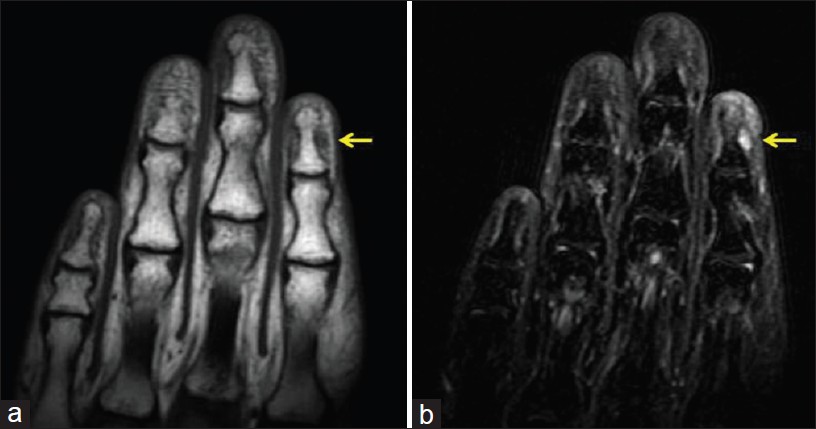 |
| Figure 1: Coronal T1-weighted (a) and fat-suppressive T2-weighted (b) Magnetic resonance images of the left second finger. A 5-mm nodule (arrow) is observed in the second finger, which is compatible with a glomus tumor |
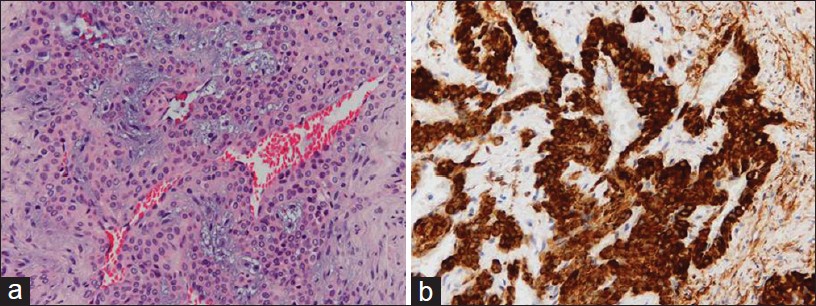 |
| Figure 2: (a) Uniform tumor cells arranged around blood vessels (H and E, × 200). (b) α -Smooth muscle actin-positive tumor cells (× 200) |
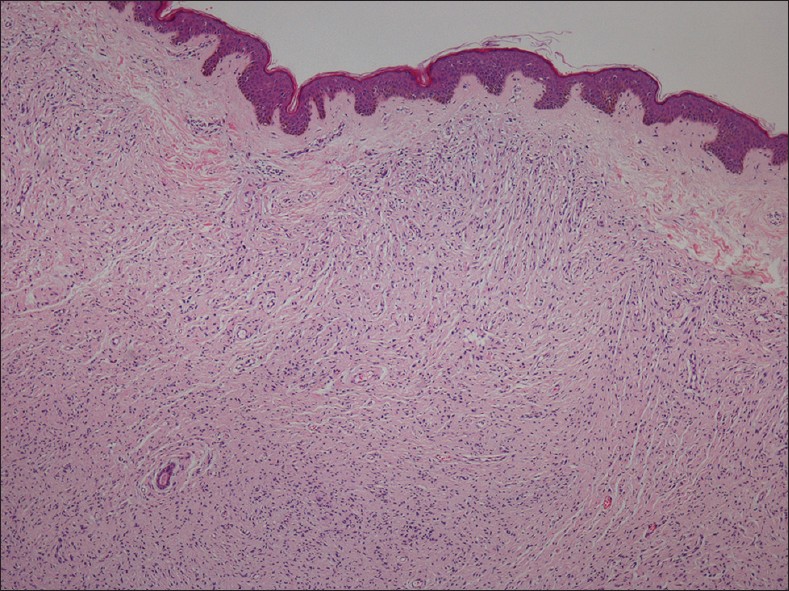 |
| Figure 3: Bland spindle cells proliferating in the dermis (H and E, × 40) |
Glomus tumors, which are usually present in the fingers and toes, are benign tumors that develop from cells closely resembling the modified smooth muscle cells of the glomus apparatuses. [1] NF1, an autosomal dominant inherited disorder, is caused by mutations of the NF1 gene located on chromosome seventeen. The protein encoded by the NF1 gene, neurofibromin, acts as a tumor suppressor. NF1 patients lose neurofibromin expression, which leads to increased cell proliferation associated with the rat sarcoma viral oncogene homologue mitogen activated protein kinase, and have a propensity to develop many different types of tumors. [2] To the best of our knowledge, there are twenty four published cases of NF1-associated glomus tumors. [3],[4],[5] The loss of neurofibromin function in NF1 patients is crucial for the pathogenesis of glomus tumors, and glomus tumors are thought to be part of the NF1 phenotype. [3] On the other hand, sporadic glomus tumors are almost always solitary, [1] whereas 10 (42%) patients among the reported NF1-associated glomus tumor cases had multiple glomus tumors, as observed in our case. Multiple occurrences may be a characteristic feature of NF1-associated glomus tumors.
This present case provides further support for the notion that NF1 has an associated risk for multiple glomus tumors. For dermatologists managing NF1 patients, awareness of this association may facilitate early diagnosis and appropriate therapy. In particular, MRI examination and the patient′s symptoms seem to be helpful for reaching a correct diagnosis.
| 1. |
Weedon D. Glomus tumor. In: Weedon D, editor. Weedon's skin pathology, 3 rd ed. China: Churchill Livingstone Elsevier; 2010. p. 907-8.
rd ed. China: Churchill Livingstone Elsevier; 2010. p. 907-8.'>[Google Scholar]
|
| 2. |
Brems H, Beert E, de Ravel T, Legius E. Mechanisms in the pathogenesis of malignant tumors in neurofibromatosis type 1. Lancet Oncol 2009;10:508-15.
[Google Scholar]
|
| 3. |
Brems H, Park C, Maertens O, Pemov A, Messiaen L, Upadhyaya M, et al. Glomus tumors in neurofibromatosis type 1: Genetic, functional and clinical evidence of a novel association. Cancer Res 2009;69:7393-401.
[Google Scholar]
|
| 4. |
Leonard M, Harrington P. Glomus tumour of the thumb in a child with neurofibromatosis: A case report. J Pediatr Orthop B 2010;19:310-2.
[Google Scholar]
|
| 5. |
Stewart DR, Sloan JL, Yao L, Mannes AJ, Moshyedi A, Lee C, et al. Diagnosis, management and complications of glomus tumours of the digits in neurofibromatosis type 1. J Med Genet 2010;47:525-32.
[Google Scholar]
|
Fulltext Views
3,441
PDF downloads
1,422





