Translate this page into:
Successful treatment of total obliteration of vulva caused by inveterate vulvar lichen sclerosus
Correspondence Address:
Stefano Basile
Outpatient Department of Vulvar Disease, Pisa University Hospital, via Roma 67, 56126 Pisa
Italy
| How to cite this article: Pinelli S, Basile S, Salerno MG. Successful treatment of total obliteration of vulva caused by inveterate vulvar lichen sclerosus. Indian J Dermatol Venereol Leprol 2017;83:725-727 |
Sir,
Total fusion of the labia minora is relatively uncommon, with only a few cases reported in women of reproductive age. There is no consensus on optimal treatment, despite this being a serious condition with tragic impairment of quality of life when irreversible anatomical distortion occurs.[1],[2],[3] The Koebnerization phenomenon (isomorphic response to trauma) or recurrent scarring of tissue may discourage surgical intervention.[1],[2],[3] However, surgery is necessary when extensive adhesions cause anatomical distortion and loss of function impairs quality of life.
A 42-year-old woman was referred for urinary incontinence, dysuria, vulvar itching, and spotting for 1 year. She had four early miscarriages, the last one 4 years prior, after which she decided to forego any further attempt at conceiving.
On physical examination, it was impossible to identify vulvar structures: the labia minora were completely fused along the midline with burial of the clitoris and total obliteration of the vaginal introitus [Figure - 1]. Urethral meatus was hidden and a pinhole orifice at the midline was the only way for the outflow of urine and menstrual blood, resulting in slow persistent dripping of menstrual blood and urine. The patient was unable to report how long it has been since the skin lesions appeared; however, she reported being sexually inactive for the last 2 years.
 |
| Figure 1: The patient at presentation: Complete fusion of the labia minora along the midline with total obliteration of vaginal introitus, with associated burial of clitoris. Urethral meatus was hidden. A pinhole opening at the midline permitted a dripping outflow of urine and menstrual blood |
A medical history of persistent severe vulvar itching and soreness as well as the morphological appeareance of the vulvar and perineal area suggested the diagnosis of inveterate vulvar lichen sclerosus. The affected skin was pale, thinned, and wrinkled. Inveterate disease had determined scarring of tissue, with complete obliteration of vaginal introitus. A vulvar biopsy confirmed the clinical suspicion of lichen sclerosus [Figure - 2]. Pelvic ultrasound image showed a 2.5-cm submucous uterine leiomyoma.
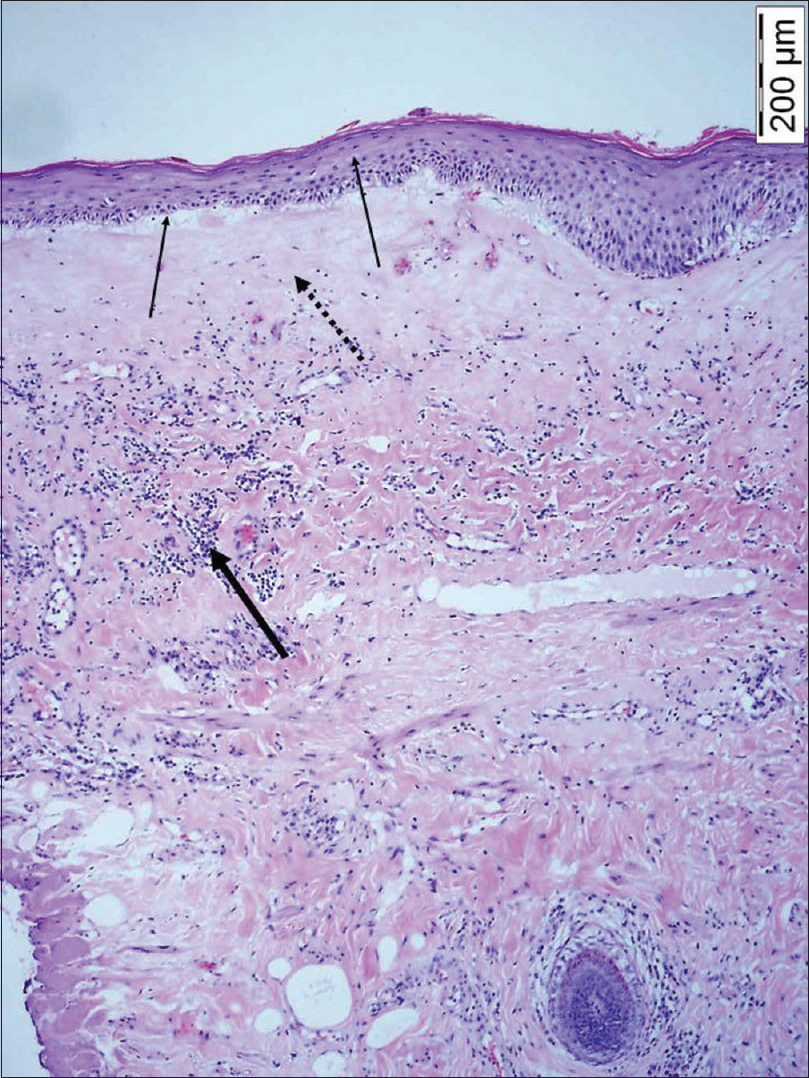 |
| Figure 2: Histologic examination: Vulvar lichen sclerosus (H and E, ×10). In the figure we can note atrophy of the epidermis with loss of rete ridges (thin arrows), homogenization of collagen in the upper dermis (dotted arrow), and a band-like lymphocytic infiltrate in the dermis (thick arrow) |
Despite a prolonged course of topical clobetasol, clinical symptoms continued until the patient requested surgical intervention for vulvar plastic surgery and simultaneous hysteroscopic myomectomy. After cold knife median incision, the labia were separated by digital blunt dissection of adhesions along the midline, exposing the urethral meatus behind the previously fused labia [Figure - 3]. The narrowed vaginal introitus was easily widened by digital pressure and hysteroscopic myomectomy was performed. Soaked gauzes, changed three times daily until healing, were applied to keep the labia separated, while vaginal packing was maintained for 2 days. Our patient used anti-adhesion oily medications. One week after surgery, she was started on a regimen comprising morning applications of daily estrogen ointment, topical emollient at noon, and clobetasol ointment at night for 3 months, administered continuously three times a week.[1],[2],[3] She could resume sexual activity and micturition. At 1-year follow-up, she had no relapse. The patient signed informed consent for scientific publication of the case and local institutional review board approved this report.
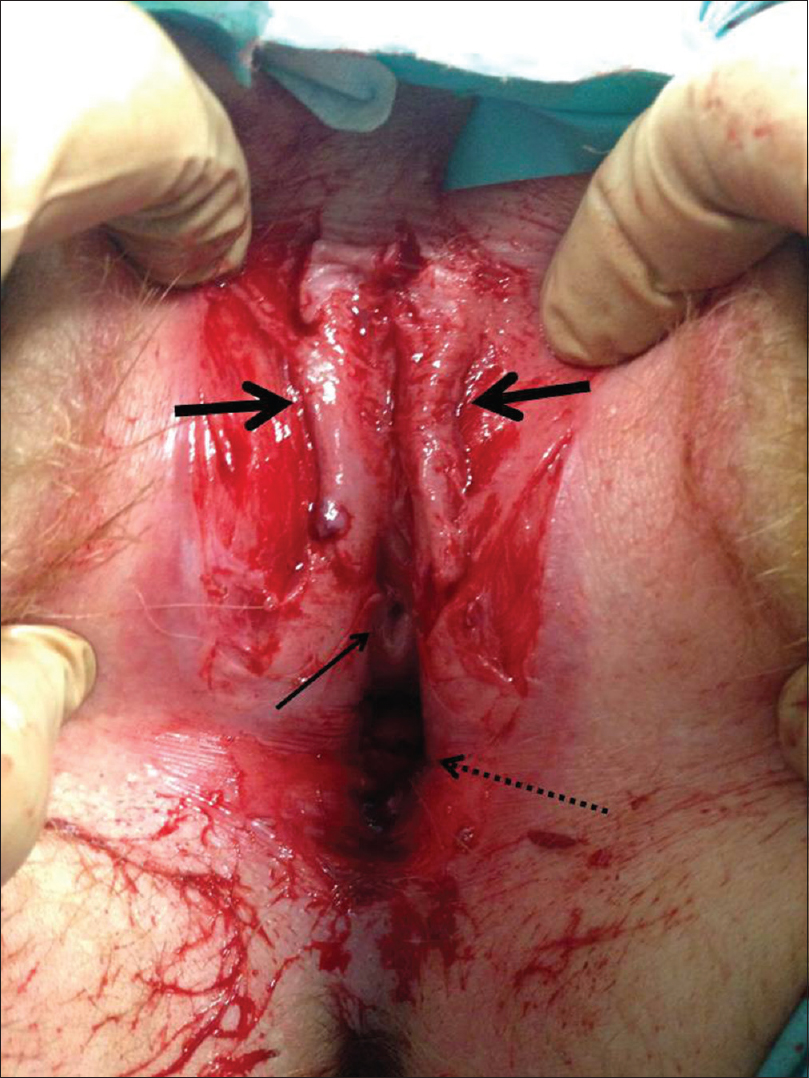 |
| Figure 3: The vulva with separated labia minora (thick arrows). The urethral meatus finally exposed behind the previously fused labia minora (thin arrow).. Exposed vaginal introitus (dotted arrow) |
Lichen sclerosus is a chronic, inflammatory dermatosis with a predilection for genital localization. The exact pathogenesis of the disease remains unclear; however, there is an association with autoimmune disorders in several patients.[1] Lack of familiarity with the disease and failure to examine the genital region can seriously prevent the correct diagnosis. In fact, the delay in diagnosis in our patient and the subsequent severe sequelae reveal the importance of expertise in vulvar disease, as well as the need for clinicians to increase their consideration of genital symptoms to ensure proper treatment for patients.
Since lichen sclerosus patients may be addressed by specialists in different medical areas, i.e., gynecologists, dermatologists, urologists and general practitioners, strong evidence produced by large randomized clinical trials is lacking. In addition, general expertise on this subject is scarce, as confirmed by the paucity of related literature. Consequently, patients frequently pay the price for this neglected condition.
Psychological trauma caused by repeated spontaneous miscarriages can lead to devastating consequences in women [4]. In this case, our patient was demotivated enough to give up plans of conception, periodic check ups and sexual activity. Noticeably, our patient was referred for urinary incontinence, not for complete distortion of vulvar architecture and apareunia. After surgery and counseling, she was able to retrieve her sexual health and preserve her relationship. The largest case series on the long-term results of vulvar surgery for lichen sclerosus was recently published.[5] The study had a mean time of follow-up of 8.4 years. The researchers found a minor relapse of the disease in eight (50%) patients, with clinical symptoms that were considerably lower than before surgery. After a median of 5 years after primary surgery, only six (38%) patients demonstrated a significant relapse of lichen sclerosus. In those patients, a second surgical procedure was performed, in consideration of the noticeable advantages obtained with the first surgery.
Despite the removal of the intracavitary myoma, which may have caused the repeated miscarriages, our patient's age may make it difficult for her to sustain a successful full-term pregnancy. Nevertheless, her genital consciousness, sexual well-being, and intimacy with her partner have been preserved. Surgery followed by medical therapy proved to be a valid option for anatomical distortion subsequent to advanced vulvar disease. The possible recurrence after surgery requires long-term follow-up, and chronic local corticosteroid therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kreuter A, Kryvosheyeva Y, Terras S, Moritz R, Möllenhoff K, Altmeyer P, et al. Association of autoimmune diseases with lichen sclerosus in 532 male and female patients. Acta Derm Venereol 2013;93:238-41.
[Google Scholar]
|
| 2. |
Goldstein AT, Burrows LJ. Surgical treatment of clitoral phimosis caused by lichen sclerosus. Am J Obstet Gynecol 2007;196:126.e1-4.
[Google Scholar]
|
| 3. |
Gurumurthy M, Morah N, Gioffre G, Cruickshank ME. The surgical management of complications of vulval lichen sclerosus. Eur J Obstet Gynecol Reprod Biol 2012;162:79-82.
[Google Scholar]
|
| 4. |
Lok IH, Neugebauer R. Psychological morbidity following miscarriage. Best Pract Res Clin Obstet Gynaecol 2007;21:229-47.
[Google Scholar]
|
| 5. |
Rangatchew F, Knudsen J, Thomsen MV, Drzewiecki KT. Surgical treatment of disabling conditions caused by anogenital lichen sclerosus in women: An account of surgical procedures and results, including patient satisfaction, benefits, and improvements in health-related quality of life. J Plast Reconstr Aesthet Surg 2017;70:501-8.
[Google Scholar]
|
Fulltext Views
12,920
PDF downloads
1,828





