Translate this page into:
Syndromic management in the control of sexually transmitted infections: Time for a relook
Correspondence Address:
Sumit Sen
CG-75, Sector 2, Salt Lake, Kolkata - 700 091, West Bengal
India
| How to cite this article: Sen S. Syndromic management in the control of sexually transmitted infections: Time for a relook. Indian J Dermatol Venereol Leprol 2013;79:816-817 |
Sir,
Syndromic management involves identifying a group of signs and symptoms in a patient and advocating treatment against the most common organism, which may be responsible. An effort to establish etiological diagnosis of the disease before instituting therapy is not required.
Vaginal discharge has been established as a syndrome. However, it fails to diagnose and treat chlamydia and gonorrhea though the two diseases may present with this manifestation. 60-70% of gonococcal and chlamydial infection are found to be asymptomatic. [1] Vaginal discharge usually visible during pregnancy or discharge seen in those on oral contraceptives is physiological, but often reported apprehending sexually transmitted disease (STD). Other women have the misconception that vaginal discharge is normal and do not report to the clinics despite suffering morbid STD. Discharge from the vagina is thus not a suitable entry point in syndromic management. Genital ulcer disease included as part of syndromic diagnosis and treatment is concerned only with the number of ulcers healed and not whether the disease is cured. [2]
Symptomatic patients do not habitually report to the STD clinics. Study among female sex workers reported only 12.7% women presenting with vaginal discharge. On examination, 51.7% were found to manifest discharge from vagina. [3] Asymptomatic patients of STD are disregarded in syndromic management. Researchers found 49% asymptomatic patients among 295 attendees in a STD clinic among responders with either genital ulcer disease or genital discharge. [4] STDs increase the spread of human immunodeficiency virus (HIV) 2-20 fold. Syndromic management fails to reduce the genital shedding of HIV and this has been demonstrated by testing genital secretions for the presence and concentrations of HIV. [5]
Overuse of antibiotics is another area of concern with syndromic management. Medicines are often prescribed unnecessarily to patients without disease. [6] Threat of antibiotic resistance looms large considering this perspective. The consistency of syndromic management has also not been validated and varies from place-to-place.
Syndromic management falls short of tackling the spiraling threat of spread of STD and with it HIV. Screening of patients, preferably laboratory based, among both high-risk and low-risk populations is the need of the hour. Behavior modification and strategies based on epidemiological data should be combined with health education. Use of mobile phones and the internet explosion can also be utilized to enhance low-cost, highly engaging and deeply permeating STD/HIV prevention and treatment support interpolations at an incomparable pace. [7] Perhaps the time has come to look closely and seriously assess aggressive strategies such as mass treatment. In comparison with syndromic management, single-round mass treatment had a greater short-term impact on HIV (36 vs. 30% over 2 years), but a smaller long-term impact (24 vs. 62% over 10 years). Mass treatment combined with improved treatment services led to a rapid and sustained fall in HIV incidence (57% over 2 years; 70% over 10 years). [6] The Piot-Fransen model of STD management depicting such mass treatment policy is based on data from underprivileged countries Uganda, Zaire, and Tanzania [Figure - 1]. All consenting individuals in the reproductive age group of 15-60 years can be offered single dose of azithromycin, ciprofloxacin, and metronidazole by health-care workers visiting each household. The health-care providers must then return after a specified time period to collect biological samples from the volunteers. These results of the prevalence of sexually transmitted infections and HIV must then be compared with the projected values without such intervention. Initial high-cost of such policy may be cost effective in the long run as asymptomatic infections are treated, contact tracing is obviated, treatment seeking behavior is not required and compliance and treatment effectiveness is assured. [8] Antibiotic resistance may result and must be weighed against the benefits of such form of treatment. Developing countries should evaluate such an approach through meticulous trials.
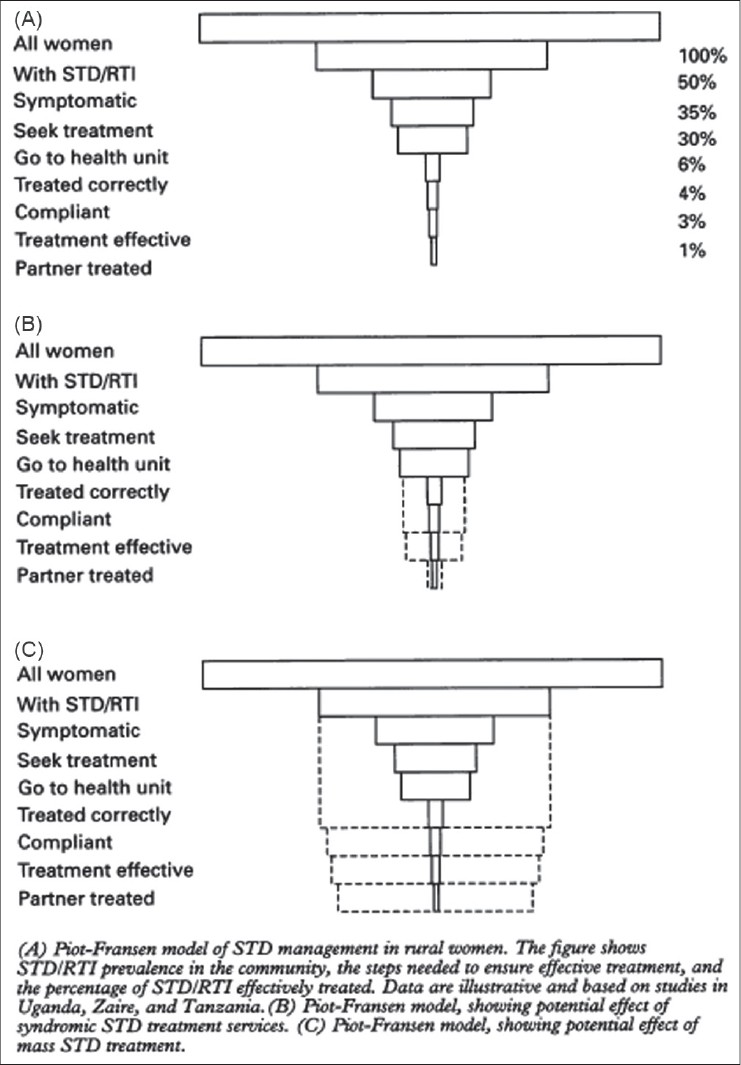 |
| Figure 1: Piot-Fransen model depicting effect of mass treatment on sexually transmitted disease |
A combined approach of a single round of mass treatment with syndromic management and with extensive use of the media to educate the population may be the answer to impede the burgeoning threat of association and spread of STD and HIV.
Acknowledgments
Professor Gobinda Chatterje, Head of the Department of Dermatology of our institute for his help in literature search.
| 1. |
Mabey D. Sexually transmitted diseases in developing countries. Trans R Soc Trop Med Hyg 1996;90:97-9.
[Google Scholar]
|
| 2. |
Wasserheit JN. The significance and scope of reproductive tract infections among Third World women. Suppl Int J Gynecol Obstet 1989;3:145-68.
[Google Scholar]
|
| 3. |
Desai VK, Kosambiya JK, Thakor HG, Umrigar DD, Khandwala BR, Bhuyan KK. Prevalence of sexually transmitted infections and performance of STI syndromes against aetiological diagnosis, in female sex workers of red light area in Surat, India. Sex Transm Infect 2003;79:111-5.
[Google Scholar]
|
| 4. |
Wolday D, G-Mariam Z, Mohammed Z, Meles H, Messele T, Seme W, et al. Risk factors associated with failure of syndromic treatment of sexually transmitted diseases among women seeking primary care in Addis Ababa. Sex Transm Infect 2004;80:392-4.
[Google Scholar]
|
| 5. |
Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: The contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect 1999;75:3-17.
[Google Scholar]
|
| 6. |
Korenromp EL, Van Vliet C, Grosskurth H, Gavyole A, Van der Ploeg CP, Fransen L, et al. Model-based evaluation of single-round mass treatment of sexually transmitted diseases for HIV control in a rural African population. AIDS 2000;14:573-93.
[Google Scholar]
|
| 7. |
Swendeman D, Rotheram-Borus MJ. Innovation in sexually transmitted disease and HIV prevention: Internet and mobile phone delivery vehicles for global diffusion. Curr Opin Psychiatry 2010;23:139-44.
[Google Scholar]
|
| 8. |
Hayes R, Wawer M, Gray R, Whitworth J, Grosskurth H, Mabey D. Randomised trials of STD treatment for HIV prevention: Report of an international workshop. HIV/STD Trials Workshop Group. Genitourin Med 1997;73:432-43.
[Google Scholar]
|
Fulltext Views
3,434
PDF downloads
1,331





