The case of a bleeding nail
Corresponding author: Prof. Chander Grover, Department of Dermatology and STD, University College of Medical Sciences and GTB Hospital, Dilshad Garden, Delhi - 110 095, India. chandergroverkubba76@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Grover C, Chauhan A, Sharma S. The case of a bleeding nail. Indian J Dermatol Venereol Leprol 2021;87:127-30.
The Case
A 45-year-old farmer presented with thickening and discoloration of medial half of left thumbnail, which was slowly progressing over 2 years. He found it increasingly difficult to cut this hard and compact nail, even having to use a blade at times. On cutting, he noticed small bleeding points which dried to form blackish crusts.
On examination, there was a medial stump of the left thumbnail with yellowish discoloration and blackening. Distally, there was a compact subungual hyperkeratosis with blackish debris deposited [Figure 1].

- The frontal view of the left thumbnail showing the thickened, discolored, and partially cut off nail plate. Note the distal-free end of the nail plate and the yellowish discoloration seen dorsally, which has a sharp demarcation from the normal nail plate
Onychoscopy showed the presence of linear yellowish-brownish streaks running the length of the nail-plate stump with small discolored cavities, containing debris visualized distally [Figure 2]. Direct microscopy and fungal culture were negative. Radiograph showed no bony involvement. A magnetic resonance imaging (MRI) could not be done due to resource constraints.

- Dermatoscopic examination (onychoscopy): Dorsal view showing longitudinal parallel white lines (black arrows) along with an occasional splinter hemorrhage (red arrow), running through the stump of the nail-plate (AM4115MZT; ×150, polarizing view with linkage fluid)
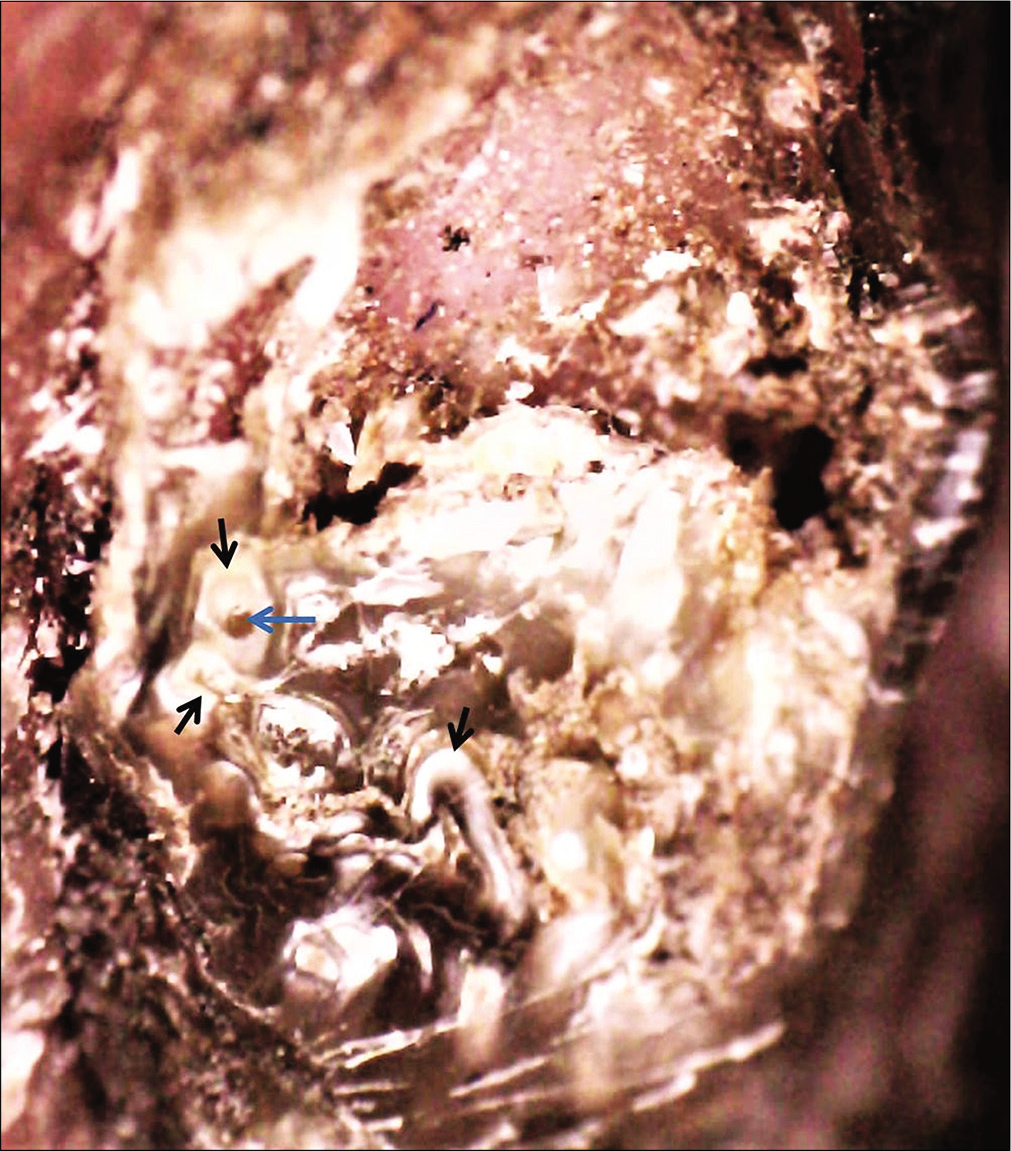
- Dermatoscopic examination (onychoscopy): Examination of the distal end showing thickening of the nail plate with multiple whitish channels/ cavities (keratinized) (black arrows) with dark dots (blue arrow) (Dino-Lite AM4115MZT; ×150, polarizing view with linkage fluid)
Partial avulsion of the affected nail plate revealed an underlying, “anemone-like” villous mass with small cavities in the proximal end of removed nail plate [Figure 3]. Both the nail plate and excised villous mass were examined histopathologically [Figure 4]. Histopathology revealed a thickened perforated nail plate apparently having multiple cavities. The villous mass was seen as a matrical tumor with multiple surface digitations and matrix epithelium lining. The underlying collagenous stroma was more cellular with fibrillary collagen superficially and dense, less cellular collagen in the deeper part of the tumor.

- Lateral partial avulsion of the affected nail plate. The avulsed stump shows an ireegular and grossly thick proximal margin

- The filiform mass (arrow head) arising from underneath the proximal nailfold can be seen after removal of nail plate
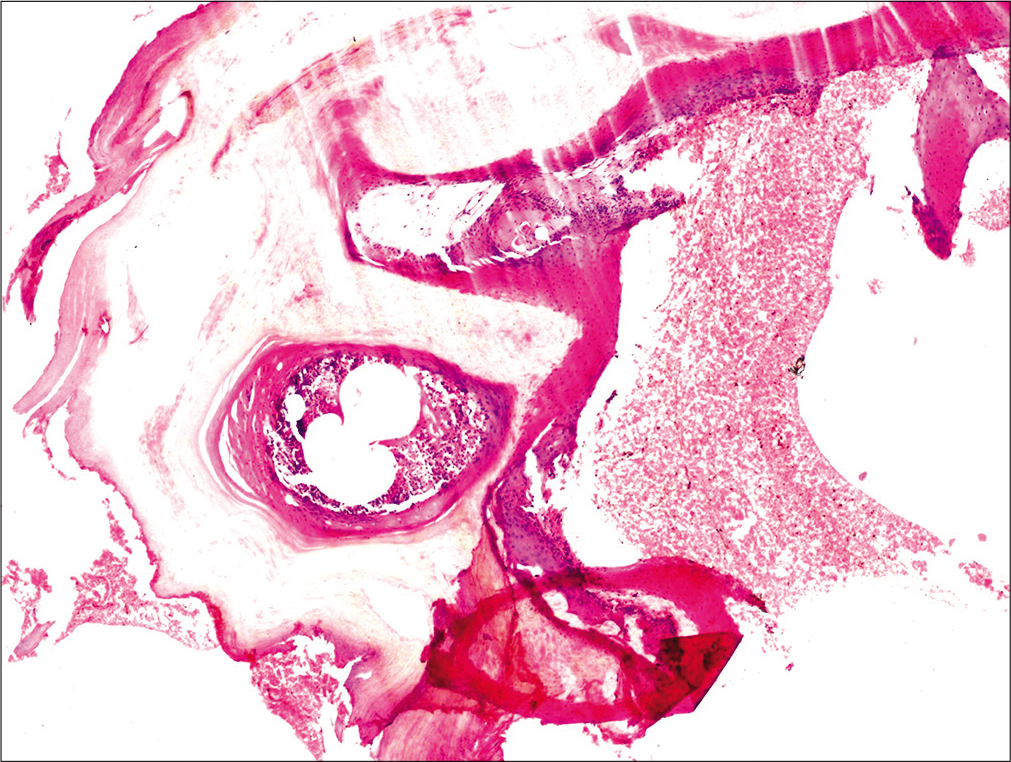
- Histopathological examination shows a thickened nail plate perforated by multiple cavities filled with serous contents (H and E, ×100)
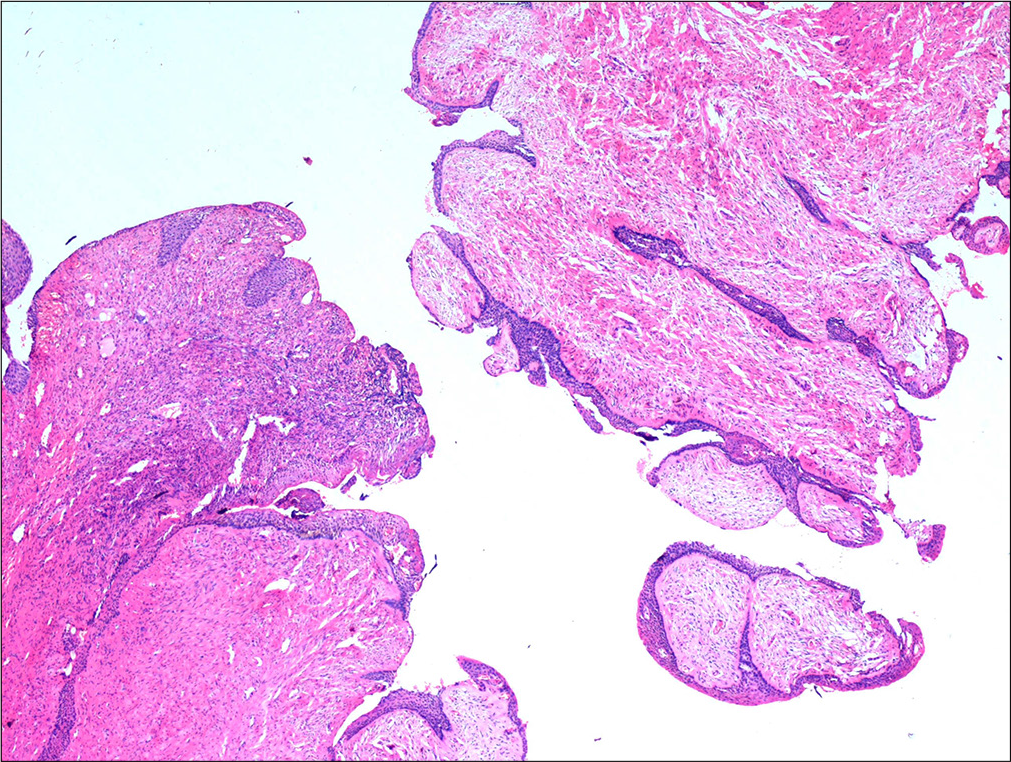
- Histopathological examination shows matrical tumor with multiple digitations on the surface, lined with matrix epithelium. The underlying collagenous stroma is more cellular with fibrillary collagen, superficially; while there is less cellularity and dense collagen in the deeper part of the tumor (H and E, ×100)
What Is Your Diagnosis?
Diagnosis
Onychomatricoma (onychomatrixoma).
Discussion
Onychomatricoma is a rare tumor arising from the nail matrix. It was first described in 1992.1 Subsequent to standardization of its terminology in 1995, only a few hundred cases have been described till now in literature, as it is probably less recognized by dermatologists and pathologists alike. The filamentous matrix tumor predominantly affects fingernails, growing distally as longitudinal channels within the nail plate. Studies show that it arises commonly in middle-aged women in the fifth decade, although other reports have shown no such sex predilection.2 The diagnosis is often delayed due to the slow growth of the tumor and the absence of pain. Many of these cases are misdiagnosed as onychomycosis and treated for long periods.
Clinically, onychomatricoma is mostly asymptomatic, but is characterized by the diagnostic tetrad of xanthonychia, longitudinal overcurvature, multiple splinter hemorrhages, and longitudinal ridging.3 The distal nail plate may show “woodworm”-like holes. Other diagnostic procedures include dermatoscopy of nail (onychoscopy), radiological imaging, and histopathology.
Onychoscopy shows the presence of perforations in the distal part of the nail plate (woodworm-like cavities), hemorrhagic striae and whitish longitudinal grooves within the nail plate (suggestive of tumor channels), and proximal and distal splinter hemorrhages.2 Plain skiagrams are generally normal, but ultrasonography can show the presence of hypoechoic tumoral lesion in the nail matrix with hyperechogenicity in the nail plate (corresponding to finger-like projections). MRI shows the characteristic invasive morphology of the tumor and is considered diagnostic.4
The excised tumor shows fibroepithelial morphology with two distinct zones: a proximal zone with deep matrix epithelial invaginations along with overlying ungual projections and the distal zone showing epithelial digitations originating from the matrix and perforating the nail plate.5 Such matrix proliferations correlate with the whitish longitudinal grooves within the nail plate, as seen on onychoscopy. These very same matricial projections with dried up blood present as the distally visible “woodworm cavities.” The tumor is both CD10 (a marker of onychodermis) and CD34 (expressed by dendritic or fibroepithelial-like mesenchymal cells) positive.3 A rare pigmented variant has also been described.6
The differential diagnoses include onychoblastoma,3 fibrokeratoma,4 periungual fibroma, subungual verruca vulgaris,3 and even squamous cell carcinoma. In longitudinal sections, the histopathology of onychomatricoma may be reminiscent of ungual fibrokeratomas; however, a fibrokeratoma lacks the multiple fibroepithelial projections and nail plate perforations characteristic of the onychomatricoma.4 Another distinguishing feature is the lack of the hyperplastic onychomatricial epithelium in the layer. These features also suggest that onychomatricoma may have a malignant potential, not hitherto known.7
The treatment for onychomatricoma is complete surgical excision. This requires the partial avulsion of the affected nail plate to visualize the underlying matrix growth which needs to be excised completely. Inclusion of some normal nail matrix proximal to the lesion is advised to help prevent local recurrences, even though the occurrence is rare. Subsequent nail scarring is dependent on the extent of the tumor and the extent of the growth. Very few long-term studies are available and mostly no recurrence has been reported. However, one should be aware of the continuum with potentially malignant onychomatricoma existing.7
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Onychomatrixoma, Filamentous tufted tumour in the matrix of a funnel-shaped nail: A new entity (report of three cases) Br J Dermatol. 1992;126:510-5.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma: Epidemiological and clinical findings in a large series of 30 cases. Br J Dermatol. 2015;173:1305-7.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma: A rare tumor of nail matrix. Ann Dermatol. 2016;28:237-41.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma: A tumor unknown to dermatologists. An Bras Dermatol. 2015;90:265-7.
- [CrossRef] [PubMed] [Google Scholar]
- The onychomatricoma: Additional histologic criteria and immunohistochemical study. Am J Dermatopathol. 2002;24:199-203.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented onychomatricoma: A rare pigmented nail unit tumor presenting as longitudinal melanonychia that has potential for misdiagnosis as melanoma. J Foot Ankle Surg. 2015;54:723-5.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma: Benign sporadic nail lesion or much more? Dermatol Online J. 2006;12:4.
- [Google Scholar]





