Translate this page into:
The enigma of eruptions: A papular puzzle
Corresponding author: Dr. Chirag Ashwin Desai, Department of Dermatology, Divya Sparsh Skin & Hair Clinic, Mumbai, Maharashtra, India. 83.chirag@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar P, Desai CA. The enigma of eruptions: A papular puzzle. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_55_2025
A 17-year-old male patient presented with an acute, itchy eruption of hyperpigmented papules and plaques, distributed symmetrically over the neck, anterior aspect of the shoulders, and cubital fossae. He also had scattered papules over the anterior trunk for the past 3 weeks. There was no history of any drug intake or systemic illness prior to the occurrence of lesions. Examination revealed multiple hyperpigmented annular small papules, coalescing at places to form plaques, with a raised border [Figures 1a, 1b]. Systemic examination was unremarkable. Dermoscopic examination revealed patchy areas of accentuation of the pigment network with overlying short brown lines, many showing acute angulations, surrounded by a narrow zone of hypopigmentation [Figure 1c]. Biopsy was taken from two lesions, one from a papular lesion on the anterior aspect of the right shoulder and another from a similar lesion on the left cubital fossa [Figures 2a and 2b].
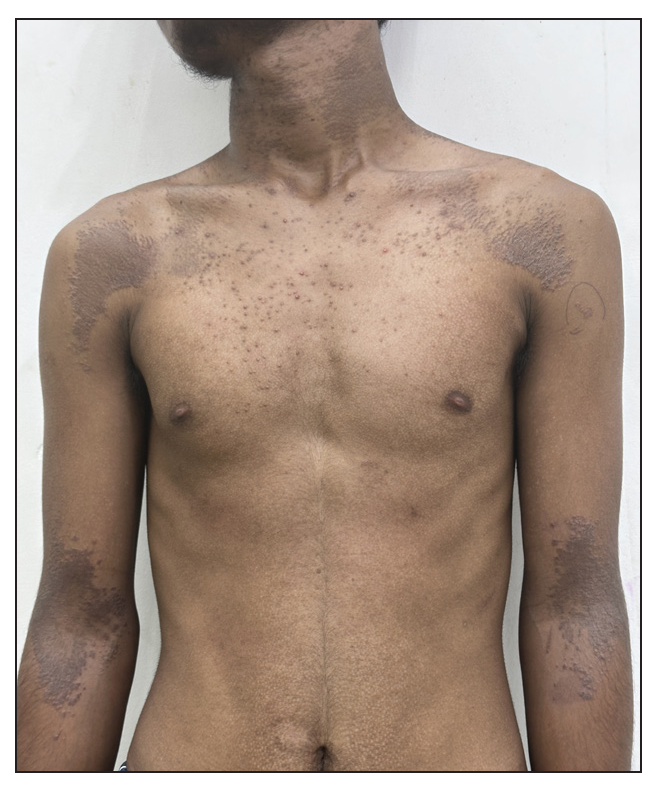
- Distribution of hyperpigmented papules and plaques on the body.

- Close-up of the coalescing lesions with raised borders in the left elbow.
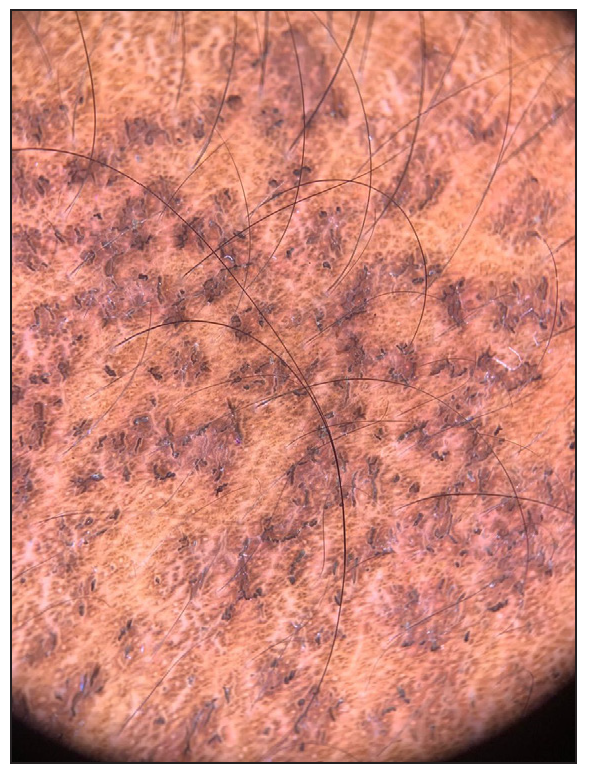
- Dermoscopy showing areas of accentuation of pigment network with overlying short brown lines, some angulated (Dermlite DL4, polarised, 10x).
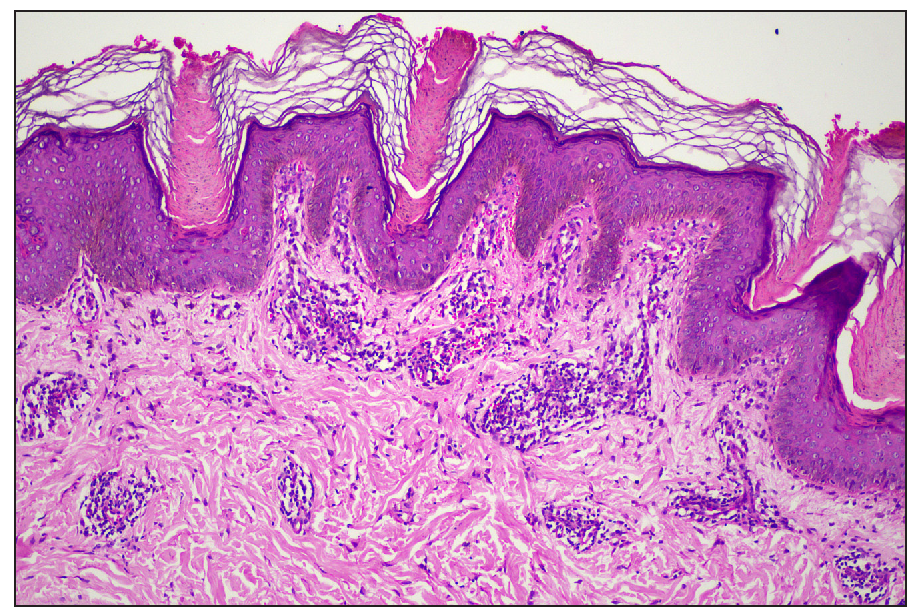
- Multiple epidermal invaginations with cornoid lamellae (Haematoxylin & eosin, 100x).
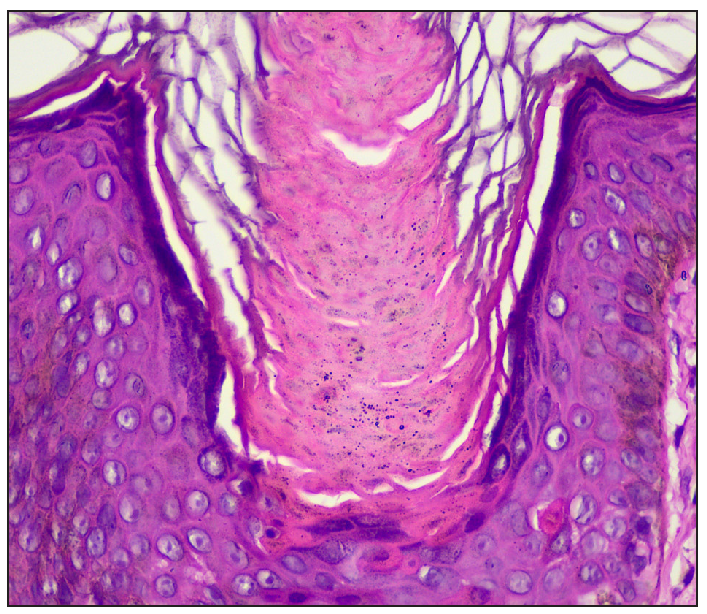
- Cornoid lamella with underlying dyskeratotic cells (Haematoxylin and eosin, 400x).
Answer
Diagnosis: Eruptive pruritic papular porokeratosis (EPPP)
Discussion
Eruptive pruritic papular porokeratosis (EPPP) was diagnosed based on clinico-dermoscopic and pathological correlation. Histopathology showed epidermis showed deep invaginations in multiple foci. Rising from the centre of these invaginations was a column of parakeratotic cells (cornoid lamella). The epidermis beneath the cornoid lamella had a diminished granular layer with scattered dyskeratotic cells, and the basal layer displayed subtle focal vacuolar changes. A moderately dense superficial and mid-perivascular lymphocytic infiltrate was seen in the dermis. These findings confirmed the diagnosis of porokeratosis [Figures 2a & 2b].
The clinical differential considered was granular parakeratosis; however, the keratotic rim and classical cornoid lamella revealed by dermoscopy and histopathology, respectively, helped in ruling out this condition.
EPPP is an acute eruptive and symptomatic variant of disseminated superficial porokeratosis. It was first described by Kanzaki et al.,1 and is similar to other porokeratosis variants in having typical histopathology, but the clinical presentation is different. EPPP is known to be associated with various internal malignancies like hepatocellular carcinoma, cholangiocarcinoma, ovarian carcinoma, and lymphoma, to name a few. These lesions subside with remission of malignancy, which includes EPPP in one of the paraneoplastic skin manifestations. EPPP may also affect patients on immunosuppressive treatment and those having pre-existing disseminated superficial porokeratosis.2 However, the patient under discussion was not on any immunosuppressants and also did not show any pre-existing variant of porokeratosis. Also, a thorough work-up including ultrasonography of the abdomen and pelvis, chest X-ray, and PET scan did not reveal any malignancy.
Very little is known about the pathogenesis of porokeratosis. Localised anomalous clone of epidermal cells may lead to dysplasia in this condition, as suggested by some workers. The body’s inflammatory response to this abnormal keratinocytic clone may be a cause of pruritus in EPPP.3 However, neither mast cells nor eosinophils are mandatory diagnostic criteria in dermal infiltrates of EPPP, as elucidated by the same authors.3 Dermal infiltrates of EPPP mainly comprise of CD4 and CD8 lymphocytes, as well as CD1a cells. It has been postulated that the presence of CD8 lymphocytes is mainly responsible for spontaneous regression of this condition.3
Most cases of EPPP spontaneously regress within 6 months. However, patients seek help due to pruritus. Various treatments like topical steroids, keratolytic agents, retinoids, 5-fluorouracil, calcipotriol, cryotherapy, systemic steroids, retinoids, tofacitinib, and abrocitinib have been tried.4,5
Our patient was treated with 10% urea-based cream and oral isotretinoin 20 mg for one month, which led to near complete resolution of the symptoms and lesions, after which the treatment was stopped [Figure 3]. We describe this case for its rarity.

- Complete resolution after one month of treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Eruptive pruritic papular porokeratosis. J Dermatol. 1992;19:109-12.
- [CrossRef] [PubMed] [Google Scholar]
- Eruptive disseminated porokeratosis: a new classification system. J Am Acad Dermatol. 2014;71:398-400.
- [CrossRef] [PubMed] [Google Scholar]
- Eruptive pruritic papular porokeratosis: A pruritic variant of porokeratosis. J Dermatol. 2006;33:813-6.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of eruptive pruritic papular porokeratosis in the elderly with tofacitinib: A case report. Clin Cosmet Investig Dermatol. 2023;16:1741-7.
- [CrossRef] [PubMed] [Google Scholar]
- A report of eruptive pruritic papular porokeratosis treated with abrocitinib. Clin Cosmet Investig Dermatol. 2023;16:2223-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





