Translate this page into:
Successful treatment of lichen amyloidosis with cryotherapy
Corresponding author: Dr. Asit K Mittal, Department of Skin & Venereal Disease, RNT Medical College, Udaipur, Rajasthan, India. asitmittal62@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar A, Mittal AK, Balai M, Jain S. Successful treatment of lichen amyloidosis with cryotherapy. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1778_2024
Dear Editor,
Lichen amyloidosis (LA), the most common primary localised cutaneous amyloidosis, presents as persistent pruritic 2-3 mm hyperkeratotic papules that may coalesce into plaques, typically on the lower extremities.1,2 Various treatments have shown limited success, with cryotherapy emerging as a promising but less frequently reported option.
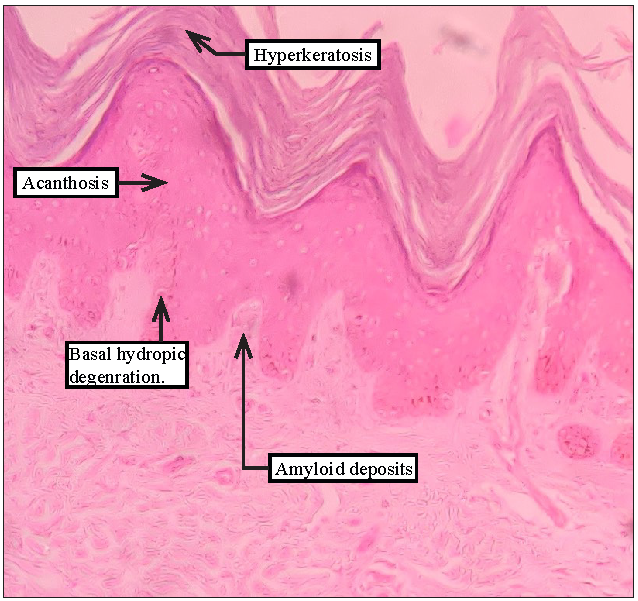
A 70-year-old man reported with the chief complaint of persistent, itchy eruptions on the anterolateral aspect of his left lower leg for 20 years [Figure 1]. His pruritus intensity was 8/10 on a Numeric Rating Scale (NRS), severely affecting his quality of life. A clinical diagnosis of lichen amyloidosis was made. The patient had previously received multiple treatment modalities, including intralesional triamcinolone injections, topical corticosteroids, systemic corticosteroids, and various over-the-counter (OTC) emollients, without lasting relief. He was otherwise healthy with no history of any other chronic illness.

- Discrete, hyperkeratotic papules on the left leg.
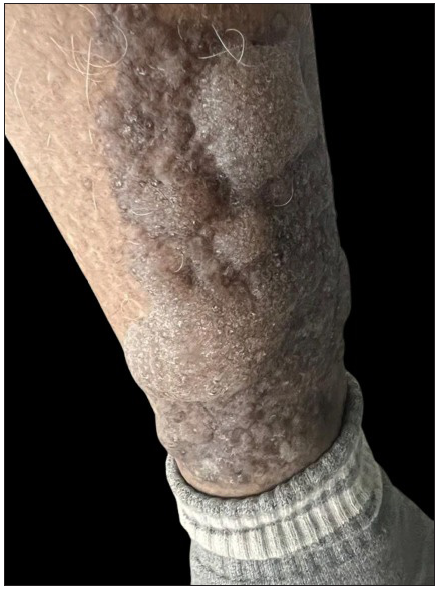
Physical examination showed a plaque composed of excoriated, firm, hyperpigmented, hyperkeratotic papules measuring 20 × 7 cm on the anterolateral aspect of the lower two-thirds of the left leg [Figure 1]. No other cutaneous or mucosal lesions were noted, and the patient was psychologically stable. There was no history of atopy. Routine laboratory investigations, including complete blood count, renal, hepatic, and thyroid function tests, and urinary analysis, were within normal limits. A punch biopsy revealed hyperkeratosis, hypergranulosis, irregular acanthosis, and basal hydropic degeneration in the epidermis. Additionally, small hyaline deposits of amyloid were identified in the papillary dermis [Figure 2], suggestive of lichen amyloidosis. Demonstration with special stains could not be undertaken.
- Epidermis showing hyperkeratosis, acanthosis, basal hydropic degeneration, small hyaline deposits of amyloid in the papillary dermis (Haematoxylin and eosin, 40x).
The patient was treated with liquid nitrogen cryotherapy using a cryogun with a single session of a 10-second double freeze-thaw cycle covering the entire area. Within 20 minutes, multiple bullae developed at the cryotherapy site [Figure 3]. The bullae were ruptured, and the site was dressed with povidone-iodine. The patient was instructed to follow up every three days for dressing change, and subsequent photographs were taken to track the progress. Blister resolution required a total of 6 dressing sessions over 18 days. Skin lesions regressed significantly over four months. Pruritus, initially rated as 8/10 on the NRS scale, was reduced to 1/10, and near-complete resolution of the lesions was achieved. Hypopigmentation was noted at the treatment site [Figure 4], but there was no recurrence during the 4-month follow-up period.
- Multiple bullae formation within 20 minutes of cryotherpay.
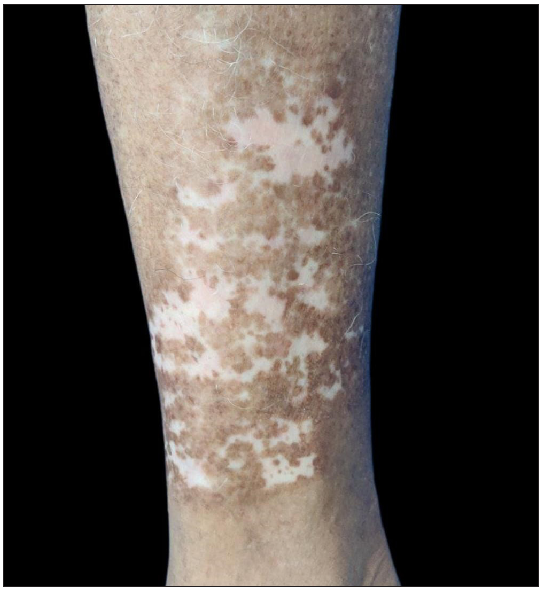
- Clearance of lesions with postinflammatory hypopigmentation after 4 months of cryotherapy on left leg.
Lichen amyloidosis is a primary cutaneous amyloidosis that involves the deposition of amyloids in the skin without internal organ involvement. The pathology is similar to lichen simplex chronicus and prurigo, and these conditions can be clubbed as “scratch lesions.” It typically affects the lower legs and may present symmetrically. It involves scratching, which leads to necrosis of keratinocytes and eventually to the formation of amyloids in the papillary dermis. Since chronic scratching seems to be the cause and not the result of the deposits of amyloid, treatment should be directed at alleviating pruritus.3 Several therapies, including topical and intralesional corticosteroids, dimethyl sulfoxide, Ultraviolet A, psoralen plus ultraviolet A (PUVA) therapy, and retinoids, have shown limited success.4,5 Topical and intralesional corticosteroids are commonly used to reduce inflammation and pruritus but are less effective against deep dermal amyloid deposits and thick plaques. Prolonged use risks side effects such as skin atrophy. Systemic treatments like retinoids and PUVA therapy may alleviate symptoms but involve challenges like teratogenicity, mucocutaneous side effects, and logistical constraints. Topical DMSO can dissolve amyloid deposits but has a strong odour and can cause contact dermatitis. Adjunctive use of emollients and anti-pruritic agents offers temporary relief but does not address the underlying amyloid deposits.
Cryotherapy breaks the itch-scratch cycle by temporarily disabling the sensory nerve endings that are responsible for transmitting itch signals to the brain, providing immediate relief from pruritus. Cryotherapy also leads to the destruction of epidermal cells that are rich in amyloid deposits.6 It also reduces the inflammatory response in itching by lowering the levels of inflammatory cells and mediators (histamine, substance P, and cytokines) through decreased local blood flow following application. Despite its effectiveness, challenges include bullae formation, hypopigmentation, and potential pain. Bullae may complicate post-treatment care, while hypopigmentation, particularly in darker skin, can affect patient satisfaction. Pain during the procedure may also limit its acceptability. A study by Sezer et al.6 found similar results; in contrast to our study, the patient was treated with liquid nitrogen cryotherapy using a 15-second, single freeze-thaw cycle.
In conclusion, cryotherapy may be an effective treatment for lichen amyloidosis that is resistant to other options, leading to significant clinical improvement and pruritus reduction, highlighting its potential in managing LA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Lichen amyloidosus: A consequence of scratching? J Am Acad Dermatol. 1999;41:501.
- [CrossRef] [PubMed] [Google Scholar]
- Primary localized cutaneous amyloidosis in association with papillary thyroid carcinoma. J Cutan Med Surg. 2002;6:332-4.
- [CrossRef] [PubMed] [Google Scholar]
- Lichen amyloidosus: a consequence of scratching. J Am Acad Dermatol. 1997;37:923-8.
- [CrossRef] [PubMed] [Google Scholar]
- Calcipotriol ointment vs. betamethasone 17-valerate ointment in the treatment of lichen amyloidosis. Int J Dermatol. 1999;38:539-41.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of phototherapy (UVB) vs. photochemotherapy (PUVA) vs. topical steroids in the treatment of primary cutaneous lichen amyloidosis. Photodermatol Photoimmunol Photomed. 2001;17:42-3.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of lichen amyloidosis with cryosurgery. Gülhane Týp Dergisi. 2006;48:112-4.
- [PubMed] [Google Scholar]





