Translate this page into:
Survey of dermatologists' phototherapy practices for vitiligo
2 Vitiligo Research Chair, College of Medicine, King Saud University, Riyadh, Saudi Arabia
3 Department of Dermatology and Pediatric Dermatology, Saint Andr� and Pellegrin Hospitals, Bordeaux University Hospitals, France
Correspondence Address:
Khalid M AlGhamdi
Dermatology Department, Director, Vitiligo Research Chair, College of Medicine, King Saud University, P.O. Box 240997, Riyadh 11322
Saudi Arabia
| How to cite this article: AlGhamdi KM, Khurram H, Ta�eb A. Survey of dermatologists' phototherapy practices for vitiligo. Indian J Dermatol Venereol Leprol 2012;78:74-81 |
Abstract
Background: The details of phototherapy practices for vitiligo have been rarely studied. Objective: To explore the details of phototherapy practices for vitiligo among dermatologists. Methods: A self-administered questionnaire about the details of phototherapy practices for vitiligo was distributed to all dermatologists attending a national general dermatology conference in Riyadh, Saudi Arabia, in 2008. Results: Questionnaires were returned by 121 of 140 participants (response rate = 86.4%). The mean age of the respondents was 39.34 9.7 years, and 65% were males. One hundred eight of 110 (98.2%) respondents provided phototherapy to their vitiligo patients. The mean number of vitiligo patients who underwent phototherapy each week per dermatologist's office was 18 2.26. Narrowband ultraviolet B (NB-UVB) was the most common modality chosen to treat generalized vitiligo (84%). Excimer laser was the most common modality used to treat focal and segmental vitiligo (53% and 39%, respectively). Sixty-eight percent of dermatologists administered a fixed starting dose of NB-UVB to all patients, whereas 31% used the minimal erythema dose as a guide. Fifty percent reported that NB-UVB resulted in better color matching with the surrounding skin. Thirty-seven percent favored NB-UVB over psoralen + ultraviolet A for a faster response, and 31% preferred NB-UVB for a pigmentation that is more durable. Forty-seven percent (50/106) of the respondents limited the number of phototherapy sessions to reduce the risks of skin cancer. However, no respondent reported any skin cancer incidence in phototherapy-treated vitiligo patients. Conclusion: There is a need for phototherapy guidelines for the treatment of vitiligo in patients with skin of color.Introduction
Vitiligo is an acquired cutaneous depigmentation disorder that affects approximately 1 to 2% of the world′s population, with no predilection for age, gender, or ethnic background. [1] Vitiligo is difficult to treat, although various nonsurgical and surgical treatment modalities have been mentioned in the literature. [2] The progressive depigmentation of the skin that characterizes vitiligo is associated with a loss of melanocytes from the basal layer of the epidermis. [3]
Narrowband ultraviolet B (NB-UVB) therapy is now a well-established and recommended phototherapy for generalized vitiligo, even in pregnant women and children, because of its high safety profile. [4],[5],[6] As with many other treatments, psoralen + ultraviolet A (PUVA) and NB-UVB therapies generally result in good repigmentation on the trunk and proximal aspects of limbs but less frequently improve pigmentation on the hands and feet. [6]
We sought to explore the details of current practice in phototherapy treatment for vitiligo among dermatologists in Saudi Arabia. No regional or worldwide study has been conducted to explore the details of phototherapy use in the management of vitiligo. Previous surveys either evaluated phototherapy for vitiligo in general as a part of the overall management of vitiligo, [7] or examined phototherapy practices for skin disorders in general. [8]
Methods
A cross-sectional survey was distributed to all participants at a national general dermatology conference in Riyadh, Saudi Arabia, on November 9-13, 2008. Participants were general dermatologists. A questionnaire was distributed to all 140 dermatologists attending the conference. The questionnaire contained 25 questions, including basic demographic variables (gender, age, and years of practice). The dermatologists were also asked about the average weekly number of vitiligo patients with whom they used phototherapy and the percentages of different phototherapy modalities employed. The questions further addressed treatment options, dosages, and the management of adverse effects.
The dermatologists completed the questionnaires on site at the conference. A scale format (always, frequently, sometimes, rarely, never) was used to assess the dermatologists′ practices regarding calculating cumulative doses and protecting body areas during phototherapy. Their preferences for different treatment modalities in vitiligo were explored. They were asked about the method they use most frequently to determine starting doses for PUVA and NB-UVB in vitiligo patients. Additionally, we requested that they indicate their first choice of phototherapy modality for treating the different types of vitiligo. Their views on the efficacy of PUVA vs NB-UVB were also probed. The percentage of vitiligo patients who suffered from side effects, such as burns, pruritus and PUVA lentigines, and the dermatologists′ immediate treatment recommendations for side effects, were examined. All data were analyzed using the Statistical Package for Social Sciences (SPSS) software, version 16, and P values ≤0.05 were considered statistically significant. Means, medians, and standard deviations were utilized to summarize the responses as measures of central tendency. Associations between baseline variables and outcomes were determined using Pearson′s Chi-square test.
This study was approved by the Research Ethics Committee at King Saud University, Riyadh, Saudi Arabia.
Results
Demographic characteristics of the respondents
Among the 140 dermatologists attending the conference, 121 returned the questionnaires (response rate, 86.4%). Eleven questionnaires were excluded because they were more than 50% incomplete. A total of 110 questionnaires were analyzed. Of these, 108 (98.2%) indicated that they provided phototherapy to their vitiligo patients. The mean age of the respondents was 39.34 ± 9.7 years. Sixty-five percent (69/106) were males. Consultants comprised 43/108 (40%), while the rest of the respondents were specialists or residents in training (28.7% and 31.5%, respectively). University and government hospital-based practices employed 72.2% of the respondents, whereas 15.7% were private dermatologists. The mean number of years′ experience in dermatology was 11.4 ± 8.4 years. The respondents had a mean of 18 ± 2.26 vitiligo patients undergoing phototherapy each week.
Preferred phototherapy modalities
Overall, NB-UVB was the most commonly used light modality for vitiligo (54%); 2.2% used broadband UVB (BB-UVB), 11% used oral PUVA, and 18% used topical (8-MOP) PUVA. Fifteen percent of the respondents had used excimer laser to treat vitiligo.
When asked about their first-choice phototherapy method for the treatment of focal vitiligo, nearly half of the respondents (52.8%, 47/89) preferred excimer laser, 6% used NB-UVB, and none used BB-UVB. For segmental vitiligo, 39.3% (33/84) preferred excimer laser, 28.6% used topical PUVA, and 27% used NB-UVB. The most common phototherapy modality used for generalized vitiligo was NB-UVB, which was selected by 83.7% of the respondents (87/104) [Figure - 1].
 |
| Figure 1: First-choice phototherapy for different types of vitiligo among a cohort of 110 dermatologists |
The most common treatment frequency for all forms of phototherapy was three times per week. NB-UVB was practiced three times a week by 74.2% of the dermatologists. A twice-weekly regimen was used by 26% for oral PUVA and by 25% for topical PUVA.
Dosage of phototherapy
Sixty-eight percent of dermatologists gave a fixed starting dose of NB-UVB to all patients, whereas 31% based the starting dose on the UVB-determined minimal erythema dose (MED). The same was true for oral PUVA treatment; 66% of dermatologists began treatment at the preset fixed dose. For topical PUVA, 54% chose the dosage according to the patient′s skin phototype, and the other 46% used a fixed protocol for all patients.
Dermatologists′ responses regarding calculating cumulative doses for different modalities were variable. For PUVA, 50% (25/50) always calculated the cumulative dose. Only 2% never calculated the cumulative dose for PUVA. For NB-UVB, 76.7% reported always calculating the cumulative dose. Three percent indicated that they never estimated the NB-UVB cumulative dose.
Photoprotection
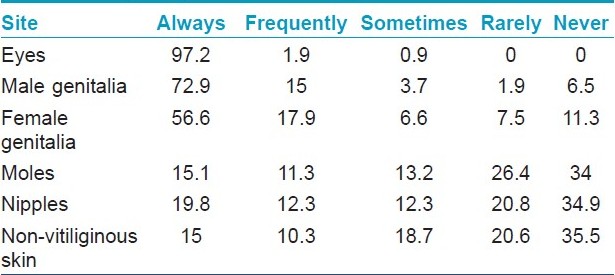
The majority of dermatologists recognized the importance of photoprotection during phototherapy treatments. Photoprotection for the eyes was always provided by 97% of the respondents (104/107). Protective shields were always used for the male genitalia by 88% and for the female genitalia by 74.5% of the respondents. Only 15% used photoprotection for moles. Thirty-five percent did not protect nipples during phototherapy. Fifteen percent (16/107) always used protective covers for non-vitiliginous skin, whereas the remainder of the dermatologists never used protective shields for normal skin [Table - 1].
Comparisons of psoralen + ultraviolet A and narrowband ultraviolet B
Half of the respondents preferred NB-UVB for better color matching with the surrounding skin, whereas 45.3% were unable to judge which modality was more effective. For stable or durable repigmentation, 31% (33/104) preferred NB-UVB, whereas 16% favored PUVA. For faster repigmentation, 37.3% preferred NB-UVB, 23.5% preferred PUVA, and 39% could not evaluate this effect for both modalities. NB-UVB was regarded as the more effective therapy by 43.7% of dermatologists. Half of the respondents considered local NB-UVB treatment for acral vitiligo ineffective, and only 26% believed it was effective for the treatment of local NB-UVB of the hands and feet.
Treatment duration
Regarding the phototherapy treatment duration, the approaches were variable. After an average of 26 ± 1.8 sessions of PUVA without repigmentation, the dermatologists considered it ineffective and terminated the treatment. NB-UVB was also stopped after 34.3 ± 2.5 sessions without response. Forty-seven percent of the respondents (50/106) said that they would limit the number of phototherapy sessions to reduce the risks of skin cancer, whereas 52.8% were not concerned about skin cancer risks with extended sessions. According to our survey, none of the dermatologists reported seeing any vitiligo patients develop skin cancer after phototherapy.
Side effects and their management
The most frequent side effects described were mild burns (16.5% ± 2.1) and pruritus (15.5% ± 1.7). A smaller number reported moderate (4.3%) or severe burns (1.7%). PUVA lentigines had been seen in 1.1% ± 3.5 of patients.
For severe accidental UVB overdose, immediate treatments practiced by respondents included topical steroids (93.5%), cool or wet compresses (88%), emollients (81%), wet dressings, and oral paracetamol (63%). Forty-five percent of the respondents recommended oral nonsteroidal anti-inflammatory drugs. Systemic corticosteroids were prescribed by 54.4%. Almost all dermatologists recommended different combinations of these treatment options.
Discussion
Several variations exist in the approaches to and practice of phototherapy for vitiligo, including the types of phototherapy used for different types of vitiligo, dosage schedules, photoprotection, comparisons of different modalities, and dermatologists′ management of adverse events.
Phototherapy is a well-established treatment for vitiligo. It should generally be reserved for patients whose vitiligo cannot be adequately controlled with more conservative treatments, who have widespread vitiligo, or who have localized vitiligo with a significant impact on their quality of life. [9]
In Saudi Arabia, the majority of patients have access to government hospitals where phototherapy, especially NB-UVB, is widely available. Some government hospitals have excimer lasers, but they are mostly offered in private hospitals. Phototherapy is provided free of charge in government hospitals, and NB-UVB is considered to be inexpensive at private centers. The cost of NB-UVB in a private center is 30 Saudi riyals (about $8 US) per session; however, excimer laser is more expensive (100-200 Saudi riyals per session, equivalent to 27 to 54 US$).
In Saudis, the skin phototype is Type IV to V, and there are no specific recommendations in the published guidelines for patients with skin of color. [10] Therefore, for our own local practice, we need to take this ignorant part into account for production of guidelines in Saudi Arabia.
The survey responses showed that phototherapy is a common and important treatment option used by most of our Saudi dermatologists (98.2%). The results are of great significance here because most of these general dermatologists see 18 ± 2.26 vitiligo patients per week.
The use of NB-UVB phototherapy to treat vitiligo was reported for the first time by Westerhof and Nieuweboer-Krobotova in 1997. [11] Subsequently, several studies confirmed the efficacy of this therapy for the treatment of vitiligo. [12],[13] NB-UVB is one of the most efficacious treatments, with an optimum side-effect profile and an average response rate of 62% demonstrated in one study; however, 6 to 12 months of treatment are needed before optimum results are achieved. [5]
Overall, our dermatologists used NB-UVB more frequently than PUVA or BB-UVB. This response was expected, as the efficacy of NB-UVB in treating vitiligo has been clearly shown in recent clinical trials. PUVA is a less-used modality for all types of vitiligo, potentially reflecting the published data that indicate a decreased effectiveness and an increased risk of PUVA-associated malignancies. [14],[15],[16],[17],[18] NB-UVB has the advantage of
being more acceptable for patients than PUVA because they do not need to take oral medication before exposure to the radiation or wear protective sunglasses afterwards. [19] Moreover, NB-UVB proved to be equal or superior to oral PUVA in treating vitiligo. [10],[20]
Phototherapy with BB-UVB appears less effective than PUVA and is used less frequently. [11] NB-UVB became widely available in 1991 and appeared to be more effective for the treatment of vitiligo than the BB-UVB that it replaced. An arbitrary limit of 200 NB-UVB treatments for vitiligo has been suggested. [10]
Most of our respondents favored NB-UVB over PUVA. The majority of them said that NB-UVB produced better repigmentation and that the repigmentation achieved was cosmetically acceptable and matched the surrounding normal skin, in contrast to the results of PUVA therapy. This finding is supported by a study demonstrating that NB-UVB therapy is superior to oral PUVA therapy. In that study, 25 patients with vitiligo were treated with PUVA, and 25 were treated with NB-UVB. [10] NB-UVB appeared to provide a better response than did PUVA. At the end of therapy, 64% of the NB-UVB patients had a 50% or greater reduction in the body surface area affected, compared with 36% of the PUVA group. The color match of the repigmented skin was excellent for all patients in the NB-UVB group but for only 44% of those in the PUVA group. [10]
Our recently published study [7] concerning the general management of vitiligo showed that the most commonly used phototherapy was NB-UVB. NB-UVB was used to treat generalized vitiligo in 36% of children and 40% of adults. The use of oral PUVA was limited (8% for generalized vitiligo in adults), and topical PUVA was also reported to be useful by a few respondents (1 to 8% for different types of vitiligo).
Excimer laser, a relatively new vitiligo treatment modality with wavelengths of 308 and 311 nm, was used by some of our respondents to treat segmental and focal vitiligo. Its main advantage is the ability to apply targeted treatment only to the depigmented sites, which makes it a good option for segmental and focal vitiligo. In two studies, the excimer laser achieved a good to very good response in 30 to 75% of patients, especially for vitiligo on the face, without any serious side effects. [21],[22],[23] In our survey, excimer laser was the most common phototherapy modality used for focal and segmental vitiligo.
The most common treatment frequency for all forms of phototherapy in our study was three times per week. NB-UVB was provided three times a week by 74.2% of dermatologists. This is consistent with the 2009 British guidelines for vitiligo management. [10]
The published data for patients with psoriasis can likely be applied to vitiligo. A randomized, observer-blinded trial of twice- vs. three-times-weekly NB-UVB therapy for psoriasis reported that for the majority of the population with skin phototypes I to III, three-times-weekly NB-UVB clears psoriasis significantly faster than twice-weekly treatment. [18]
However, there are no published comparative studies of different weekly frequencies of phototherapy for vitiligo.
The dermatologists predominantly started all patients at the fixed starting dose of NB-UVB, whereas 31% reported that they base the starting dose on the UVB-determined MED. For topical PUVA, 54% use the Fitzpatrick skin phototype of the patient to determine the initial phototherapy dose. Fifty percent always calculate the cumulative doses for PUVA, and 76% always calculate the cumulative doses for UVB.
UVB-determined MED has significant therapeutic importance when applied to protocols that base the dose of UVB on MED. The measurement of MED actually determines the dose-response to the UVB light delivered. The average NB-UVB MED for type I skin is reported as 400 mJ/cm 2 . [13]
Seventy percent of the MED value is commonly used for the first treatment; thereafter, therapy is administered two or three times per week with 20% increase each week, depending on the local response and the skin-type tolerance. Another approach involves the use of a standard starting dose (280 mJ/cm 2 ) with stepwise increase (usually 20%) depending on the patient′s erythema response. [12]
The 2009 British guidelines for vitiligo management suggest that treatment regimens for patients with skin types I to III should not exceed 200 treatments with NB-UVB or 150 treatments with PUVA. The evidence is deficient to set an upper limit for NB-UVB or PUVA for patients with skin types IV to VI. [11]
Only 50% of the dermatologists always calculated the cumulative PUVA dose. However, 50% do not bother about it. Therefore, the issue of awareness of phototherapy-induced skin cancer risk needs to be addressed.
Based on our earlier survey concerning the general management of vitiligo, [7] it was clear that the phototherapy treatment duration was restricted to less than one year by 46% of respondents due to the fear of increasing the patients′ risks of developing skin cancer. To date, there have been no reports of skin cancer in Saudi vitiligo patients treated with phototherapy, as confirmed by the results of the present survey. Dermatologists with a mean work experience duration of more than 10 years and an average of 18 vitiligo patients per week did not observe any skin cancer in their phototherapy-treated vitiligo patients. This is very reassuring for dermatologists who use phototherapy to treat their vitiligo patients.
Only a very few cases of phototherapy-induced (or -related) skin cancer have been reported in vitiligo patients. [24],[25] Interestingly, Schallreuter et al.[26] reported the absence of an increased risk of sun-induced damage and skin cancer in a study of 136 sun-exposed Caucasian patients with vitiligo.
Hexsel et al.[27] reported the incidence of nonmelanoma skin cancer (NMSC) in a cohort of 477 patients with vitiligo. NMSC was found on sun-exposed sites of Caucasian patients with vitiligo in both vitiligo-affected and unaffected skin. Two of the six cancers arose in vitiliginous skin; the other four were found in skin containing melanocytes. The authors concluded that NMSC is as common or more so in patients with vitiligo than in the white population at large.
Nordlund [28] later challenged this finding by reporting that there are few reports of skin cancer in vitiliginous skin. Many points described by Hexsel were disregarded, and none of the 91 nonwhite patients presented with NMSC in his study.
All vitiligo skin is considered to be of the Fitzpatrick skin type I. This indicates that the depigmented skin of all ethnic groups should be equally susceptible to skin cancer if melanin is the major determinant. These six cancers occurred only in the white people. Only two of these cancers occurred on true vitiliginous skin; the others were present on normal skin. Nordlund further commented that one would predict the converse to be true: that vitiliginous skin is more prone to skin cancer. The prevalence rates calculated by Hexsel et al. for basal cell carcinoma should be only one in four for depigmented skin and one in two for squamous-cell carcinomas (SCCs); this is lower than the rates anticipated for depigmented skin compared with normal skin. [27],[28]
Vitiliginous skin is less likely to be sun damaged than normal skin. [26] There is a scarcity of reports of skin cancers in depigmented, vitiliginous skin treated with all modalities, including PUVA. Sun exposure is a known carcinogen in patients with psoriasis, [29] but it has been the treatment of choice for vitiligo for many decades.
The cause of the low incidence of skin cancers in vitiligo patients remains unclear. One study has demonstrated the overexpression of a functional wild-type p53 protein in both the depigmented and the normal-pigmented epidermis of patients with vitiligo compared that of healthy controls. Surprisingly, long-term NB-UVB (311 nm) treatment does not alter this expression. This increase in epidermal p53 in vitiligo supports the hypothesis of a low incidence of actinic damage and basal cell carcinoma and SCC in vitiligo patients. [30]
To the best of our knowledge, none of the published studies has demonstrated an increase in skin cancer risk with UVB phototherapy for psoriasis. Based on the data that are currently available, even for fair-skinned Caucasians, no precise limit to the number of allowable UVB treatments can be defined. However, it is recommended that dermatologists continue the current practice of shielding the patients′ genitals during UVB phototherapy. Exposure should be even less of a concern for darker-skinned non-Caucasians whose skin is less prone to UV damage. The relative carcinogenicity of NB-UVB vs BB-UVB phototherapy remains to be determined. [31]
Eye protection is always used during phototherapy. The appropriate sunglasses must filter out more than 99% of the UV light that penetrates the cornea. [32] Ninety-seven percent of the present respondents adhered to this guideline. Only 6.5% of our respondents said that they did not protect the male genitalia during phototherapy. The strongly dose-dependent increase in the risk for genital tumors associated with PUVA and UVB radiation exposure is well reported, making it prudent for men to use genital protection whenever they are exposed to PUVA or NB-UVB. [33],[34]
The most common side effects reported by our dermatologists were mild erythema, burning, and pruritus. The approaches used for the management of severe accidental UVB exposure are markedly variable. The majority of dermatologists treat overexposure with topical steroids, emollients, and cool or wet compresses. This treatment strategy is supported by recent management recommendations, which are largely supportive and include the use of emollients, cool compresses, and ample pain control. [20] Nearly half of our dermatologists (45%) suggested the use of NSAIDs within 24 hours of side effect. NSAIDs have been shown to partially prevent UVB-induced erythema, but they are not effective when given in the late phase of an injury. [35]
Phototherapy is used by a large number of dermatologists for all types of vitiligo. The present survey has identified variations in phototherapy practices for vitiligo in Saudi Arabia. To the best of our knowledge, this is the first detailed report concerning phototherapy practices in vitiligo treatment among dermatologists worldwide. We demonstrate some clear differences in vitiligo management in dark skin compared to European skin. A limitation of this study is the use of a convenience sample, as dermatologists attending a scientific conference might not be very representative of all dermatologists in the country. However, due to the lack of postal addresses or a database for dermatologists in this country, the distribution of questionnaires at a national conference was probably the best available option.
The good sample size is a strength of this study. However, it is true that it is a spot survey and more or less individual dependent. But we are not looking for therapeutic comparison, rather to see the dermatologists′ perception about them. The respondents of survey are relatively representatives of our dermatologist community, because they belong to different age groups, different practicing groups, for example, residents, specialists, and consultants and have different levels of experience.
More studies are needed to compare phototherapy practices for vitiligo in other countries and worldwide.
Acknowledgements
The authors would like to express their gratitude to the following dermatologists who helped to distribute and collect questionnaires: Dr. Sahar AlNatour, Dr. Khalid AlAttas, Dr. Muhammad Fatani, Dr. Essam AlSobyani, Dr. Khalid Bahmdan, Dr. Saleh AlGhamdi, Dr. Abdulatif AlZolibani, and Dr. Muhammad AlDuribi.
| 1. |
Njoo MD, Spuls PI, Bos JD, Westerhof W, Bossuyt PM. Nonsurgical repigmentation therapies in vitiligo: Meta-analysis of the literature. Arch Dermatol 1998;134:1532-40.
[Google Scholar]
|
| 2. |
Rusfianti M, Wirohadidjodjo WY. Dermatosurgical techniques for repigmentation of vitiligo. Int J Dermatol 2006;45:411-7.
[Google Scholar]
|
| 3. |
Mahmoud BH, Hexsel CL, Hamzavi IH. An update on new and emerging options for the treatment of vitiligo. Skin Therapy Lett 2008;13:1-6.
[Google Scholar]
|
| 4. |
Hercogova J, Buggiani G, Prignano F, Lotti T. A rational approach to the treatment of vitiligo and other hypomelanoses: Pigmentary disorders. Dermatol Clin 2007;25:383-92.
[Google Scholar]
|
| 5. |
Njoo MD, Bos JD, Westerhof W. Treatment of generalized vitiligo in children with narrow-band (TL-01) UVB radiation therapy. J Am Acad Dermatol 2000;42:245-53.
[Google Scholar]
|
| 6. |
Kanwar AJ, Dogra S. Narrow-band UVB for the treatment of generalized vitiligo in children. Clin Exp Dermatol 2005;30:332-6.
[Google Scholar]
|
| 7. |
AlGhamdi KM. A survey of vitiligo management among dermatologists in Saudi Arabia. J Eur Acad Dermatol Venereol 2009;11:1282-8.
[Google Scholar]
|
| 8. |
Huynh NT, Sullivan JR, Commens CA. Survey of phototherapy practice by dermatologists in Australia. Australas J Dermatol 2002;43:179-85.
[Google Scholar]
|
| 9. |
Taieb A, Picardo M. The definition and assessment of vitiligo: A consensus report of the Vitiligo European Task Force. Pigment Cell Res 2007;20:27-35.
[Google Scholar]
|
| 10. |
Gawkrodger DJ, Ormerod AD, Shaw L, Mauri-Sole I, Whitton ME, Watts MJ, et al. Guideline for the diagnosis and management of vitiligo. Br J Dermatol 2008;159:1051-76.
[Google Scholar]
|
| 11. |
Westerhof W, Nieuweboer-Krobotova L. Treatment of vitiligo with UVB radiation versus topical PUVA. Arch Dermatol 1997;133:1525-8.
[Google Scholar]
|
| 12. |
Scherschun L, Kim JJ, Lim HW. Narrow-band ultraviolet B is a useful and well-tolerated treatment for vitiligo. J Am Acad Dermatol 2001;44:999-1003.
[Google Scholar]
|
| 13. |
Tjioe M, Gerritsen MJ, Juhlin L, van de Kerkhof PC. Treatment of vitiligo vulgaris with narrow band UVB (311 nm) for one year and the effect of addition of folic acid and vitamin B12. Acta Derm Venereol 2002;82:369-72.
[Google Scholar]
|
| 14. |
Stern RS. The risk of melanoma in association with long-term exposure to PUVA. J Am Acad Dermatol 2001;44:755-61.
[Google Scholar]
|
| 15. |
Lindelöf B, Sigurgeirsson B. PUVA and cancer: A case control study. Br J Dermatol 1993;129:39-41.
[Google Scholar]
|
| 16. |
Bajdik CD, Gallagher RP, Astrakianakis G, Hill GB, Fincham S, McLean DI. Non-solar ultraviolet radiation and the risk of basal and squamous cell skin cancer. Br J Cancer 1996;73:1612-4.
[Google Scholar]
|
| 17. |
Stern RS. Genital tumors among men with psoriasis exposed to psoralens and ultraviolet A radiation (PUVA) and ultraviolet B radiation: the Photochemotherapy Follow-up Study. N Engl J Med 1990;322:1093-7.
[Google Scholar]
|
| 18. |
Cameron H, Dawe RS, Yule S, Murphy J, Ibbotson SH, Ferguson J. A randomised, observer-blinded trial of twice vs. three times weekly narrowband ultraviolet B photo�therapy for chronic plaque psoriasis. Br J Dermatol 2002;147:973-8.
[Google Scholar]
|
| 19. |
Parsad D, Kanwar AJ, Kumar B. Psoralen-ultraviolet A. vs. Narrow-band ultraviolet B phototherapy for the treatment of vitiligo. J Eur Acad Dermatol Venerol 2006;20:175-7.
[Google Scholar]
|
| 20. |
Yones SS, Palmer RA, Garibaldinos TM, Hawk JL. Randomized double-blind trial of treatment of vitiligo: Efficacy of psoralen-UVA therapy vs.Narrowband - UV-B Therapy. Arch Dermatol 2007;143:578-84.
[Google Scholar]
|
| 21. |
Esposito M, Soda R, Costanzo A, Chimenti S. Treatment of vitiligo with the 308 nm excimer laser. Clin Exp Dermatol 2004;29:133-7.
[Google Scholar]
|
| 22. |
Ostavari N, Passeron T, Zakaria W, Fontas E, Larouy JC, Blot JF, et al. Treatment of vitiligo by 308-nm excimer laser: An evaluation of variables affecting treatment response. Laser Surg Med 2004;35:152-6.
[Google Scholar]
|
| 23. |
Hadi S, Tinio P, Al Ghaithi K, Al-Qari H, Al-Helalat M, Lebwohl M, et al. Treatment of vitiligo using the 308 nm excimer laser. Photomed Laser Surg 2006;24:354-7.
[Google Scholar]
|
| 24. |
Park HS, Lee YS, Chun DK. Squamous cell carcinoma in vitiligo lesion after long-term PUVA therapy. J Eur Acad Dermatol Venereol 2003;17:578-80.
[Google Scholar]
|
| 25. |
Buckley DA, Rogers S. Multiple keratoses and squamous carcinoma after PUVA treatment of vitiligo. Clin Exp Dermatol 1996;21:43-5.
[Google Scholar]
|
| 26. |
Schallreuter KU, Tobin DJ, Panske A. Decreased photodamage and low incidence of non-melanoma skin cancer in 136 sun-exposed Caucasian patients with vitiligo. Dermatology 2002;204:194-201.
[Google Scholar]
|
| 27. |
Hexsel CL, Eide MJ, Johnson CC, Krajenta R, Jacobsen G, Hamzavi I, et al. Incidence of nonmelanoma skin cancer in a cohort of patients with vitiligo. J Am Acad Dermatol 2009;60:929-33.
[Google Scholar]
|
| 28. |
Nordlund JJ. Nonmelanoma skin cancer in vitiligo patients. J Am Acad Dermatol 2009;61:1080-1.
[Google Scholar]
|
| 29. |
Seidl H, Kreimer-Erlacher H, Bäck B, Soyer HP, Höfler G, Kerl H, et al. Ultraviolet exposure as the main initiator of p53 mutations in basal cell carcinomas from psoralen and ultraviolet A-treated patients with psoriasis. J Invest Dermatol 2001;117:365-70.
[Google Scholar]
|
| 30. |
Schallreuter KU, Behrens-Williams S, Khaliq TP, Picksley SM, Peters EM, Marles LK, et al. Increased epidermal functioning wild-type p53 expression in vitiligo. Exp Dermatol 2003;12:268-77.
[Google Scholar]
|
| 31. |
Lee E, Koo J, Berger T. UVB phototherapy and skin cancer risk. Int J Dermatol 2005;44:355 -60.
[Google Scholar]
|
| 32. |
Lerman S, Van Vorhees A. Cutaneous and ocular ramifications of ultraviolet radiation. Dermatol Clin 1992;10:483-504.
[Google Scholar]
|
| 33. |
Stern RS. Genital tumors among men with psoriasis exposed to psoralens and ultraviolet A radiation (PUVA) and ultraviolet B radiation: the Photochemotherapy- Follow-up Study. N Engl J Med 1990;322:1093-7.
[Google Scholar]
|
| 34. |
Stern RS, Bagheri S, Nichols K. The persistent risk of genital tumors among men treated with psoralen + UVA (PUVA) for psoriasis. J Am Acad Dermatol 2002;47:33-9.
[Google Scholar]
|
| 35. |
Ibbotson SH, Diffey BL, Farr PM. The effect of topical indomethacin on ultraviolet-radiation-induced erythema. Br J Dermatol 1996;135:523-7.
[Google Scholar]
|
Fulltext Views
4,495
PDF downloads
3,059





