Translate this page into:
Symmetric plaques on the inguinoscrotal folds: An unusual pattern of lichen sclerosus post-penile amputation and perineal urethrostomy
Corresponding author: Dr. Vishal Gupta, Department of Dermatology and Venereology, All India Institute of Medical Sciences, Delhi, India. doctor.vishalgupta@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mehta N, Manandhar K, Arava S, Gupta V. Symmetric plaques on the inguinoscrotal folds: An unusual pattern of lichen sclerosus post-penile amputation and perineal urethrostomy. Indian J Dermatol Venereol Leprol. 2025;91:244-5. doi: 10.25259/IJDVL_443_2023
Dear Editor,
A 71-year-old man presented with hypopigmented plaques and painful erosions on his scrotum and bilateral groins of six weeks duration. The pain worsened gradually, interfering with his walking and other routine activities. His past medical history was significant for penile carcinoma for which he underwent total penectomy with bilateral inguinal lymph node dissection and perineal urethrostomy one-and-half years back and local radiotherapy a year back. On examination, the patient had atrophic hypo-to-depigmented sclerosed plaques on the scrotal skin surrounding the urethrostomy opening and on bilateral inguinal folds symmetrically [Figure 1]. There were multiple erosions and punctate telangiectasias overlying the inguinal plaques. Perianal examination was within normal limits. On probing, the patient admitted to recurrent spillage and prolonged contact of urine at the affected areas during micturition. A Tzanck smear from the erosion did not show any acantholytic or multinucleated giant cells and polymerase chain reaction for herpes simplex virus 1 and 2 was negative. Skin biopsy from the scrotal and inguinal plaques showed marked upper dermal sclerosis, prominent papillary dermal oedema and an occasional necrotic keratinocyte in the irregularly acanthotic epidermis [Figure 2]. A diagnosis of lichen sclerosus was made on clinico-pathological correlation. Because of the erosive plaques and disabling pain, we chose to treat the patient initially with daily oral prednisolone instead of the usually recommended potent topical corticosteroids. There was good improvement in pain and healing of erosions with oral prednisolone 30 mg daily for 4 weeks, following which prednisolone dose was tapered and stopped over the next 6 weeks. The improvement was maintained with topical clobetasol propionate 0.05% cream.

- Atrophic hypo-to-depigmented sclerosed plaques on the scrotal skin surrounding the urethrostomy opening and on bilateral inguinal folds symmetrically with overlying erosions.
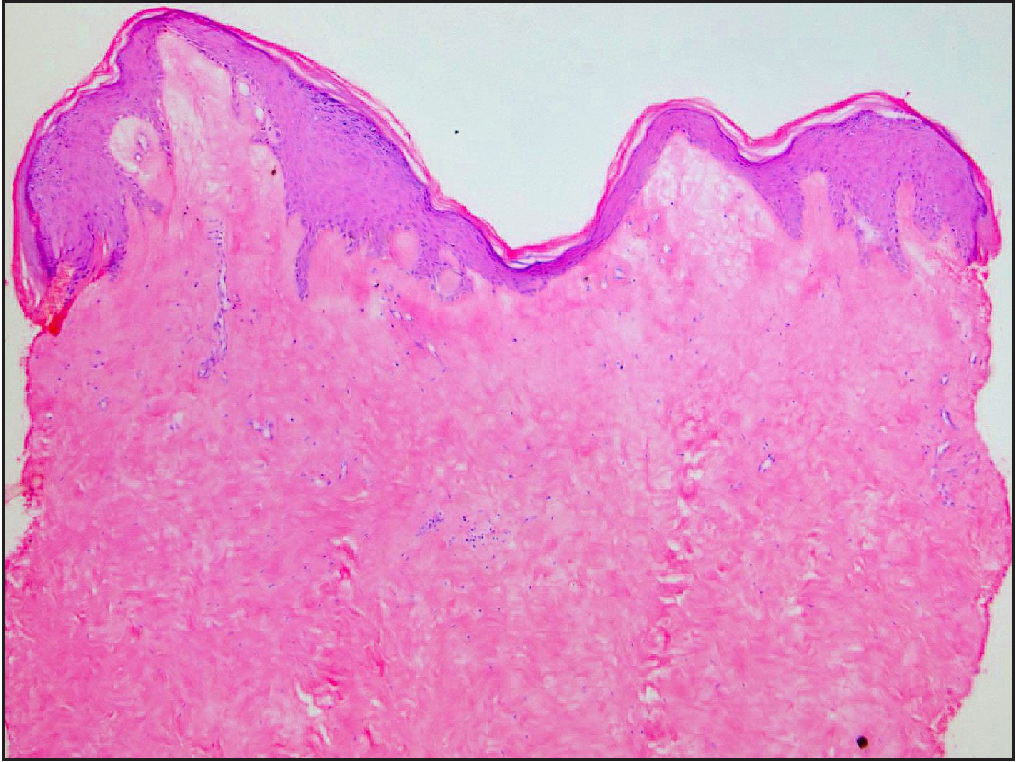
- Irregularly acanthotic epidermis, prominent papillary dermal edema and marked upper dermal sclerosis (Haematoxylin & eosin, 100x)
Lichen sclerosus is a chronic inflammatory sclerosing disorder, primarily affecting the anogenital region. Its pathogenesis is not clearly understood and multiple factors such as genetic susceptibility, autoimmunity, infectious agents, hormonal imbalance, trauma and exposure to urine have been implicated.1
Prolonged exposure of susceptible epithelium to urine under occlusion may play an important role in the pathogenesis of lichen sclerosus, suggested by its increased prevalence among uncircumcised men and in those with post-void dribbling of urine.2,3 Males with lichen sclerosis may have an abnormal urethral meatus or navicular fossa leading to urinary dribbling.4 The clinical pattern of genital lichen sclerosus also points towards a role of occlusion and prolonged contact with urine. Gupta et al, in their series of six patients with genital lichen sclerosus, reported preferential involvement of the occluded skin, between the prepuce and glans penis in males and opposed surface of the vulva in females with relative sparing of uncovered areas.5 Similarly, there are reports of lichen sclerosus plaques developing on the undersurface of the penile shaft and the opposing scrotal skin in cases of hypospadias and perineal urethrostomies.6 The unusual clinical pattern of lichen sclerosus in our patient lends further support to this theory. Penile amputation with perineal urethrostomy led to an altered pattern of urinary stream that coupled with post-micturition dribbling produced a ‘female pattern’ of lichen sclerosus on the scrotum; on the skin folds around the ‘new’ urethral opening, while prolonged exposure of spilled urine under occlusion led to lesions on inguinal folds.
Notably, no differences have been found in the urinary composition of men with genital lichen sclerosus and those without, suggesting that urine lacks a specific constituent and may rather act as a non-specific irritant.3 Recent studies have reported an alteration in the urinary microbiome of patients with genital lichen sclerosus which warrants further investigation.7 Interestingly, lichen sclerosus has been shown to develop on the peristomal skin of colostomy sites as well.8 This further points towards a non-specific irritant effect of a body fluid, be it urine, smegma, faeces or bowel mucus which gets enhanced by occlusion and results in lichen sclerosus in genetically predisposed individuals.
To conclude, we report an unusual clinical pattern of lichen sclerosus that re-emphasises the role of urine and occlusion in its pathogenesis.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Lichen sclerosus: A current landscape of autoimmune and genetic interplay. Diagnostics (Basel). 2022;12:3070.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical parameters in male genital lichen sclerosus: A case series of 329 patients. J Eur Acad Dermatol Venereol. 2012;26:730-7.
- [CrossRef] [PubMed] [Google Scholar]
- Urinary voiding symptomatology (micro-incontinence) in male genital lichen sclerosus. Acta Derm Venereol. 2013;93:246-8.
- [CrossRef] [PubMed] [Google Scholar]
- Male Genital Lichen Sclerosus. Indian J Dermatol. 2015;60:111-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lichen sclerosus: Role of occlusion of the genital skin in the pathogenesis. Indian J Dermatol Venereol Leprol. 2010;76:56-8.
- [CrossRef] [PubMed] [Google Scholar]
- Genital lichen sclerosus developing around “ectopic” urethral orifices supports the role of occlusion and urine in its pathogenesis. Int J STD AIDS. 2017;28:940-2.
- [CrossRef] [PubMed] [Google Scholar]
- Synchronous genitourinary lichen sclerosus signals a distinct urinary microbiome profile in men with urethral stricture disease. World J Urol. 2021;39:605-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Peristomal lichen sclerosus: The role of occlusion and urine exposure? Br J Dermatol. 2013;168:643-6.
- [CrossRef] [PubMed] [Google Scholar]





