Translate this page into:
Syringocystadenocarcinoma papilliferum with coexisting trichoblastoma: A case report with review of literature
Correspondence Address:
Rajeshwari K Muthusamy
Department of Pathology, Kovai Medical Center and Hospital, Coimbatore - 641 014, Tamil Nadu
India
| How to cite this article: Muthusamy RK, Mehta SS. Syringocystadenocarcinoma papilliferum with coexisting trichoblastoma: A case report with review of literature. Indian J Dermatol Venereol Leprol 2017;83:574-576 |
Abstract
We present a unique case of syringocystadenoma with malignant transformation into syringocystadenocarcinoma papilliferum and coexisting trichoblastoma arising de novo in a scalp swelling of long duration in a 78-year-old woman. Syringocystadenocarcinoma papilliferum was described by the World Health Organization as an extremely rare malignant adnexal tumor of apocrine origin with varied histology with some cases reported in literature.Introduction
Syringocystadenocarcinoma papilliferum, an extremely rare malignant adnexal tumor, usually arises from syringocystadenoma, a benign adnexal tumor of apocrine origin. It was described by Stokes as early as 1917. Since then, less than 30 cases have been reported till date. Hoekzema et al. have well documented the transformation of syringocystadenoma into syringocystadenocarcinoma papilliferum in their study.[1] Syringocystadenoma occurs most commonly on the head and neck region and is usually associated with nevus sebaceus of Jadassohn. It can arise de novo and in other parts of the body. As nevus sebaceous has pluripotency, it can give rise to sebaceous adenoma, trichoblastoma, syringocystadenoma and basal cell carcinoma.[2] We were unable to find any previous report of syringocystadenocarcinoma papilliferum arising de novo in syringocystadenoma with coexisting trichoblastoma.
Case Report
A 78-year-old woman came to Kovai Medical Center and Hospital (Coimbatore) with a history of a lesion on the scalp of peanut size for a duration of around 10 years. There was recent increase in the size of the lesion for the past 6 months with ulceration and mild pain. She was hypertensive for the past 8 years, under control. On examination, she had an ulcerated nodular lesion on the scalp measuring 4.5 cm × 3.5 cm, attached to the scalp with a broad base. There was no regional lymphadenopathy. After preoperative evaluation, the lesion was excised with wide margins.
The specimen consisted of hairy skin with a raised, broad based nodular exophytic lesion with ulceration and crust on the top measuring 4.5 cm × 3.5 cm × 2 cm.. The tumor cut surface was soft and fleshy. Microscopically, a tumor was seen in the dermis and subcutaneous fat, infiltrating as nests. Some of these tumor nests showed ductal lumina with cellular debris within. The tumor cells were large, polygonal with granular eosinophilic cytoplasm with moderately pleomorphic oval nuclei. Fibrocollagenous stroma with plasma cell-rich infiltrate and increased mitosis were noted. There was pagetoid spread into the overlying epidermis with ulceration and exudate. Superficially, benign counterpart was seen with cystic invagination from the epidermis showing papilla, lined by bilayered cells. The inner layer was columnar with decapitating secretions while the outer layer was cuboidal. Transition to malignancy was prominent [Figure - 1] and [Figure - 2]. Periodic acid–Schiff (with and without diastase) showed positivity along the apical border of tumor cells. The histomorphology was that of a syringocystadenocarcinoma papilliferum arising from syringocystadenoma. Adjacent to this tumor, a separate tumor showing proliferation of basaloid cells in nests [Figure - 3] was seen in the mid-dermis with stromal condensation around. These cells had scant cytoplasm and oval dark nuclei with minimal atypia and some mitoses [Figure - 4]. There was no connection to the overlying epidermis or the adjacent malignant tumor. The morphology was that of a trichoblastoma. Histological features suggesting the existence of nevus sebaceous were not found. Hence, a diagnosis of syringocystadenocarcinoma papilliferum arising from syringocystadenoma and a coexisting trichoblastoma was made.
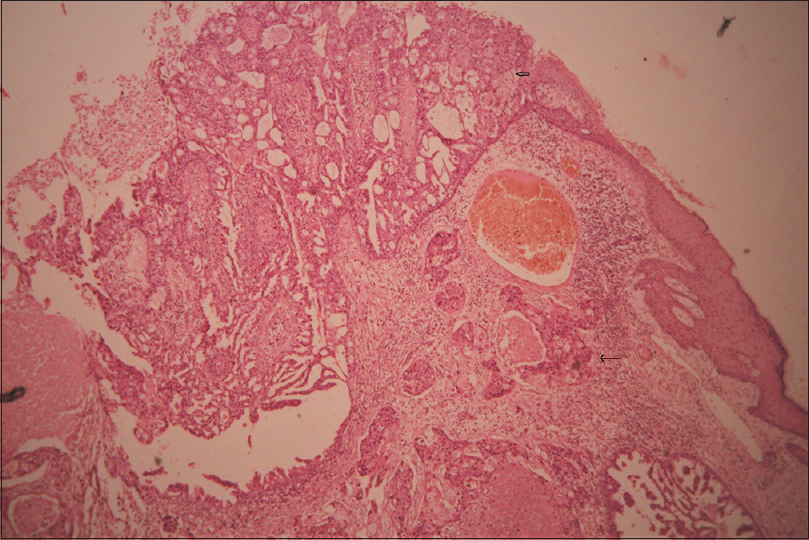 |
| Figure 1: Syringocystadenocarcinoma in the deep dermis (black arrow) with syringocystadenoma in the superficial dermis (block arrow) with clear transition and overlying epidermis (H and E, ×400) |
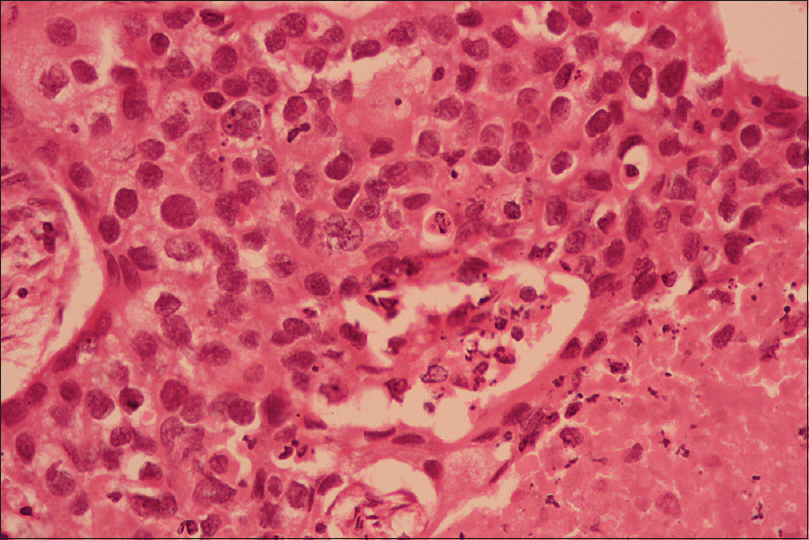 |
| Figure 2: Tumor nests of syringocystadenocarcinoma with high-grade nuclear features and cellular debris in the center (H and E, ×100) |
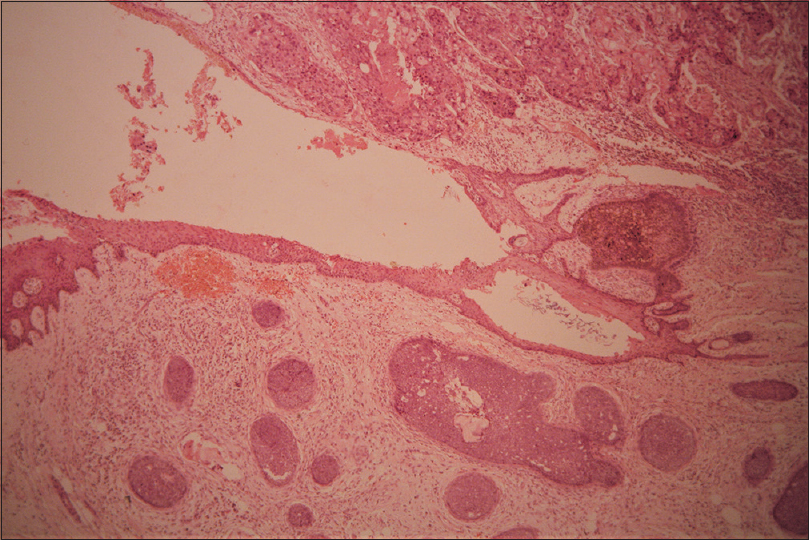 |
| Figure 3: Skin with malignant adnexal tumor, syringocystadenocarcinoma papilliferum in the upper half of the image and a separate tumor, trichoblastoma, in the lower half (H and E, ×400) |
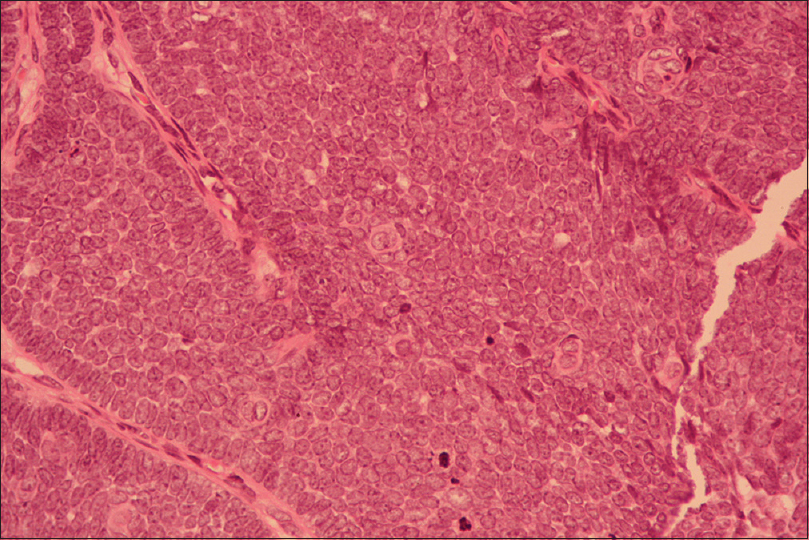 |
| Figure 4: High-power image of trichoblastoma with nuclear features and stromal condensation (H and E, ×100) |
Discussion
Syringocystadenocarcinoma papilliferum, an extremely rare malignant adnexal tumor, is described by the World Health Organization as a malignant transformation of syringocystadenoma occurring in middle-aged to elderly individuals with a predilection for the head and neck. The other possible sites reported include chest, back, supra pubic and perianal areas.[3],[4],[5] There was no gender preponderance. It seems to arise from a long-standing syringocystadenoma in a background of nevus sebaceous of Jadassohn in one-third of the cases. The lesion usually presents as a raised nodule for a long duration, usually decades and recent sudden increase in size with ulceration, crust formation and mild pain. Regional lymphadenopathy was uncommon, accompanying occasional reports with lymph node involvement.[5]
Histologically, syringocystadenocarcinoma papilliferum resembles syringocystadenoma in all aspects, marked by funnel-shaped invaginations from the epidermis with transition from keratinizing squamous epithelium into glandular component with subjacent cystic changes and papilla formation. The cells are bilayered with outer cuboidal cells and inner layer of columnar cells with decapitating secretions. The fibrous stroma contains an inflammatory infiltrate rich in plasma cells. The malignant counterpart in the deeper aspect shows cells of variable thickness with dermal and/or subcutaneous infiltration, cellular debris in the center of these nests, high nuclear-cytoplasmic ratio, nuclear atypia and increased mitosis.[6]
Leeborg et al. have described the earlier cases of syringocystadenocarcinoma papilliferum with the predominant site of involvement being head and neck in the elderly, presenting as a swelling for a long duration of up to 30 years and recent increase in size as seen in our patient.[6] Leeborg et al. and Paradiso et al. had described a high-grade component of the tumor mimicking squamous cell carcinoma and then proven to be adenocarcinoma.[6],[7] Paradiso et al. further provided the evidence of stem cell features in the tumor by immunohistochemistry with overexpression of stem cell marker nestin, CD44 and CD133.[7] Epithelial–mesenchymal transition-like properties in syringocystadenocarcinoma papilliferum [7] were also discussed, considering epithelial–mesenchymal transition as a general event implicated in all types of carcinoma, providing a survival advantage.[7]
Syringocystadenoma in association with nevus sebaceous was found in 30%–40% of the cases. We found <30 cases of syringocystadenocarcinoma papilliferum in English literature and with loco-regional metastasis in <5 cases.[8],[9] Syringocystadenoma was also described to be coexisting with trichoblastoma in some of the reports published.[2] Our case was unique in some aspects. First, syringocystadenoma with malignant transformation into syringocystadenocarcinoma papilliferum with clear transition areas proving the potential of syringocystadenoma to become malignant. Second, coexistence of trichoblastoma in the subjacent dermis. Third, there was no association with nevus sebaceous though it was in scalp.
The present case shows de novo origin of syringocystadenoma with malignant transformation in a long-standing swelling and coexistence of trichoblastoma. Simultaneous occurrence of these tumors arising de novo is rare. Hence, we report this case due to its rarity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hoekzema R, Leenarts MF, Nijhuis EW. Syringocystadenocarcinoma papilliferum in a linear nevus verrucosus. J Cutan Pathol2011;38:246-50.
[Google Scholar]
|
| 2. |
Namiki T, Miura K, Ueno M, Arima Y, Nishizawa A, Yokozeki H. Four different tumors arising in a nevus sebaceous. Case Rep Dermatol 2016;8:75-9.
[Google Scholar]
|
| 3. |
Numata M, Hosoe S, Itoh N, Munakata Y, Hayashi S, Maruyama Y. Syringadenocarcinoma papilliferum. J Cutan Pathol 1985;12:3-7.
[Google Scholar]
|
| 4. |
Park SH, Shin YM, Shin DH, Choi JS, Kim KH. Syringocystadenocarcinoma papilliferum: A case report. J Korean Med Sci 2007;22:762-5.
[Google Scholar]
|
| 5. |
Iga N, Fujii H, Miyake T, Ehara M, Kore-Eda S. Syringocystadenocarcinoma papilliferum in the perianal area. Case Rep Dermatol 2015;7:84-9.
[Google Scholar]
|
| 6. |
Leeborg N, Thompson M, Rossmiller S, Gross N, White C, Gatter K. Diagnostic pitfalls in syringocystadenocarcinoma papilliferum: Case report and review of the literature. Arch Pathol Lab Med 2010;134:1205-9.
[Google Scholar]
|
| 7. |
Paradiso B, Bianchini E, Cifelli P, Cavazzini L, Lanza G. A new case of syringocystadenocarcinoma papilliferum: A rare pathology for a wide-ranging comprehension. Case Rep Med 2014;2014:453874.
[Google Scholar]
|
| 8. |
Rao PB, Ghosh S, Mohapatra M, Philip NP, Kumar PR, Manam S, et al. Chemoradiotherapy in a case of malignant syringocystadenocarcinoma papilliferum of vulva with locoregional failure. Case Rep Oncol Med 2015;2015:638294.
[Google Scholar]
|
| 9. |
Castillo L, Moreno A, Tardío JC. Syringocystadenocarcinoma papilliferum in situ: Report of a case with late recurrence. Am J Dermatopathol 2014;36:348-52.
[Google Scholar]
|
Fulltext Views
2,722
PDF downloads
1,512





