Translate this page into:
Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome with co-existing ulcerative and superficial granulomatous variants of pyoderma gangrenosum
Corresponding author: Dr. Swastika Suvirya, Department of Dermatology, Venereology and Leprosy, King George’s Medical University, Lucknow, India. swastika.p@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Verma P, Shukla P, Deswal S, Malhotra KP, Kumar P, Suvirya S. Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome with co-existing ulcerative and superficial granulomatous variants of pyoderma gangrenosum. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1093_2024
Dear Editor,
SAPHO syndrome is a rare seronegative spondyloarthropathy that stands for synovitis, acne, palmoplantar pustulosis, hyperostosis and osteitis. Palmoplantar pustulosis is the most common associated cutaneous feature, but around 16% of adults never manifest cutaneous symptoms.1
A young boy in his late teens presented to the dermatology outpatient department with multiple painful ulcerative lesions over bilateral cheeks and legs for the past two years. He also recalled a history of episodic pain over multiple joints since the age of 14 years. There was no history of morning stiffness in joints, bowel disturbances or other systemic complaints. Patient was prescribed non-steroidal anti-inflammatory drugs (NSAIDs), isotretinoin, and antibiotics from various physicians, without relief.
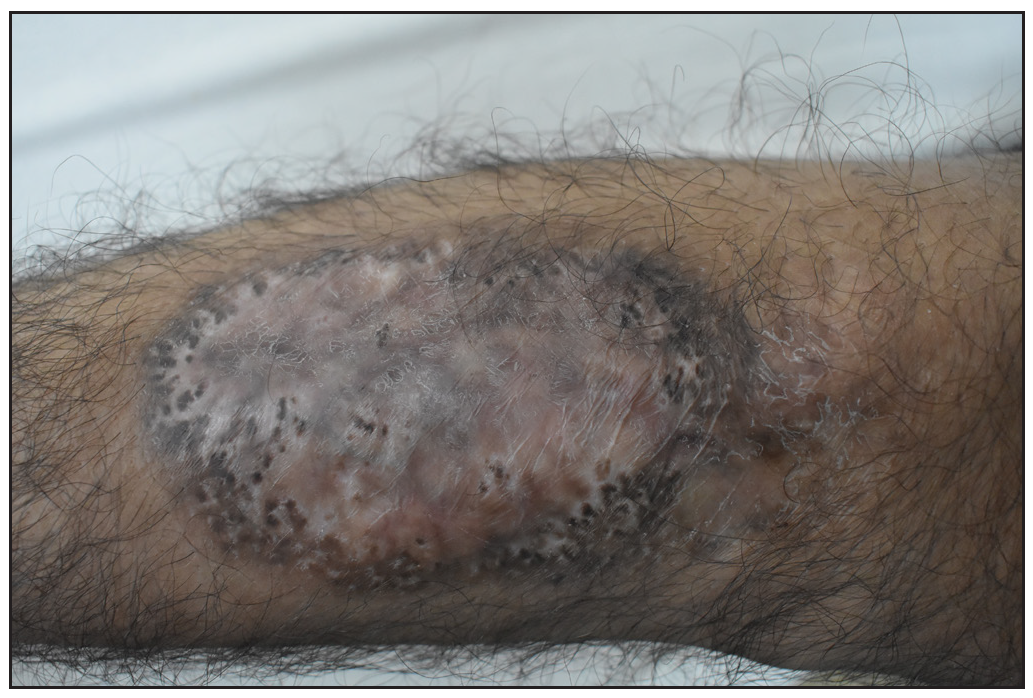
On examination, erythematous plaques of approximately 8 × 6 cm size were present on both cheeks with an overlying yellowish crust and serosanguinous discharge [Figure 1a]. A tender indurated ulcer of size 10 × 6 cm with undermined edges was present on the lateral aspect of the right leg, covered with haemorrhagic crust and serosanguinous discharge, with the surrounding skin showing violaceous discoloration [Figure 1b]. Multiple rounds to oval depressed cribriform scars were noted on all four limbs.
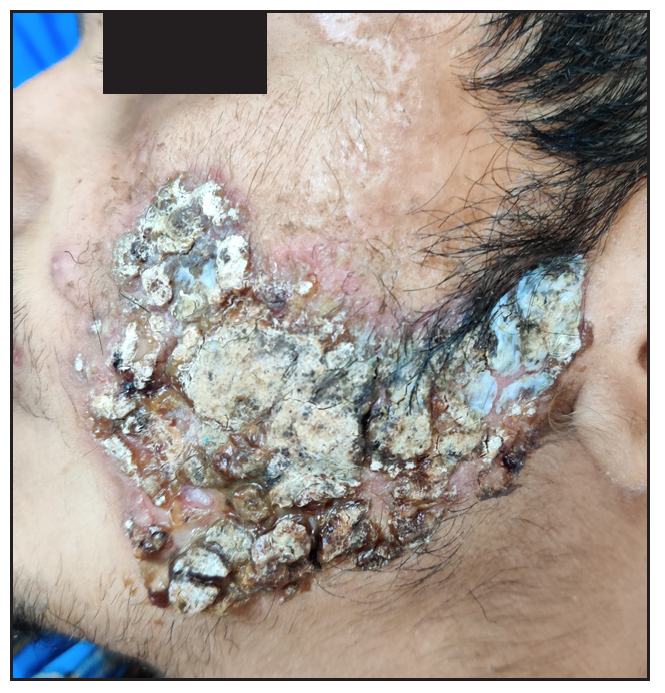
- Erythematous plaque over the left cheek with areas of yellow-black crusting and scarring.

- An ulcer over the right leg with haemorrhagic crust and serosanguinous discharge. Surrounding peripheral skin showed violaceous discoloration.
There was tenderness at the bilateral knee, ankle and right sternoclavicular joint. Medial end of the right clavicle appeared enlarged as compared to the left [Supplementary Figure 1]. Routine laboratory investigations did not reveal any abnormality. Erythrocyte sedimentation rate was 64 mm/hr (Normal range < 10 mm/hr for men). Anti-nuclear antibodies were positive (2+, fine speckled). Anti-double stranded deoxyribonucleic acid (Anti-dsDNA) antibody, rheumatoid factor, Copmlement levels C3 and C4, anti-myeloperoxidase and anti-proteinase-3 antibodies were negative. Biopsy from facial plaque showed deep dermal ulcer with intense mixed dermal inflammation and ill-defined granulomas [Figure 1c]. Biopsy from leg lesion showed epidermal ulceration with mixed dermal inflammation and perivascular lymphocytic infiltrate [Figure 1d]. Direct immunofluorescence (DIF), bacterial, mycobacterial, and fungal cultures were negative. Ultrasound whole abdomen and colonoscopy were within normal limits. X-rays of hip joints, bilateral elbow, knee and chest revealed no abnormality.
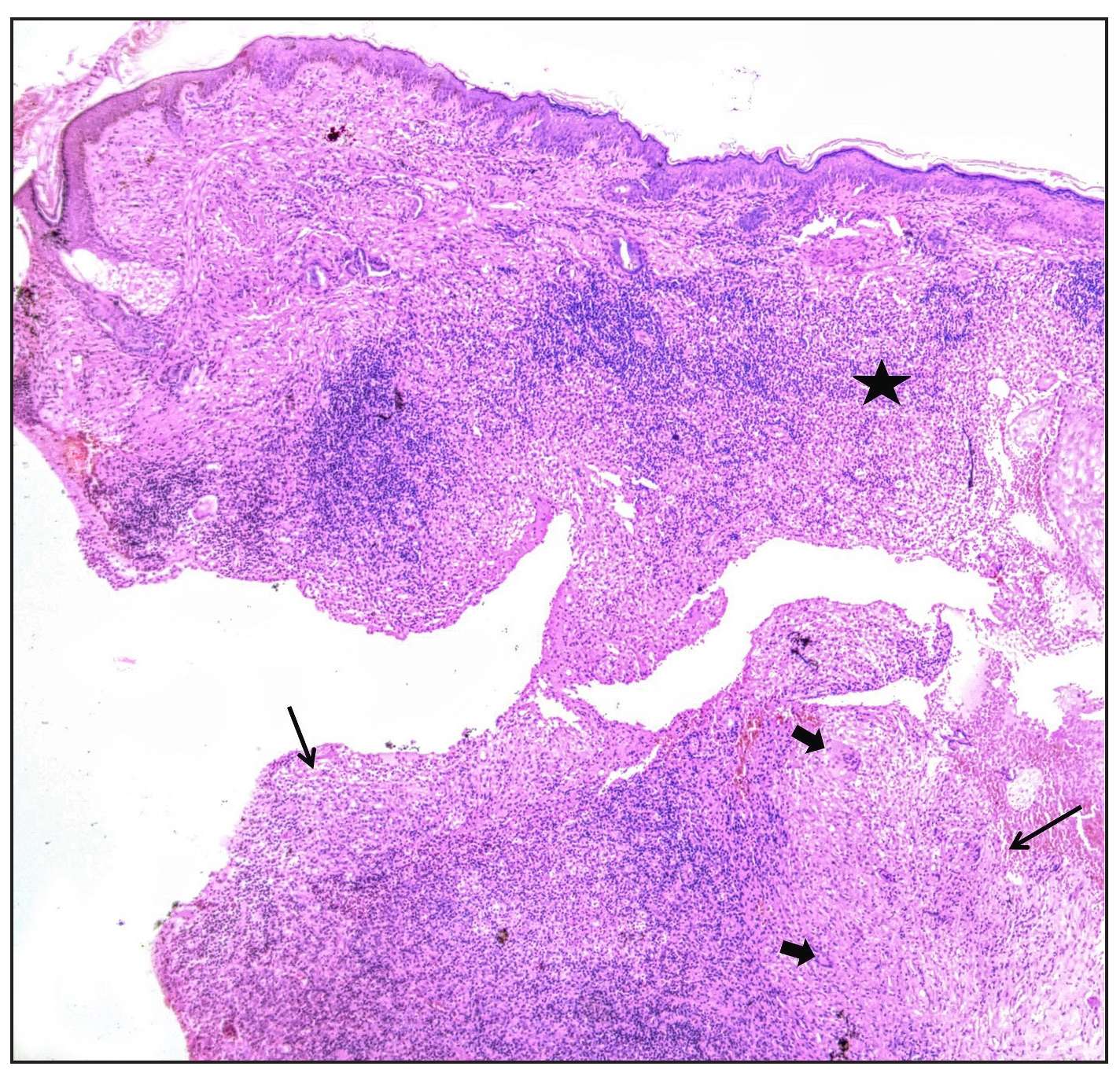
- Biopsy from face showing intense mixed inflammation in superficial dermis (asterisk) and deep dermal granulomas (black arrows) with giant cells (block arrows) (Haematoxylin & eosin, 50x.)
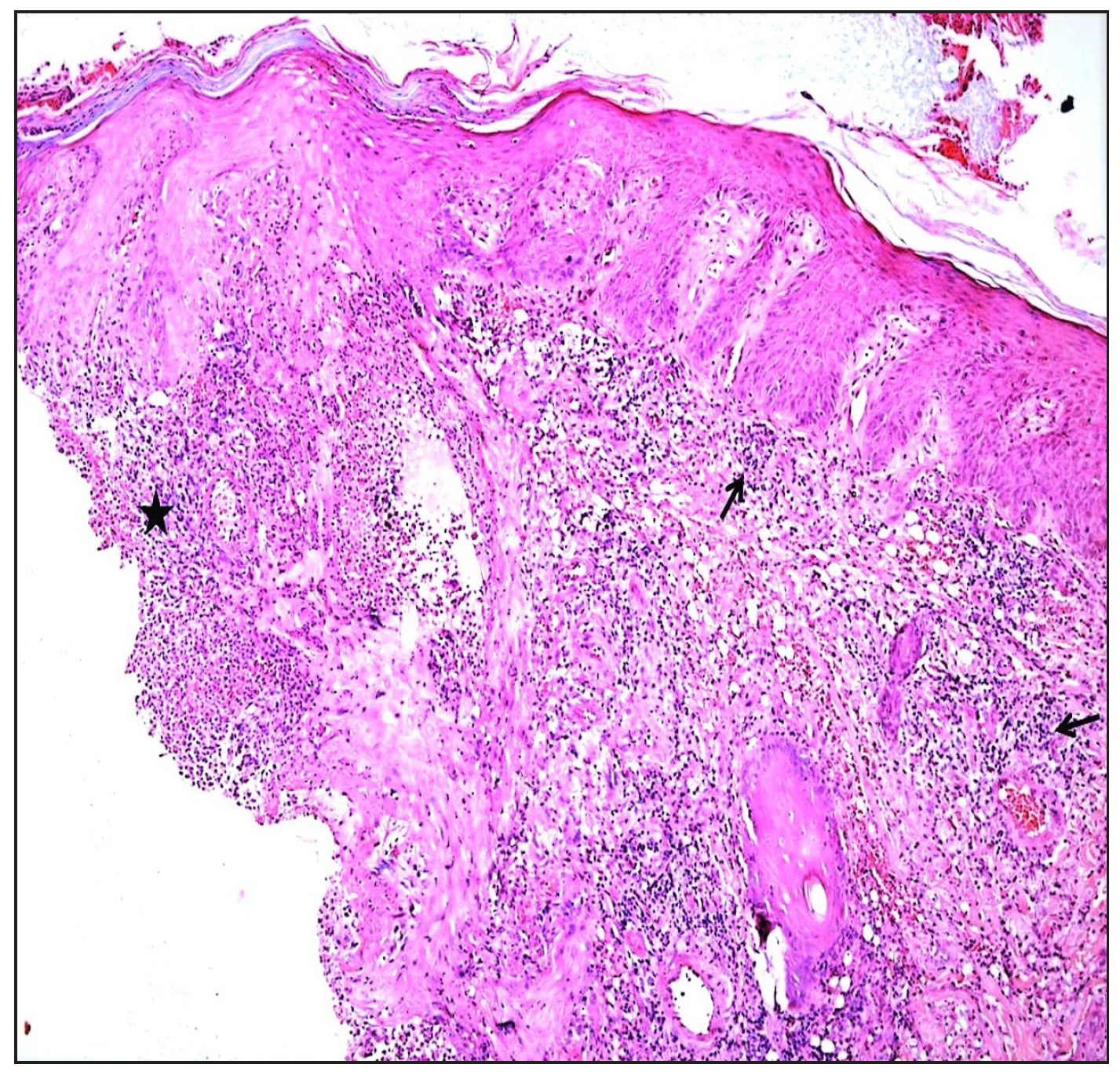
- Biopsy from leg plaque showing ulcer edge (asterisk) and lymphocytic vasculitis with infiltrate around dermal vessels (black arrows) (Haematoxylin & eosin, 200x).
Tc-99m methylene diphosphonate (MDP) whole body bone scan performed in the anterior and posterior view revealed increased radiotracer uptake in bilateral shoulders (right>left), left elbow, bilateral knee and ankle joints. Right clavicle was also expanded along with increased tracer uptake [Figure 2a]. The scan findings were consistent with osteitis of the clavicle and inflammation at the above joints. Reconstructed three-dimensional (3D) computed tomography (CT) image of bones of the anterior chest wall showed hyperostosis of the bony and sternal end of the right clavicle [Figure 2b]. Synovial fluid aspirate from the knee joint did not show any growth on culture, suggestive of the aseptic nature of inflammation.
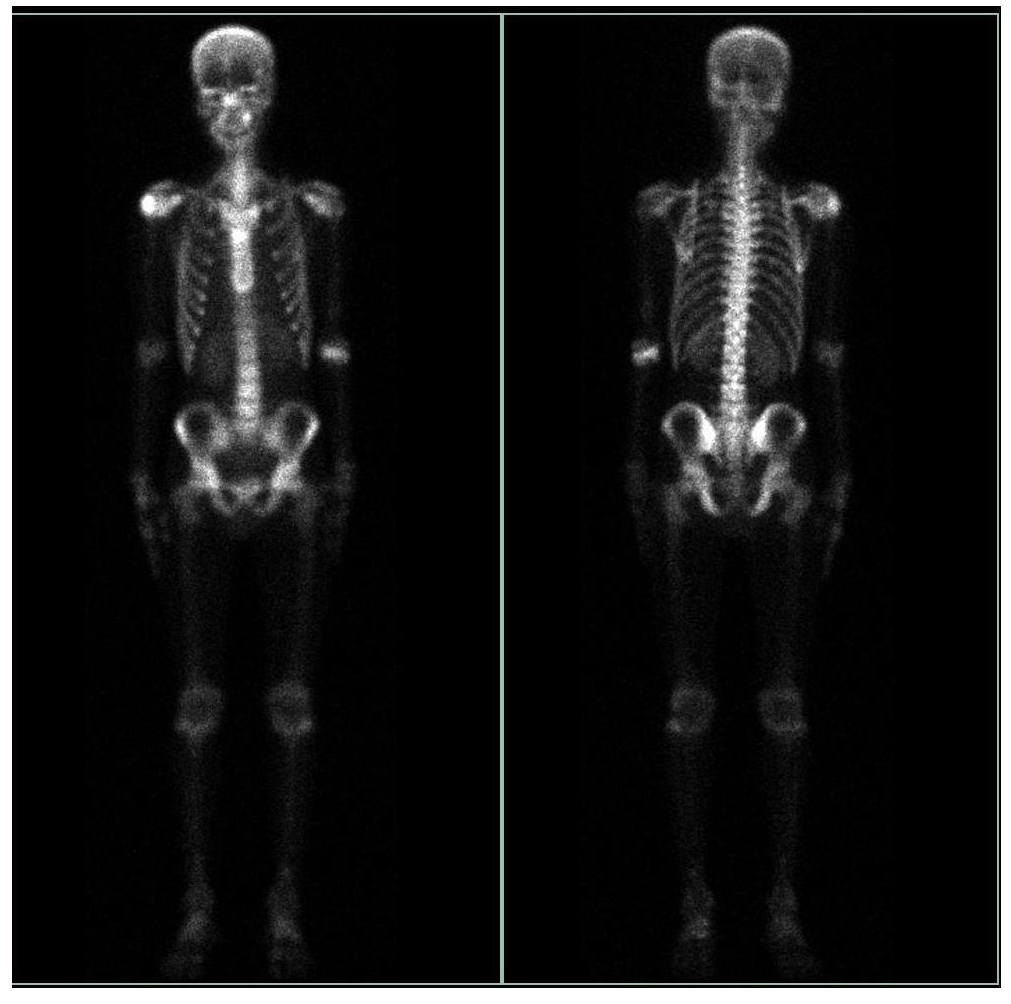
- 99mTc MDP (Methyl Diphosphonate) bone scan anterior and posterior images showing increased radiotracer uptake in bilateral shoulders (right> left), left elbow, bilateral knee and bilateral ankle joint. The right clavicle appears expanded with a mild increase in tracer uptake.
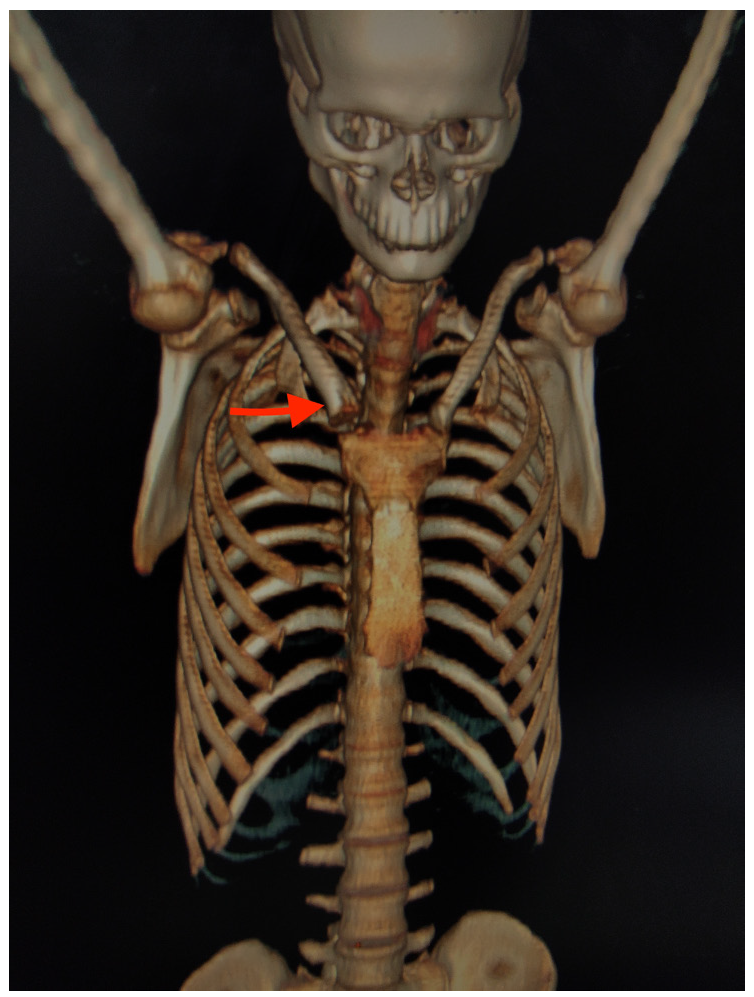
- Reconstructed 3D CT image of bones of the anterior chest wall showed hyperostosis of bony and sternal end of right clavicle (red arrow).
A final diagnosis of SAPHO syndrome2 was established along with co-existing superficial granulomatous (face) and ulcerative variants (legs) of pyoderma gangrenosum (PG) in consultation with a rheumatologist. Patient was administered infliximab 5mg/kg IV at weeks 0, 2, 6 and 14. On induction of infliximab therapy, he showed promising responses in both cutaneous and bony symptoms. Patient is presently in remission one month after the last dose of infliximab therapy [Figure 3a,b]. Dermatological disorders, infrequently reported with SAPHO syndrome, include acne conglobata, acne fulminans, pustular psoriasis, subcorneal pustular dermatosis, hidradenitis suppurativa, psoriasis vulgaris, linear IgA (immunoglobulin A) disease, Behçet’s disease, Sweet syndrome and very rarely, PG (pyoderma gangrenosum).3 PG is an uncommon, chronic, recurrent neutrophilic dermatosis that requires clinicopathological correlation for diagnosis. With four different subtypes, ulcerative PG is the most common variant. Superficial granulomatous PG, also known as the vegetative subtype, is infrequent and very rarely reported.4

- Scarring over right cheek post-treatment.
- Healed ulcer with cribriform scarring over the right leg post-treatment.
So far, only a very few cases of SAPHO syndrome with PG have been described, and none with two subtypes of PG simultaneously co-existing with SAPHO.5,6 The pathogenesis of SAPHO remains unclear, but similarities with auto-inflammatory disorders and involvement of cytokines like interleukin-1-beta (IL-1β) and tumour necrosis factor-alpha (TNFα) have been observed. These findings suggest that PG and SAPHO may represent different manifestations of a single auto-inflammatory spectrum.7 Treatment options include NSAIDs and intra-articular corticosteroids for arthritis; bisphosphonates for bone involvement; and systemic corticosteroids or other immunosuppressive medications, TNFα inhibitors and IL-1antagonists for both skin and bone disease.5
In the above case, simultaneous presence of PG with arthritis served as a diagnostic dilemma. The differentials for the same have been illustrated in Table 1. Distinctive radiographic features of the osteoarticular lesions formed the cornerstone for diagnosis in the index case. Despite being rare, it would be a good practice to keep an eye out for this condition when dealing with a case of neutrophilic dermatoses or a seronegative spondyloarthropathy.
| S.no. | A) PG lesions with arthritis | |||||
|---|---|---|---|---|---|---|
| Condition | Clinical findings | Laboratory findings | Imaging | |||
| Cutaneous | Osteoarticular | Others | ||||
| 1. | Vasculitis |
|
|
|
|
X-ray joints: Meniscus horns, intra-articular bodies of Pellagri-Shtaydi and Hoff, Baker cysts, tendovaginitis, subchondral sclerosis and osteocystosis |
| 2. | *Inflammatory arthritides: | |||||
| a) RA (Rheumatoid arthritis) |
|
|
|
|
X-ray joints: Periarticular osteopenia, uniform joint space loss, bone erosions and soft tissue swelling | |
| b) PsA1 (Psoriatic arthritis) |
|
|
|
|
X-ray joints: Periarticular soft tissue swelling, marginal erosion and pencil-in-cup deformity | |
| 3. | *Autoinflammatory syndromes | |||||
| a) PAPA syndrome7 [Pyoderma Gangrenosum, Acne, and Pyogenic arthritis syndrome] |
|
|
- |
|
X-ray joints: Effusion without erosions Ultrasound:Soft tissue swelling |
|
| b) PAPASH syndrome7 [Pyoderma gangrenosum, Pyogenic arthritis, Acne, and Suppurative hidradenitis syndrome] |
|
|
- |
|
X-ray joints:Similar to PAPA | |
| c) SAPHO syndrome2 |
|
|
- |
|
X-ray joints:Hyperostosis, sclerosis, osteitis, osteolysis and periosteal reaction Bone scintigraphy: Increased uptake in affected areas |
|
| 4. | *IBD {Inflammatory bowel disease} (e.g. Crohn’s disease, ulcerative colitis) |
|
|
|
|
Radiograph:Axial spondyloarthritis and non-erosive peripheral arthritis Barium studies and CT findings: IBD |
| 5. | *SLE (Systemic lupus erythematosus) |
|
|
|
|
X-ray joints: Non-erosive, non-deforming arthritis MRI: effusions, synovial and/or tenosynovial hypertrophy and vascularity |
| 6. | *Behçet’s disease |
|
|
|
|
X-ray joints: Non-erosive, non-deforming arthritis commonly involving knee, wrist, ankle, elbow |
| B) PG like ulcers with arthritis | ||||||
| 1. | *Infectious diseases |
|
|
|
|
X-ray joints: Effusion, joint space narrowing, joint destruction MRI in TB arthritis: #Phemister triad |
| 2. | *Malignancy (e.g., Mycosis fungoides, leukemia) |
|
|
|
|
X-ray hands:Synovitis, erosive and deforming polyarthritis, joint space narrowing, periarticular osteoporosis |
#Phemister triad: marginal erosion, periarticular osteoporosis and joint space narrowing.
PG: Pyoderma gangrenosum; ANA: anti-nuclear antibodies; ANCA: anti-neutrophil cytoplasmic antibodies; DIF: Direct immunofluorescence; s/o: suggestive of; RA: Rheumatoid arthritis; MCP: Metacarpophalangeal; PIP: Proximal interphalangeal; MTP: Metatarsophalangeal; CTS: Carpel tunnel syndrome; RF: Rheumatoid factor; anti-CCP: anti-cyclic citrullinated peptide; PsA: Psoriatic arthritis; DIP: Distal interphalangeal; PAPA: Pyogenic arthritis, Pyoderma gangrenosum, and Acne; PAPASH: Pyogenic arthritis, Pyoderma gangrenosum, Acne, and Hidradenitis suppurativa; SAPHO: Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis; IBD: Inflammatory bowel disease; ASCA: anti-saccharomyces cerevisiae antibodies; SLE: Systemic lupus erythematosus; MRI: Magnetic resonance imaging; HLA-B51: Human leukocyte antigen-B51
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- SAPHO syndrome: A review. J Child Orthop. 2015;9:19-27.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermatology (4th ed). China: Elsevier; 2018. p. :468-70.
- Superficial granulomatous pyoderma gangrenosum involving the face: A case series of five patients and a review of the literature [Formula: see text] J Cutan Med Surg. 2021;25:371-6.
- [CrossRef] [PubMed] [Google Scholar]
- Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome associated with pyoderma gangrenosum: Report of two patients. Int J Dermatol. 2023;62:e186-9.
- [CrossRef] [PubMed] [Google Scholar]
- SAPHO syndrome associated with hidradenitis suppurativa and pyoderma gangrenosum successfully treated with adalimumab and methotrexate: A case report and review of the literature. Int J Dermatol. 2018;57:10-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pyoderma gangrenosum and its syndromic forms: Evidence for a link with autoinflammation. Br J Dermatol. 2016;175:882-91.
- [CrossRef] [PubMed] [Google Scholar]






