Translate this page into:
Syphilitic onychopathy: Clinical and onychoscopy findings
Corresponding author: Dr. Archana Singal, Department of Dermatology & STD, University College of Medical Sciences & GTB Hospital, Delhi, India. archansingal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aggarwal B, Singal A. Syphilitic onychopathy: Clinical and onychosocpy findings. Indian J Dermatol Venereol Leprol. 2025;91:97-100. doi: 10.25259/IJDVL_1289_2023
Dear Editor,
Syphilis is a preventable and treatable sexually transmitted infection (STI). Its protean genital and extragenital manifestations may result in delayed diagnosis and treatment. Nail involvement, although rare, has been observed across all stages of syphilis but often remains overlooked or receives limited attention in the literature.1 Primary nail involvement, arising from sexual or healthcare exposure, constitutes 14% of extragenital manifestation of syphilis.2 Other non-primary manifestations include alterations in the nail plate and nail folds.2 Understanding these nail changes can significantly aid in achieving a timely and accurate diagnosis.
A 68-year-old man presented to the STI clinic with asymptomatic hyperpigmented lesions on his palms and soles along with generalised raised red crusted lesions, including the genitalia, for the past 3-months. He denied any prior history of genital or oral ulcers, drug use, fever or joint pain. Notably, he disclosed the loss of his wife 18 years ago and denied engaging in sexual promiscuity, recent sexual encounters, or other high-risk behaviours. Cutaneous examination revealed multiple well-defined erythematous to hyperpigmented plaques with crusting and collarette of scales, varying in size from 0.5 cm to 3.5 cm. These lesions were distributed across the face, neck, buttocks, both the legs and the dorsa of the hands and feet. Additionally, lesions were also present on the palms and soles, accompanied by positive Biett’s and Buschke–Ollendorff signs [Figure 1a]. On genital examination, phimosis was observed, in addition to multiple erythematous plaques present on the prepuce, glans, penile shaft, and scrotum [Figure 1b]. Moist plaques were present in the perianal area involving the anal verge. Bilateral non-tender, non-matted significant inguinal lymphadenopathy was noted. Rest of the mucosae were normal. Nail examination revealed mildly tender erythematous swelling with overlying crusted erosion along the proximal nail fold, extending distally over the nail bed. Peripheral scaling and ragged cuticle were observed on both the left fifth finger and right middle finger. Additionally, longitudinal melanonychia was present on the right middle finger [Figure 1c]. On onychoscopy of both affected fingers, the fullness of the proximal nail fold with brown crusting and white-yellow areas with peripheral white scaling was noted. In addition, increased vascularity of the nail bed [Figure 2a] and short linear vessels on the proximal nail fold [Figures 2a and 2b] was noted and, after treatment marked improvement was observed with residual linear vessels in the nail bed and onychomadesis as a manifestation of prolonged nail matrix insult [Figures 2c and 2d]. Histopathological evaluation of the nail lesions was not done. Dark ground microscopy yielded positive results from the perianal lesion but negative from the periungual lesions. The Venereal Disease Research Laboratory (VDRL) test showed a reactive titre of 1:32, and the Treponema pallidum hemagglutination assay (TPHA) yielded a positive result. Routine haematological and biochemical investigations were normal and viral serologies (HIV, Hepatitis B & C) were negative. A diagnosis of secondary syphilis was made and the patient was treated with an intramuscular injection of 2.4 million units of benzathine penicillin G after sensitivity testing under observation. On one-month follow up, VDRL titre declined to 1:4 (fourfold) and resolution of mucocutaneous lesions with hyperpigmentation was observed [Figures 3a and 3b] along with reduction in periungual swelling and crusting [Figure 3c].

- Hyperpigmented plaques over the bilateral palms and soles, Beitt’s sign positive (yellow arrow).

- Multiple psoriasiform annular plaques present on bilateral inner thighs, scrotum and penile shaft (Blue star).

- Left hand’s fifth digit shows crusted ulceration encroaching the nail bed and the right hand’s third digit shows swelling with overlying crusted ulceration.
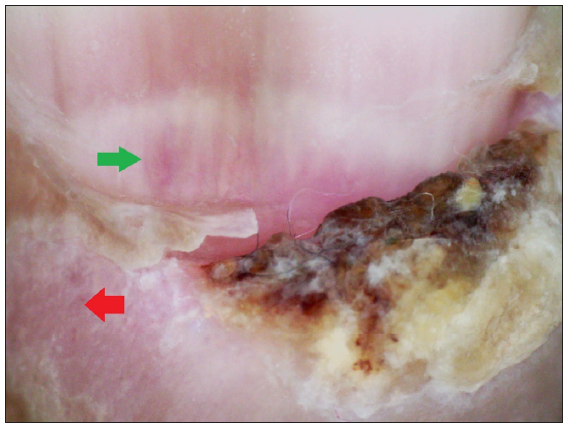
- Pre-treatment: Brown crusting, swelling and short linear vessels on PNF (red arrow) and nail bed vascularity (green arrow) of 3rd digit of right hand (Dino-lite AM7115MZT, non-contact, polarised mode, 50x).
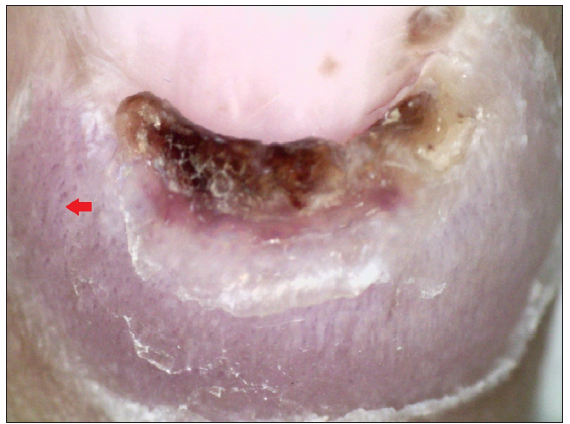
- Pre-treatment: Brown crusting, swelling and short linear vessels on proximal nail fold (PNF) (red arrow) and nail bed vascularity of left 5th digit. Dino-lite AM7115MZT, non-contact, polarised mode, 50x).
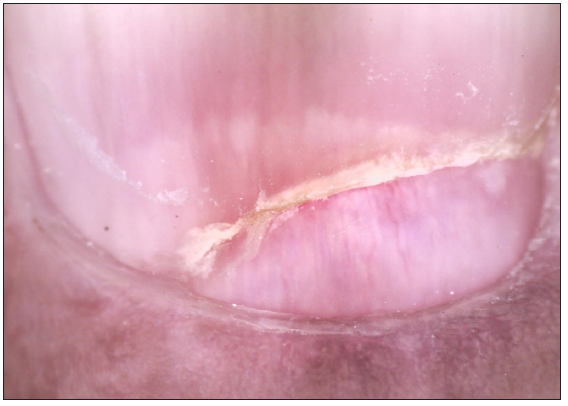
- Post treatment: Oychomadesis with proximal nail fold devoid of any lesion on right 3rd digit (Dino-lite AM7115MZT, non-contact, polarised mode, 50x).

- Post treatment: Onychomadesis with normal proximal nail fold of left 5th digit (Dino-lite AM7115MZT, non-contact, polarised mode, 50x).

- Resolution of scaling and crusting on the feet and palms.

- Resolution of perianal lesion with hyperpigmentation.

- Resolution of swelling, ulceration crusting with onychomadesis.
Syphilis is caused by Treponema pallidum and exhibits a wide range of mucocutaneous manifestations across different stages, aptly referred to as the ‘great imitator’.3 Primary syphilis is identified by syphilitic chancre, while secondary syphilis exhibits a range of manifestations such as condyloma lata, alopecia, mucosal patches, palmoplantar or truncal syphilide. Untreated primary or secondary syphilis leads to an early or late latent phase followed by tertiary syphilis which can result in severe complications, including cardiovascular syphilis (e.g. aortic aneurysm), neurosyphilis (e.g. meningitis) or gummatous syphilis. Nail changes constitute a rare manifestation of the disease.4 Nail changes in syphilis may arise from direct inflammation around the nail, potential matrix damage by Treponema pallidum and the systemic impact of syphilis on overall health.4 Primary syphilis has been reported to present as fingernail chancre with onychodystrophy and/or paronychia.5,6 They manifest as painful, persistent, crusted ulceration, developing over the free edge of the nail plate or along nail folds.5 Secondary syphilis can affect multiple fingers and toenails. In this stage, nail changes can be categorised based on the involvement of either the nail plate or the surrounding area (subungual or periungual areas).1 Syphilitic onychia encompasses splitting (Onyxis craquele), fissuring, onycholysis, pitting, beau’s line and onychomadesis, while syphilitic paronychia is the inflammation of the periungual or subungual area. Other changes include ulcerative paronychia, complete nail loss (anonychia) and syphilitic dactylitis.1,4,7 In tertiary syphilis, though rare, nail involvement can manifest as onychodystrophy, onychogryphosis and paronychia.4 There are only anecdotal reports and no case studies regarding nail changes in syphilis in the literature and to the best of our knowledge there are no reports of onychoscopic changes in syphilitic nails.5-7 Various nail changes encountered in syphilis have been enumerated in Table 1.
| Stages | Clinical features |
|---|---|
| Primary syphilis | Syphilitic chancre, onycholysis, onychodystrophy, paronychia, anonychia |
| Secondary syphilis |
1. Nail plate changes – syphilitic onychia, onyxis-craquele, Beau’s lines, onychomadesis, onycholysis, onychogryphosis (thick, discoloured nail with increased curvature), onychauxis (thick, discoloured nails with loss of translucency), racket nails, melanonychia, punctate leukonychia, clubbing, koilonychia, onychoptosis (Shedding of nail) and anonychia 2. Peri/subungual changes – paronychia, subungual papules |
| Tertiary syphilis | Amber coloured nails, onychodystrophy, onychogryphosis, paronychia |
In our case, we observed syphilitic onychopathy presenting as painful, crusted, ulcerated periungual plaques encroaching the nail bed and affecting two fingernails. Confirmatory serological tests and a rapid response to penicillin injection validated the diagnosis of syphilitic onychopathy. With the recent resurgence of syphilis, it is imperative for the treating physician to identify the onychopathic changes for early management and follow up.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Periungual lesion due to secondary syphilis. Skin Appendage Disord. 2017;2:116-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non-primary nail-plate syphilis in an HIV-infected patient. SAGE Open Med Case Rep. 2018;6:1-3.
- [CrossRef] [PubMed] [Google Scholar]
- Bacterial, viral and other infections. In: Baran R, Berker D, Holzberg Mark BM, Richert B, Thomas L, eds. Baran & Dawber’s Diseases of the nails and their management (5th ed). UK: John Wiley and Sons Ltd; 2019. p. :396-8.
- [Google Scholar]
- Primary syphilis of the fingers. Br J Vener Dis. 1983;59:169-71.
- [CrossRef] [PubMed] [Google Scholar]





