Translate this page into:
Successful use of topical ivermectin in the treatment and maintenance of lupus miliaris disseminatus faciei
Corresponding author: Dr. Anshuman Dash, Dermatology, and STD Vardhman Mahavir Medical College and Safdarjung Hospital, South Delhi, India. anshu.sipun@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dash A, Verma P, Srivastava P, Choudhary A, Goyal A, Khunger N, et al. Successful use of topical ivermectin in the treatment and maintenance of lupus miliaris disseminatus faciei. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_28_2024
Dear Editor,
Lupus miliaris disseminatus faciei (LMDF) is a chronic granulomatous dermatosis of uncertain aetiology. It presents as asymptomatic monomorphic erythematous to skin-coloured papules predominantly on the face. The lesions usually regress spontaneously during the course of one to two years with pitted scars. Currently, available treatment modalities are often ineffective. Here, we report a case of LMDF in a middle-aged female, with an excellent response to a combination of oral doxycycline, oral metronidazole, and topical ivermectin.
A 44-year-old female with Fitzpatrick-IV skin presented with multiple asymptomatic erythematous, round, discrete to coalescing papules ranging from size 1×1 cm to 1×2 cm on the face of seven to eight months duration [Figure 1]. The centro-facial area and the uninvolved skin were spared with no background erythema, scaling or telangiectasias. The patient was prescribed tacrolimus 0.03% cream and oral prednisolone in a dose of 1 mg/kg for 14 days by a private practitioner with no response. She had no personal or family history of tuberculosis. Ophthalmological evaluation was normal. Hemogram, renal function test, hepatic function test, urine analysis, blood sugar, and serum electrolytes, including calcium and chest X-ray, were normal. Microscopic examination of skin scrapings from the lesions did not reveal demodex mites. Histopathology of a representative skin lesion revealed thinned out epidermis with foci of caseous necrosis surrounded by palisading epithelioid cells and giant cells [Figures 2a and 2b]. Multiple sections of the tissue failed to show either solar elastosis or capillary dilatation in the dermis. Parts of demodex mites were found in multiple hair follicles [Figure 2c]. Accordingly, a diagnosis of LMDF was rendered and the patient was started on doxycycline 100 mg twice daily perorally and metronidazole 400 mg twice daily perorally, along with topical ivermectin 1% cream for daily night-time application. After 30 days of treatment, the lesions regressed. Subsequently, doxycycline and metronidazole were stopped while topical ivermectin was continued. After three months with only topical ivermectin, residual lesions had flattened with no scarring or new lesions [Figure 3].
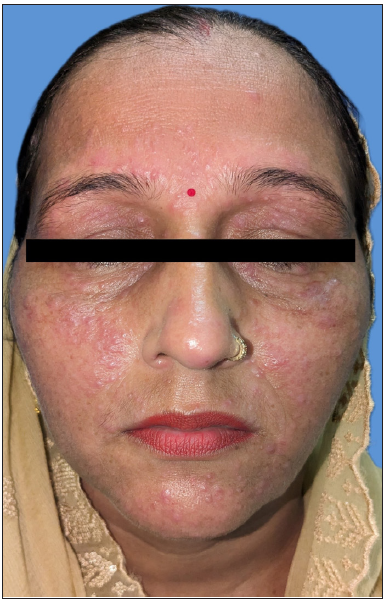
- Monomorphic, erythematous papules of LMDF on the face including eyelids, cheeks and chin, and sparing centro-facial region.
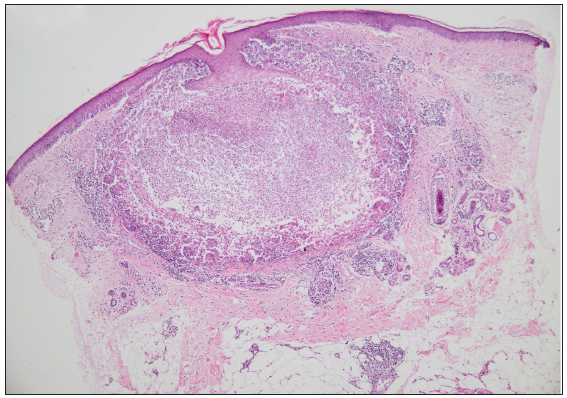
- Histopathology shows thinned-out epidermis. Dermis shows a large area of necrosis surrounded by palisading epitheloid cells and giant cells (Haematoxylin and eosin; 40x).
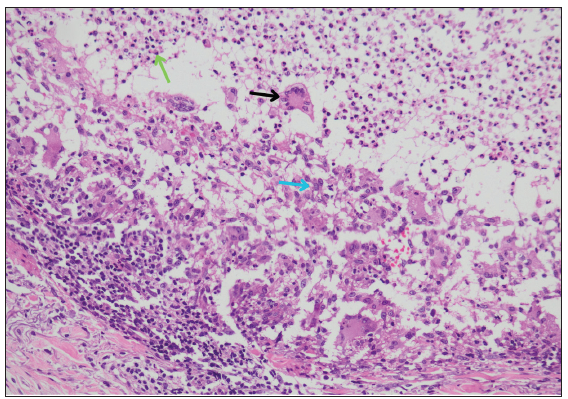
- Higher power view shows necrotic tissue containing a collection of neutrophils (green arrow) and surrounded by palisading epitheloid cells (blue arrow) and giant cells (black arrow) (Haematoxylin and eosin; 200x).
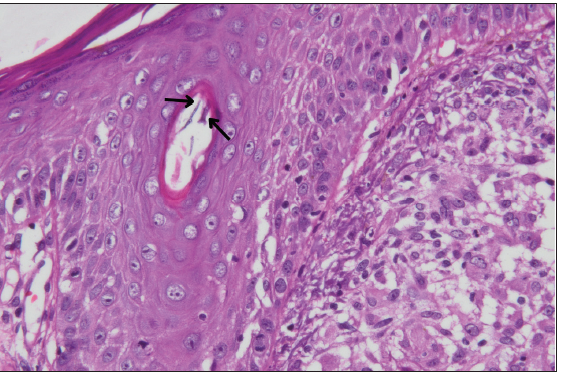
- Higher power view of a hair follicle containing parts of Demodex (black arrows) (Haematoxylin and eosin; 400x).

- Post-treatment image after 3-months showing flattening of lesions without scarring.
LMDF is challenging for clinicians to treat because of its uncertain aetiology and lack of controlled studies to devise effective treatments.1 Despite various hypotheses, none convincingly pinpoint its aetiology. Initially considered to be a tuberculid due to the presence of tuberculoid granuloma with caseation necrosis in LMDF, further studies failed to demonstrate any evidence of Mycobacterium tuberculosis.2 During the 1980s, LMDF was considered to be a variant of granulomatous rosacea (GR) since both the diseases have similar presentations.3 However, many clinical features in LMDF differ strikingly from GR like involvement of eyelids, lack of background erythema and telangiectasias, and absence of caseation necrosis in the GR. Also, LMDF usually runs a self-limiting course with spontaneous resolution in one to two years, often with scarring.4 Propionibacterium acnes was also suggested to be responsible, as their signatures were found to be associated with granulomas in a case series of nine patients.5 But this still needs further research. Demodex folliculorum has been found in association with caseating granulomas of LMDF, but inconsistently.1,6
Owing to the varied pathogenetic mechanisms, multitude of treatments options have been tried viz systemic steroids, tetracyclines, dapsone, isotretinoin and topical tacrolimus with variable and unpredictable response.1 In our case, the presence of Demodex mite remnants in multiple hair follicles prompted us to start the patient on oral tetracycline along with oral metronidazole and topical ivermectin. To our knowledge, this is the first reported use of topical ivermectin cream in a case of LMDF. As elucidated by its role in papulopustular rosacea, anti-acaricidal and anti-inflammatory actions could be the plausible mechanisms by which ivermectin might act in LMDF.7 Furthermore, the histopathology and treatment outcome in our case suggest Demodex as a possible agent responsible for aberrant immune responses resulting in caseation necrosis in the pilosebaceous unit, which needs further research.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Nosology and therapeutic options for lupus miliaris disseminatus faciei. J Dermatol. 2011;38:864-73.
- [CrossRef] [PubMed] [Google Scholar]
- Lupus miliaris disseminatus faciei – The DNA of Mycobacterium tuberculosis is not detectable in active lesions by polymerase chain reaction. Br J Dermatol. 1997;137:614-19.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical and histopathologic study of granulomatous rosacea. J Am Acad Dermatol. 1991;25:1038-43.
- [CrossRef] [PubMed] [Google Scholar]
- Lupus miliaris disseminatus faciei versus granulomatous rosacea: A case report. Case Rep Dermatol. 2021;13:321-29.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The detection of propionibacterium acnes signatures in granulomas of lupus miliaris disseminatus faciei. J Dermatol. 2015;42:418-21.
- [CrossRef] [PubMed] [Google Scholar]
- Demodex-induced lupus miliaris disseminatus faciei: A case report. Medicine (Baltimore). 2020;99:e21112.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Topical Ivermectin in the treatment of papulopustular rosacea: A systematic review of evidence and clinical guideline recommendations. Dermatol Ther (Heidelb). 2018;8:379-87.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






