Translate this page into:
Sun-related behaviors among individuals previously diagnosed with non-melanoma skin cancer
2 Department of Health, Exercise Science and Recreation Management, The University of Mississippi, Jackson, MS, USA
3 Department of Dermatology, University of Mississippi Medical Center, Jackson, MS, USA
4 Department of Health and Human Performance, College of Education, Health, and Behavioral Sciences, The University of Tennessee at Martin, Martin, TN, USA
5 Department of Dermatology, University of Mississippi Medical Center, Jackson, MS; Department of Pathology, University of Mississippi Medical Center, Jackson, MS; Department of Dermatology, University of Rochester School of Medicine and Dentistry, Rochester, NY, USA
Correspondence Address:
Vinayak K Nahar
The University of Mississippi, 236 Turner Center, University, MS 38677
USA
| How to cite this article: Nahar VK, Ford M A, Jacks SK, Thielen SP, Johnson AK, Brodell RT, Bass MA. Sun-related behaviors among individuals previously diagnosed with non-melanoma skin cancer. Indian J Dermatol Venereol Leprol 2015;81:568-575 |
Abstract
Compared to the general population, the risk of developing non-melanoma skin cancer is considerably higher among individuals with a previous history of this condition. Protection from ultraviolet (UV) radiation is the primary evidence-based approach for minimizing this risk. This review was aimed to assess the prevalence of sun-safe behaviors in non-melanoma skin cancer survivors. Searches were conducted in six electronic databases including PubMed, Psyclnfo, CINAHL, EMBASE, ERIC and Science Direct. A narrative approach was adopted to synthesize the data. The findings demonstrated that respondents do not protect themselves optimally from UV radiation exposure. Low levels of perceived skin cancer risk, a lack of knowledge about effective sun protection strategies and the inconvenience associated with sun-safe behaviors appear to explain this finding. A note of caution is required here, as there is a potential for publication bias. Moreover, the results of this study cannot be generalized to all non-melanoma skin cancer patients. Skin cancer survivors must be educated about their increased risk of future skin cancers. Behavioral interventions must be developed to increase the adoption of skin protective behaviors in this high-risk population group.Introduction
Non-melanoma skin cancers, including squamous cell carcinoma and basal cell carcinoma, are the most frequently diagnosed forms of skin cancer.[1] At the population level, the likelihood of developing squamous cell carcinomas is less compared to basal cell carcinoma; however, squamous cell carcinoma metastasizes more frequently and has a greater mortality rate.[2] Worldwide, between 2 and 3 million squamous cell carcinomas and 10 million basal cell carcinomas are reported annually.[3],[4] In the White population, since 1960, the incidence of non-melanoma skin cancer has increased annually by an average of 3–8% in countries such as Australia, Canada, Europe, and the United States.[5] Australia has the highest non-melanoma skin cancer incidence rates in the world, approximately 10 times higher than that recorded in the United Kingdom.[6] In the US, around 3.5 million people are diagnosed with non-melanoma skin cancer, and nearly 2000 of these individuals succumb to the disease each year.[7] Although non-melanoma skin cancers do not account for high mortality rates, these malignancies cause significant morbidity and lead to enormous annual health care costs.[8] The annual financial cost associated with non-melanoma skin cancer treatment is approximately $4.8 billion in the US.[9]
The diagnosis of non-melanoma skin cancer portends a significantly increased risk of developing new skin cancers of all kinds including malignant melanoma. A meta-analysis showed that, after an index squamous cell carcinoma, the mean 3-year cumulative risk of developing another squamous cell carcinoma is 18%, representing about a 10-fold increase in incidence compared with the incidence rate of first tumors in a comparable general population.[10] After the first basal cell carcinoma, the mean 3-year cumulative risk of subsequent basal cell carcinoma is 44%. This also represents a 10-fold increase in incidence compared to the first-time basal cell carcinoma rate in the general population.[10] More alarmingly, there is a 3.4% increased risk of developing malignant melanoma during the 4-year period after the diagnosis of non-melanoma skin cancer.[11]
Approximately, 90% of all non-melanoma skin cancers are caused by sunlight exposure.[12] However, the risk of skin cancer could be lowered dramatically by engaging in sun protection practices. Recommended primary prevention strategies involve seeking shade during mid-day when the sun is strongest (between 10:00 a.m. and 2:00 p.m.), wearing protective clothing (e.g., wide-brimmed hat, long sleeved shirts, long pants, and sunglasses), and appropriately using sunscreen with a sun protection factor of at least 30.[13]
In recognition of the increased risk of skin cancer in patients previously diagnosed with non-melanoma skin cancer, we carried out a review to provide an overview of ultraviolet (UV) radiation exposure and sun protection behaviors in people with a history of non-melanoma skin cancer across the US and other countries. A secondary goal was to discuss the correlates of sun-related behaviors among this population group. Finally, we included recommendations to guide future research and develop intervention programs, specifically targeting individuals with a history of skin malignancy.
Methods
The methodology section of this review comprised of two stages. In stage one, without placing date restrictions, literature searches were conducted in PubMed, PsycInfo, CINAHL, EMBASE, ERIC, and Science Direct. In order to identify pertinent studies, the following Boolean terms were used: “skin cancer survivors and UV radiation exposure” and “skin cancer survivors and sun protection behaviors.” Further searches were performed in Google Scholar and a University library to make sure relevant published papers were not missed. No attempt was made in the present study to assess gray literature.
In stage two, papers retrieved through electronic computerized searching were combined and then duplicates were eliminated from the list. After accounting for eligibility criteria, titles and abstracts were analyzed, and irrelevant studies were removed. Next, remaining studies were considered for full-text review to assess potentially eligible studies. Reference lists of eligible studies were scanned for additional relevant articles.
Studies were included in this review if they: (1) exclusively targeted non-melanoma skin cancer survivors; (2) used observational design; (3) measured either UV radiation exposure or sun protection practices; and (4) were English language literature published in a peer-reviewed journal. The criteria for excluding studies from this review were: (1) qualitative methodology; (2) review papers, meta-analyses, and conference abstracts.
Two independent reviewers (VKN and MAF) completed each aforementioned stage of methodology. Disagreements that occurred between the reviewers at any stage were resolved through discussion.
Because of very limited data available and differences in the measurement of sun protection behaviors, we could not use statistical techniques to combine the quantitative data extracted from the included studies. Therefore, a narrative approach was adopted to review the literature on this topic. Associations with a P value below 0.05 were considered statistically significant. If a study consisted of both bivariate and multivariate analysis findings, then only multivariate relationships were extracted for this review.
Results
A total of 85 studies were retrieved through online electronic searches. After eliminating duplicates, 55 titles and abstracts were scanned, which resulted in 19 papers for full-text review. Based on pre-determined inclusion and exclusion criteria, seven studies were included in this review. Additionally, one study was generated through reference list screening of seven potentially eligible studies. In all, eight studies that met the eligibility criteria were included in this review [Figure - 1].
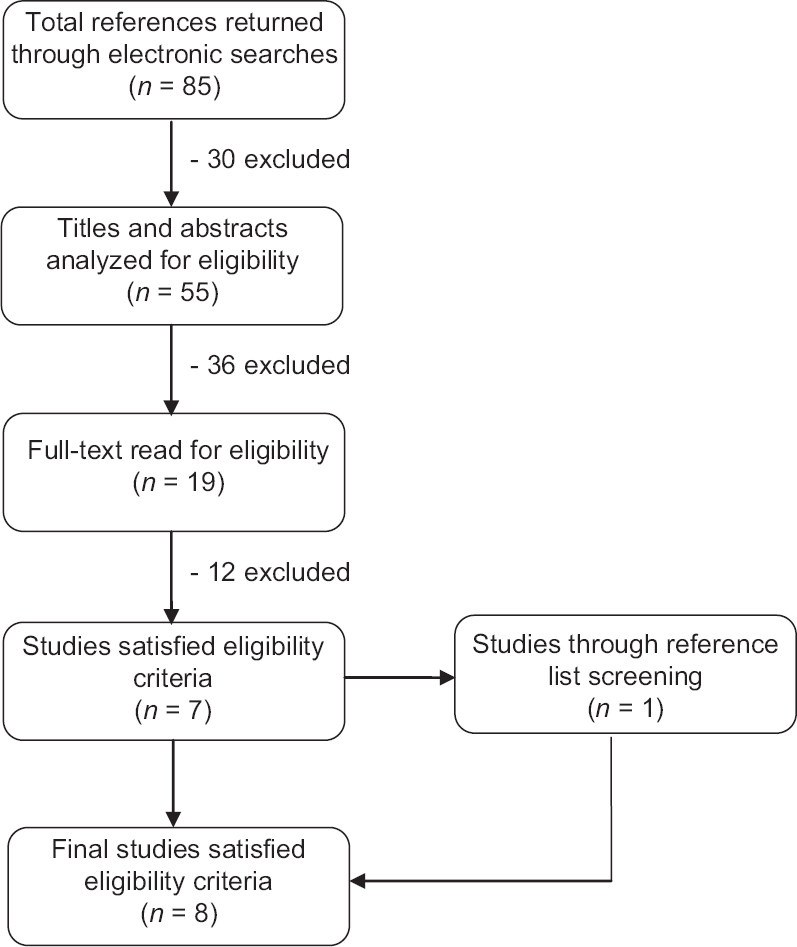 |
| Figure 1: Literature search procedure |
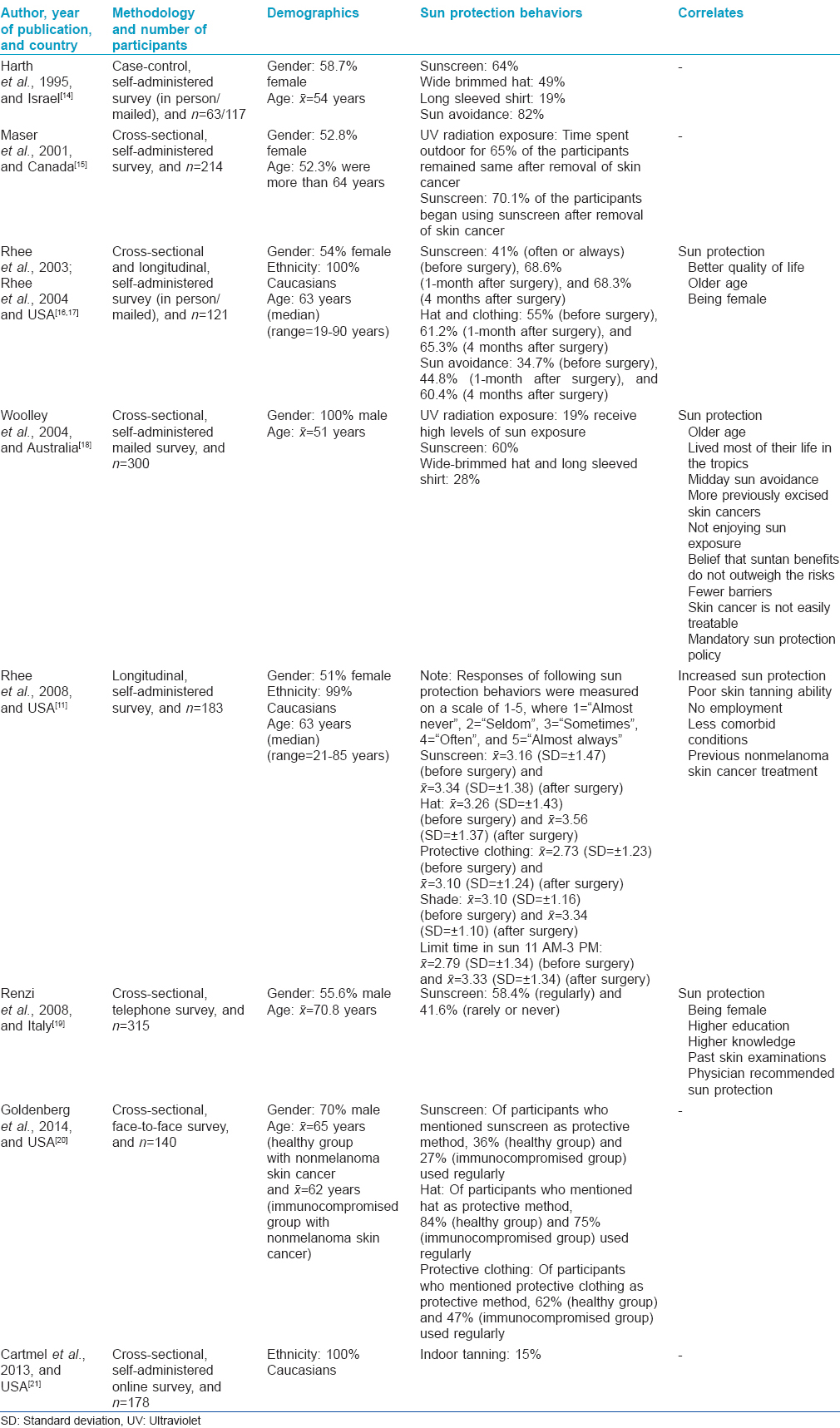
In [Table - 1], we have summarized the study characteristics (e.g., year of publication, country, methodology, and number of participants), participant characteristics (e.g., gender, ethnicity, and age), measures (e.g., UV radiation exposure and sun protection behaviors), and correlates of sun protection behaviors. The data are arranged in ascending order of the year of publication.
Discussion
Although the data are very limited, the findings of this study are particularly alarming and worthy of consideration for future research and intervention programs. The non-melanoma skin cancer patients continued to practice health-compromising behaviors, such as working in a heavy sun exposure environment and engaging in indoor tanning behaviors.[18],[21] It was also reported that about 40% do not avoid outdoors in the middle of the day when the sun is at its peak.[16] This suggests not only that more research is required in this area, but also that health care professionals should continue to inform non-melanoma skin cancer patients about the dangerous effects of natural and artificial exposure to UV radiation exposure. It appears that patients with non-melanoma skin cancer continue to harbor cognitive beliefs about the positive benefits of sun tanning, even after skin cancer diagnosis. Evidence suggests that the belief that a suntan improves physical attractiveness strongly influences intentional UV radiation exposure.[22],[23] Future survey studies should consider incorporating additional items to assess survivors' appearance-related attitudes. One strategy would be to emphasize the negative effects of UV exposure on future appearance such as premature aging or perhaps to substitute safe sunless tanning options.
Another troubling finding relates to skin cancer primary preventative behaviors. An Israeli-based study indicated that 49% of non-melanoma skin cancer patients wore wide-brimmed hats and only 19% wore long sleeved shirts on a regular basis during the summer months.[14] Furthermore, just 28% of North Australian men who had a history of non-melanoma skin cancer reported wearing a wide-brimmed hat and long sleeved shirt.[18] An Italian study targeting a large sample of non-melanoma skin cancer patients revealed that a substantial percentage (41.6%) “rarely or never” applied sunscreen.[19] A study in US showed that 55% of the non-melanoma skin cancer patients used protective clothing.[17] Moreover, a recent US study reported that of respondents that recognized sun protection strategies, 36% applied sunscreen and 62% wore protective clothing regularly.[20] These data suggest that health care professionals are not effectively presenting the risks of UV radiation exposure to their patients with non-melanoma skin cancer in a manner that motivates them to engage in protective behaviors.
One possible explanation for inadequate protective behaviors is that patients' perceived risk of skin cancer is not as high as would be desired.[11],[15] This result may be partially explained by the fact that patients showed low levels of skin cancer knowledge.[19] According to the Health Belief Model, a health behavior change is more likely to occur in individuals who perceive themselves to be at risk for a health problem and the perceived risk to a given health problem depends on knowledge about the problem.[24] Aside from these explanations, some studies have attempted to establish the primary barriers cited for not engaging in sun safety practices. They were “sunscreen is too messy and oily” and “clothing is too hot to wear.”[18],[20] All of the aforementioned concerns highlight the need for continuous development of psycho-educational interventions that increase knowledge about the risk factors for non-melanoma skin cancer patients, modify attitudes about sun exposure, and motivate behavioral health change. This will help in improving their sun protection practices which may decrease the risk of future skin cancer among this highly susceptible group.
Among the eight studies selected for this review, five involved a multivariate analysis to assess correlates of sun protective behaviors. A recurring theme was the relationship between patients' beliefs and attitudes regarding sun exposure and the likelihood of using sun protection. People who felt they could not suntan, disliked being in the sun and/or minimized the value of sun exposure were more likely to practice some form of sun protection.[18] Those who stated not enjoying sun exposure, and/or believed that the benefits of sun exposure do not outweigh the risks were found to be more likely to use protective clothing while in the sun.[18] Increased sun protection was also found amongst those who listed themselves as having poor skin tanning ability.[11] Although data on these correlates are limited, they suggest the possible benefit of a closer examination of the relationship between attitudes and beliefs regarding sun exposure and sun protection.
Another common correlation was increased sun protection among those who had been previously diagnosed with non-melanoma skin cancer. In general, a history of treatment for non-melanoma skin cancer does increase the use of various sun protective behaviors by 21.8–30.7%.[16] Patients with a history of multiple non-melanoma skin cancers are more likely to use sun protection when compared to those who have undergone treatment for a single non-melanoma skin cancer.[11],[18] Men with prior non-melanoma skin cancer who had lived most of their life in the tropics were more likely to use sun protection. Even more interestingly, men over age 50 years were more likely to use protective clothing while men who used sunscreen tended to be younger. This suggests that these men may have realized through experience that sunscreen alone provides inadequate protection compared to the use of long sleeved shirts and wide-brimmed hats.[18] While these results are promising in that patients do appear to adopt more protective strategies after a diagnosis of non-melanoma skin cancer, they are less promising in that the results also suggest that multiple experiences over many years may be necessary before patients make changes in their behavior.
Several other demographic variables influenced patients' use of sun protection after a diagnosis of non-melanoma skin cancer. A survey revealed that males were nearly 1.5 times less likely than females to limit their sun exposure during peak hours.[16] In another study, the multivariable analysis indicated that females reported more frequent use of sunscreen compared to males.[19] These gender differences may be attributable to higher knowledge regarding skin cancer and greater perceived susceptibility among females compared to males.[25] Age-related discrepancies were also noted in the literature. As discussed above, older males are more likely to wear protective clothing, and another study revealed that older patients are more likely to avoid the mid-day sun.[18],[16] Employed patients were less likely to engage in sun protective behaviors, which may be due to the confounding variable of age, as those in the workforce tended to be younger, as well as more susceptible to societal pressures to maintain what is perceived as a “healthy” or “attractive” skin tan.[11] Patients with other medical co-morbidities were less likely to change their behavior, perhaps due to focusing on other concerns that were perceived to be more pressing.[11] In light of these results, future skin cancer educational interventions may be more beneficial if targeted toward specific population subgroups of non-melanoma skin cancer patients.
The studies we reviewed highlight several opportunities for improving rates of use of sun protection among non-melanoma skin cancer patients. Men with a history of non-melanoma skin cancer who worked for companies with a mandatory sun protection policy were more likely to engage in sun protection behaviors.[18] This calls attention to the need for companies to implement and enforce sun protection policies for outdoor workers. Additionally, patients who were advised by their physicians to use sunscreen did increase use, which underscores the role that dermatologists and other physicians can play in impacting sun protective behaviors.[19]
Unfortunately, studies have shown that treatment of non-melanoma skin cancer does not lead to changes in other preventive health behaviors related to diet, smoking, and exercise.[11] While they do seem to realize that the risk of developing additional non-melanoma skin cancer is significant, patients with a history of non-melanoma skin cancer do not associate this diagnosis with an increased risk for melanoma or other non-cutaneous malignancies, despite research showing increased risk of general cancer morbidity and mortality.[11] This calls attention to the need for better general health education and preventive interventions in this vulnerable population.
Limitations
The present review has some limitations that should be acknowledged. This review was limited to studies that were written in the English language, published in peer-reviewed journals and electronically available; therefore, the impact of publication bias on our findings cannot be precluded. The findings are based on respondents' self-reports that may have been affected by recall bias. This also could have introduced a social desirability bias into responses of sun protection practices.
Collectively, the literature can be characterized as lacking wide generalizability. This is in part due to the fairly low methodological quality; for example, the majority of the reviewed studies used convenience sampling strategies recruited from a single site. Furthermore, the studies that reported information on ethnicity involved a vast majority of Caucasians. One of the obvious reasons for studies involving a large proportion of Caucasians is the high rate of skin cancer among this population group.[26] However, there is growing evidence to suggest that the incidence rate of skin cancer diagnosis among non-Caucasian populations is increasing.[27],[28],[29] Consequently, future studies should focus on identifying strategies to recruit more diverse populations to capture racial and ethnic disparities in relation to sun protection attitudes and behaviors among non-melanoma skin cancer patients.
Skin cancer continues to increase worldwide, yet existing literature is based mostly on western nations, suggesting research from other regions is warranted. Doing so may strengthen how the health community responds to one of the most commonly diagnosed cancers in the US and across the globe.
The instruments used also constrain the external validity. There is a lack of valid and reliable instruments that can be used to increase the rigor of this work. In addition, due to the variety of ways in which sun protection was assessed in earlier studies, a comparison between populations cannot be carried out. Researchers should be encouraged to take standardized scales into consideration to allow uniformity in the measurement of preventive behaviors across the literature in this domain.
The current literature lacks rigor in terms of research design. Because of the cross-sectional design of most of the included studies, a possible temporality of the associations cannot be established. Prospective studies are warranted to provide a level of compelling evidence in order to assert causality or directionality between explanatory variables and skin cancer prevention behaviors among patients with skin malignancies.
Conclusions
The studies included in this review highlight the need for continuing research on the prevalence of UV radiation exposure and sun protection behaviors in people diagnosed with non-melanoma skin cancer. The findings, although limited, strongly suggest that intervention programs for non-melanoma skin cancer survivors should focus on increasing knowledge and the perceived risk of skin cancer. At the same time, barriers that prevent individuals from engaging in sun-safe practices should be minimized. Health care professionals should be encouraged to provide education to patients regarding skin cancer risk and primary prevention strategies (e.g., wearing protective clothing, using sunscreen, and staying in shade). Educational programs should include family members to influence patients' engagement in sun protection behaviors. In addition, free skin cancer screening programs at the community level should be implemented to prevent and identify skin cancer during early stages. Finally, the medical community should work in partnership with mass media to raise awareness about the benefits of sun protection and consequences of overexposure to the UV radiation exposure.
Further studies are required with the non-melanoma skin cancer population to draw firm conclusions regarding the associations that may correlate with sun protection behaviors. A theoretical approach would be beneficial to conceptualize sun protection behaviors among this at-risk group. Hopefully, these efforts will guide future interventions, as well as provide a greater understanding of potential factors, related to sun protection behavior change.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Skin Cancer Foundation. Cancer Facts and Figures. Available from: http://www.skincancer.org/skin-cancer-information/skin-cancer-facts. [Last accessed on 2014 Nov 22].
[Google Scholar]
|
| 2. |
Rittié L, Kansra S, Stoll SW, Li Y, Gudjonsson JE, Shao Y, et al. Differential ErbB1 signaling in squamous cell versus basal cell carcinoma of the skin. Am J Pathol 2007;170:2089-99.
[Google Scholar]
|
| 3. |
Lucas RM, McMichael AJ, Armstrong BK, Smith WT. Estimating the global disease burden due to ultraviolet radiation exposure. Int J Epidemiol 2008;37:654-67.
[Google Scholar]
|
| 4. |
Vernez D, Milon A, Vuilleumier L, Bulliard JL, Koechlin A, Boniol M, et al. A general model to predict individual exposure to solar UV by using ambient irradiance data. J Expo Sci Environ Epidemiol 2015;25:113-8.
[Google Scholar]
|
| 5. |
Trakatelli M, Ulrich C, del Marmol V, Euvrard S, Stockfleth E, Abeni D. Epidemiology of nonmelanoma skin cancer (NMSC) in Europe: Accurate and comparable data are needed for effective public health monitoring and interventions. Br J Dermatol 2007;156 Suppl 3:1-7.
[Google Scholar]
|
| 6. |
Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol 2012;166:1069-80.
[Google Scholar]
|
| 7. |
American Cancer Society. Available from: http://www.cancer.org/acs/groups/content/@research/documents/webcontent/acspc-042151.pdf. [Last accessed on 2014 Nov 22].
[Google Scholar]
|
| 8. |
Rogers HW, Weinstock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol 2010;146:283-7.
[Google Scholar]
|
| 9. |
Guy GP Jr, Machlin SR, Ekwueme DU, Yabroff KR. Prevalence and costs of skin cancer treatment in the U.S 2002-2006 and 2007-2011. Am J Prev Med 2015;48:183-7.
[Google Scholar]
|
| 10. |
Marcil I, Stern RS. Risk of developing a subsequent nonmelanoma skin cancer in patients with a history of nonmelanoma skin cancer: A critical review of the literature and meta-analysis. Arch Dermatol 2000;136:1524-30.
[Google Scholar]
|
| 11. |
Rhee JS, Davis-Malesevich M, Logan BR, Neuburg M, Burzynski M, Nattinger AB. Behavior modification and risk perception in patients with nonmelanoma skin cancer. WMJ 2008;107:62-8.
[Google Scholar]
|
| 12. |
Koh HK, Geller AC, Miller DR, Grossbart TA, Lew RA. Prevention and early detection strategies for melanoma and skin cancer. Current status. Arch Dermatol 1996;132:436-43.
[Google Scholar]
|
| 13. |
American Academy of Dermatology. Available from: https://www.aad.org/spot-skin-cancer/understanding-skin-cancer/how-do-i-prevent-skin-cancer. [Last accessed on 2014 Nov 22].
[Google Scholar]
|
| 14. |
Harth Y, Ulman Y, Peled I, Friedman-Birnbaum R. Sun protection and sunscreen use after surgical treatment of basal cell carcinoma. Photodermatol Photoimmunol Photomed 1995;11:140-2.
[Google Scholar]
|
| 15. |
Maser E, Berg D, Solish N. Changes in patient perception and behavior following Mohs micrographic surgery. J Cutan Med Surg 2001;5:14-7.
[Google Scholar]
|
| 16. |
Rhee JS, Matthews BA, Neuburg M, Smith TL, Burzynski M, Nattinger AB. Quality of life and sun-protective behavior in patients with skin cancer. Arch Otolaryngol Head Neck Surg 2004;130:141-6.
[Google Scholar]
|
| 17. |
Rhee JS, Loberiza FR, Matthews BA, Neuburg M, Smith TL, Burzynski M. Quality of life assessment in nonmelanoma cervicofacial skin cancer. Laryngoscope 2003;113:215-20.
[Google Scholar]
|
| 18. |
Woolley T, Buettner PG, Lowe J. Predictors of sun protection in northern Australian men with a history of nonmelanoma skin cancer. Prev Med 2004;39:300-7.
[Google Scholar]
|
| 19. |
Renzi C, Mastroeni S, Mannooranparampil TJ, Passarelli F, Caggiati A, Pasquini P. Skin cancer knowledge and preventive behaviors among patients with a recent history of cutaneous squamous cell carcinoma. Dermatology 2008;217:74-80.
[Google Scholar]
|
| 20. |
Goldenberg A, Nguyen BT, Jiang SI. Knowledge, understanding, and use of preventive strategies against nonmelanoma skin cancer in healthy and immunosuppressed individuals undergoing Mohs surgery. Dermatol Surg 2014;40:93-100.
[Google Scholar]
|
| 21. |
Cartmel B, Ferrucci LM, Spain P, Bale AE, Pagoto SL, Leffell DJ, et al. Indoor tanning and tanning dependence in young people after a diagnosis of basal cell carcinoma. JAMA Dermatol 2013;149:1110-1.
[Google Scholar]
|
| 22. |
Hillhouse JJ, Turrisi R, Kastner M. Modeling tanning salon behavioral tendencies using appearance motivation, self-monitoring and the theory of planned behavior. Health Educ Res 2000;15:405-14.
[Google Scholar]
|
| 23. |
Pagoto SL, Schneider KL, Oleski J, Bodenlos JS, Merriam P, Ma Y. Design and methods for a cluster randomized trial of the sunless study: A skin cancer prevention intervention promoting sunless tanning among beach visitors. BMC Public Health 2009;9:50.
[Google Scholar]
|
| 24. |
Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: John Wiley and Sons; 2008. p. 45-65.
[Google Scholar]
|
| 25. |
Stanton WR, Janda M, Baade PD, Anderson P. Primary prevention of skin cancer: A review of sun protection in Australia and internationally. Health Promot Int 2004;19:369-78.
[Google Scholar]
|
| 26. |
Leiter U, Garbe C. Epidemiology of melanoma and nonmelanoma skin cancer – the role of sunlight. Adv Exp Med Biol 2008;624:89-103.
[Google Scholar]
|
| 27. |
Hu S, Parmet Y, Allen G, Parker DF, Ma F, Rouhani P, et al. Disparity in melanoma: A trend analysis of melanoma incidence and stage at diagnosis among whites, Hispanics, and blacks in Florida. Arch Dermatol 2009;145:1369-74.
[Google Scholar]
|
| 28. |
Skin Cancer Foundation. Cancer Facts and Figures. Available from: http://www.skincancer.org/publications/sun-and-skin-news/winter-2013-30-4/soar. [Last accessed on 2014 Nov 22].
[Google Scholar]
|
| 29. |
McLeod MP, Ferris KM, Choudhary S, Alqubaisy Y, Shiman M, Loring-Warsch J, et al. Contralateral distribution of nonmelanoma skin cancer between older Hispanic/Latino and non-Hispanic/non-Latino individuals. Br J Dermatol 2013;168:65-73.
[Google Scholar]
|
Fulltext Views
2,048
PDF downloads
830





