Translate this page into:
The mechanism of oxidative stress in keloid fibroblasts and the experimental study of early application of angiotensin-converting enzyme inhibitor
Corresponding author: Dr. Chen Junjie, Department of Aesthetic and Plastic Burn Surgery, West China Hospital of Sichuan University, Chengdu, China, 308939298@qq.com
-
Received: ,
Accepted: ,
How to cite this article: Hong L, Junjie C, Pengyu Z, Ping L, Wei C. The mechanism of oxidative stress in keloid fibroblasts and the experimental study of early application of angiotensin-converting enzyme inhibitor. Indian J Dermatol Venereol Leprol 2023;89:842-9.
Abstract
Objective
To investigate the protective effects of an angiotensin-converting enzyme inhibitor after inducing oxidative stress on keloid fibroblasts.
Methods
Primary keloid fibroblasts were isolated and cultured by enzyme digestion combined with the tissue adhesion method in vitro, and the third to fifth generations of cells were selected for the experiment. For 24 hours, keloid fibroblasts were treated with different concentrations of hydrogen peroxide. Different concentrations of angiotensin-converting enzyme inhibitor were added to the keloid fibroblast culture medium, and then the cells were treated with hydrogen peroxide for 24 hours.
Results
With the increase of hydrogen peroxide concentration, the growth of keloid fibroblasts was inhibited and the levels of malondialdehyde, superoxide dismutase, and reactive oxygen species increased gradually, accompanied by an increase in the expression of nicotinamide adenine dinucleotide phosphate oxidase and collagen I mRNA. The expression of nicotinamide adenine dinucleotide phosphate oxidase-mRNA in keloid fibroblasts and the formation of reactive oxygen species in keloid fibroblasts were induced by different concentrations of angiotensin II, and the most significant effect was at 10–5 mmol/mL. The effects of diphenyleneiodonium chloride (NOX inhibitor), N-acetylcysteine (reactive oxygen species inhibitor) and nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase) RNA treatment on angiotensin II-induced nicotinamide adenine dinucleotide phosphate oxidase and collagen I increased significantly. Hydrogen peroxide and angiotensin II alone or combined can induce NADPH oxidase and reactive oxygen species expression in keloid fibroblasts. When the angiotensin-converting enzyme inhibitor was added, the expression of NADPH oxidase and reactive oxygen species in keloid induced by hydrogen peroxide and angiotensin II could be inhibited.
Conclusion
Oxidative stress can lead to increased expression of reactive oxygen species, NADPH oxidase and collagen I in keloid fibroblasts, suggesting oxidative stress mediates the migration of human keloid fibroblasts and extracellular matrix synthesis.
Keywords
Angiotensin II
angiotensin-converting enzyme inhibitor
fibroblast
hydrogen peroxide
keloid
oxidative stress
Plain Language Summary
This study investigates the protective effects of angiotensin-converting enzyme inhibitors after inducing oxidative stress on keloid fibroblasts. Primary keloid fibroblasts were isolated and cultured by enzyme digestion combined with the tissue adhesion method in vitro, and the expression of nicotinamide adenine dinucleotide phosphate oxidase-mRNA in keloid fibroblasts and the formation of reactive oxygen species in keloid fibroblasts were induced by different concentrations of angiotensin-II. The most significant effect was at 10–5 mmol/mL. The effects of diphenyleneiodonium chloride, N-acetylcysteine and nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase) RNA treatment on angiotensin II-induced NADPH oxidase and collagen I increased significantly. Hydrogen peroxide and angiotensin II alone or combined can induce NADPH oxidase and reactive oxygen species expression in keloid fibroblasts. When an angiotensin-converting enzyme inhibitor was added, the expression of NADPH oxidase and reactive oxygen species in keloid induced by hydrogen peroxide and angiotensin II could be inhibited. Angiotensin II can induce the expression of NADPH oxidase and the generation of reactive oxygen species in keloid fibroblasts, suggesting that angiotensin II activation of NADPH oxidase may induce reactive oxygen species to mediate the migration of keloid fibroblasts and the synthesis of extracellular matrix. The application of angiotensin-converting enzyme inhibitor after oxidative stress can inhibit the production of NADPH oxidase and reactive oxygen species in keloid fibroblasts and has a certain anti-fibrosis effect.
Introduction
In recent years, the role of oxidative stress response in chronic inflammatory fibrosis of various organs and tissues has attracted more and more attention. A large number of studies have found that the oxidative stress in skin keloid tissue is significantly increased and the antioxidants in plasma are significantly reduced, suggesting that the imbalance of oxidation/antioxidation may play an important role in skin fibrosis.1,2
Angiotensin-converting enzyme is a dipeptide carboxyl peptidase that can convert angiotensin I into angiotensin II. Angiotensin II is one of the strongest stimuli causing oxidative stress. Existing evidence shows that angiotensin II participates in the formation of atherosclerosis, cardiac fibrosis and liver fibrosis by inducing the production of reactive oxygen species by vascular smooth muscle cells, endothelial cells and hepatic stellate cells.3–6 In light of these observations, we speculate that reactive oxygen species may also be involved in angiotensin II-induced skin fibrosis. We used hydrogen peroxide to simulate the process of oxidative stress in keloid fibroblasts to observe whether angiotensin II can activate nicotinamide adenine dinucleotide phosphate oxidase to produce reactive oxygen species in keloid fibroblasts and whether nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase) derived reactive oxygen species are involved in angiotensin II-induced keloid fibroblast proliferation and extracellular matrix synthesis. We also investigated if the early application of angiotensin-converting enzyme inhibitors can have an anti-fibrosis effect by reducing reactive oxygen species in keloid fibroblasts and provide an experimental basis for the clinical application of these drugs against skin fibrosis.
Methods
Experimental methods and detection indicators
In vitro experiment: primary human keloid fibroblasts were isolated and cultured by enzyme digestion combined with the tissue adhesion method at the department of medical cosmetology, Chengdu Second People’s Hospital, Chengdu city, China. The third to fifth generations of cells were used for the following experiments.
Experiment 1
-
Tissue used: human keloid, human keloid cells were isolated by the collagenase method.
-
Identification: fluorescent staining of fibroblast markers (a-SMA, vimentin). Harvest: P3–P5 cells.
Experiment 2
-
Cells used: primary human keloid fibroblasts. Methods: human keloid fibroblasts were treated with hydrogen peroxide (0, 20, 50, 100, 200 and 500 µmol/L) for 24 hours.
-
Test indicators and methods: (1) The growth of cells was detected by the CCK8 method (0 hours, 8 hours, 16 hours and 24 hours); (2) The concentrations of malondialdehyde and superoxide dismutase in culture medium were detected by enzyme-linked immunosorbent assay; (3) Apoptosis was detected by flow cytometry; (4) Real-time polymerase chain reaction and western blot were used to detect the expression of NADPH oxidase and collagen I protein; (5) The expression of reactive oxygen species was detected by flow cytometry or immunofluorescence.
Experiment 3
-
Cells used: primary human keloid fibroblasts. Methods: human keloid fibroblasts were treated with angiotensin II (10–9, 10–7 and 10–5 mmol/M1), diphenyleneiodonium chloride (NOX inhibitor), N-acetylcysteine, a reactive oxygen species inhibitor, and NADPH oxidase-siRNA for 24 hours.
-
Test indicators and methods: (1) The growth of cells was detected by CCK8 method (0 hours, 8 hours, 16 hours and 24 hours); (2) The expression of reactive oxygen species was detected by flow cytometry or immunofluorescence; (3) Real-time polymerase chain reaction and western blot were used to detect the expression of NADPH oxidase, collagen I protein and catalase.
-
Expected results: different concentrations of angiotensin II (10–9, 10–7 and 10–5 mmol/M1) can promote the expression of NADPH oxidase protein and the production of reactive oxygen species. Diphenyleneiodonium chloride (NOX inhibitor) and N-acetylcysteine (reactive oxygen species inhibitor) significantly inhibited angiotensin II-induced cell migration and increased collagen expression. Not only can diphenyleneiodonium chloride and N-acetylcysteine reduce the production of reactive oxygen species induced by angiotensin II (10 mmol/ML), but also NADPH oxidase-siRNA can inhibit the production of reactive oxygen species induced by angiotensin II. At the same time, angiotensin II can significantly downregulate the expression of catalase in a time and dose-dependent manner.
Experiment 4
-
Cells used: primary human keloid fibroblasts. Methods: human keloid fibroblasts were treated with hydrogen peroxide (the best concentration) for 24 hours. Then, different concentrations of angiotensin-converting enzyme inhibitors were added to stimulate the cells for 24 hours. The angiotensin-converting enzyme inhibitor mainly used in this experiment was captopril.
-
Test indicators and methods: (1) The growth of cells was detected by the CCK8 method (0 hours, 8 hours, 16 hours and 24 hours); (2) The concentrations of malondialdehyde and superoxide dismutase in culture medium were detected by enzyme-linked immunosorbent assay; (3) Apoptosis was detected by flow cytometry; (4) Real-time polymerase chain reaction and western blot were used to detect the expression of nicotinamide adenine dinucleotide phosphate oxidase, collagen I protein and catalase. (5) The expression of reactive oxygen species was detected by flow cytometry or immunofluorescence.
-
Expected results: compared with the control group, after fibroblast oxidative stress pre-treatment, different concentrations of angiotensin-converting enzyme inhibitor stimulated cells for 24 hours, and they could significantly inhibit the migration and collagen synthesis of angiotensin II. A fluorescence spectrophotometer was used to reduce the expression of nicotinamide adenine dinucleotide phosphate oxidase, collagen I protein, catalase and reactive oxygen species.
Statistical methods
The experimental data are expressed in x ± s and SPSS 24.0 software was used to analyze the data. One-way analysis of variance was used among the three groups, and Q-test was considered to be used for comparison between the groups, P < 0.05 was significant.
Results
Cell proliferation
We studied the effects of hydrogen peroxide and angiotensin II treatment on the growth of keloid fibroblasts by the CCK8 method. CCK8 was tested at 0 hours, 8 hours, 16 hours and 24 hours, respectively, and the growth curve after transfection was drawn according to the above results. We found that after treating keloid fibroblasts with hydrogen peroxide (0, 20, 50, 100, 200 and 500 mol/L) and angiotensin II (10–9, 10–7 and 10–5 mmol/mL), the cell activity of each concentration group was inhibited to varying degrees, and the inhibition of hydrogen peroxide and angiotensin II on the activity of keloid fibroblasts was dose-dependent. The proliferation of keloid fibroblasts decreased gradually with the extension of hydrogen peroxide and angiotensin II treatment times. Human keloid fibroblasts were treated with hydrogen peroxide (the best concentration was 200 mol/L) for 24 hours, and then stimulated with different concentrations of an angiotensin-converting enzyme inhibitor (10–9, 10–7, and 10–5 mmol/ml) for 24 hours. The cell activity of each concentration group of angiotensin-converting enzyme inhibitors can improve the effect of hydrogen peroxide-induced keloid fibroblast proliferation to varying degrees.
Change of malondialdehyde and superoxide dismutase content
In order to study the effects of hydrogen peroxide treatment simulating oxidative stress and angiotensin II treatment on keloid fibroblasts, we detected the levels of malondialdehyde and superoxide dismutase in keloid fibroblasts after oxidative stress [Figures 1 and 2]. We found that after keloid fibroblasts were treated with hydrogen peroxide (0, 20, 50, 100, 200 and 500 µmol/L) and angiotensin II (10–9, 10–7 and 10–5 mmol/mL) for 24 hours, the content of malondialdehyde in the culture medium gradually increased with the increase of hydrogen peroxide treatment concentration. After keloid fibroblasts were treated with different concentrations of hydrogen peroxide and angiotensin II for 24 hours, the concentration of superoxide dismutase was upregulated to varying degrees, and there was a significant difference in the level of superoxide dismutase between the concentration groups. Human keloid fibroblasts were treated with hydrogen peroxide (the best concentration was 200 µmol/L) for 24 hours, and then stimulated with different concentrations of an angiotensin-converting enzyme inhibitor (10–9, 10–7 and 10–5 mmol/mL) for 24 hours. We found that the malondialdehyde content level of the culture medium gradually decreased with the intervention of an angiotensin-converting enzyme inhibitor, while the superoxide dismutase concentration did not change significantly [Figure 3].

- Contents of MDA and SOD in keloid fibroblasts. After treating keloid fibroblasts with hydrogen peroxide (0, 20, 50, 100, 200 and 500 µmol/L) for 24 hours, the contents of MDA and SOD in the culture medium were. The content of MDA increased gradually with the increase of hydrogen peroxide treatment concentration. Different concentrations of hydrogen peroxide treatment upregulated the SOD of keloid fibroblasts, but there was no significant difference in the SOD level between the concentration groups. MDA, Malondialdehyde; SOD, Superoxide dismutase
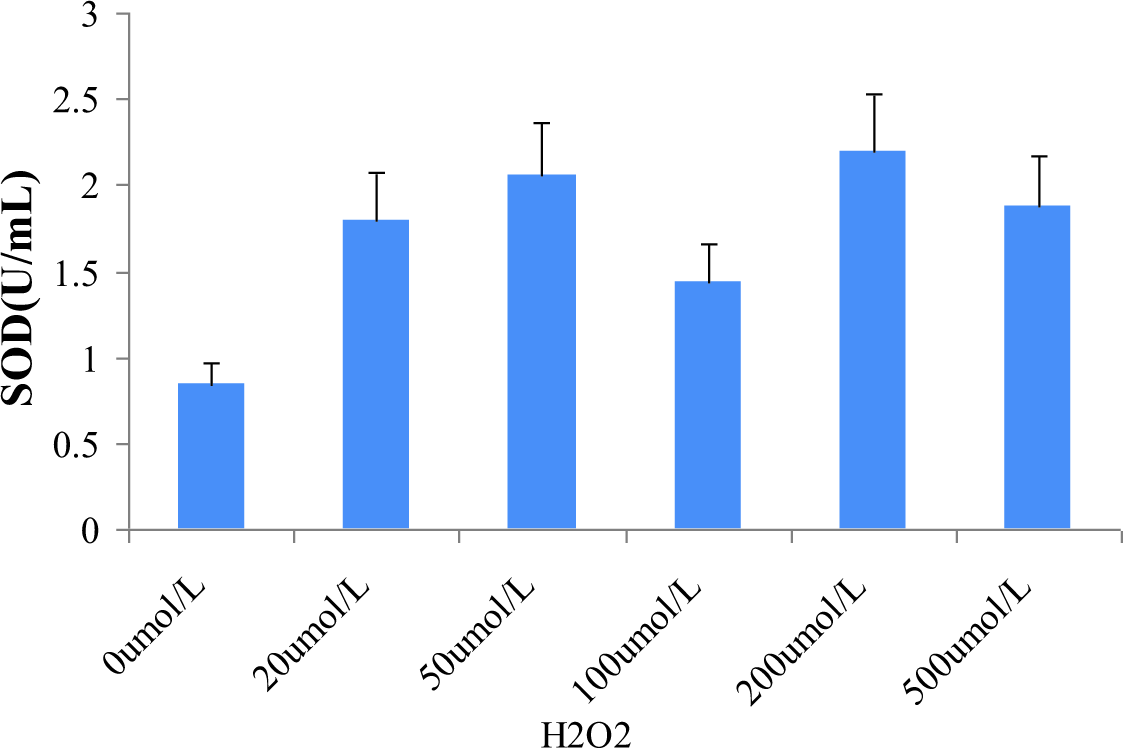
- Contents of SOD in keloid fibroblasts

- Contents of MDA and SOD in keloid fibroblasts. After Ang II (10–9, 10–7 and 10–5 mmol/M1) treated keloid fibroblasts alone and treated keloid fibroblasts with DPI (NOX inhibitor), NAC (ROS inhibitor) and NOX4 siRNA for 24 hours, the contents of MDA and SOD in the culture medium. Ang II, Angiotensin II; DPI, Diphenyleneiodonium chloride; MDA, Malondialdehyde; NAC, N-acetylcysteine; NOX4, Nicotinamide adenine dinucleotide phosphate; ROS, Reactive oxygen species; SOD, Superoxide dismutase
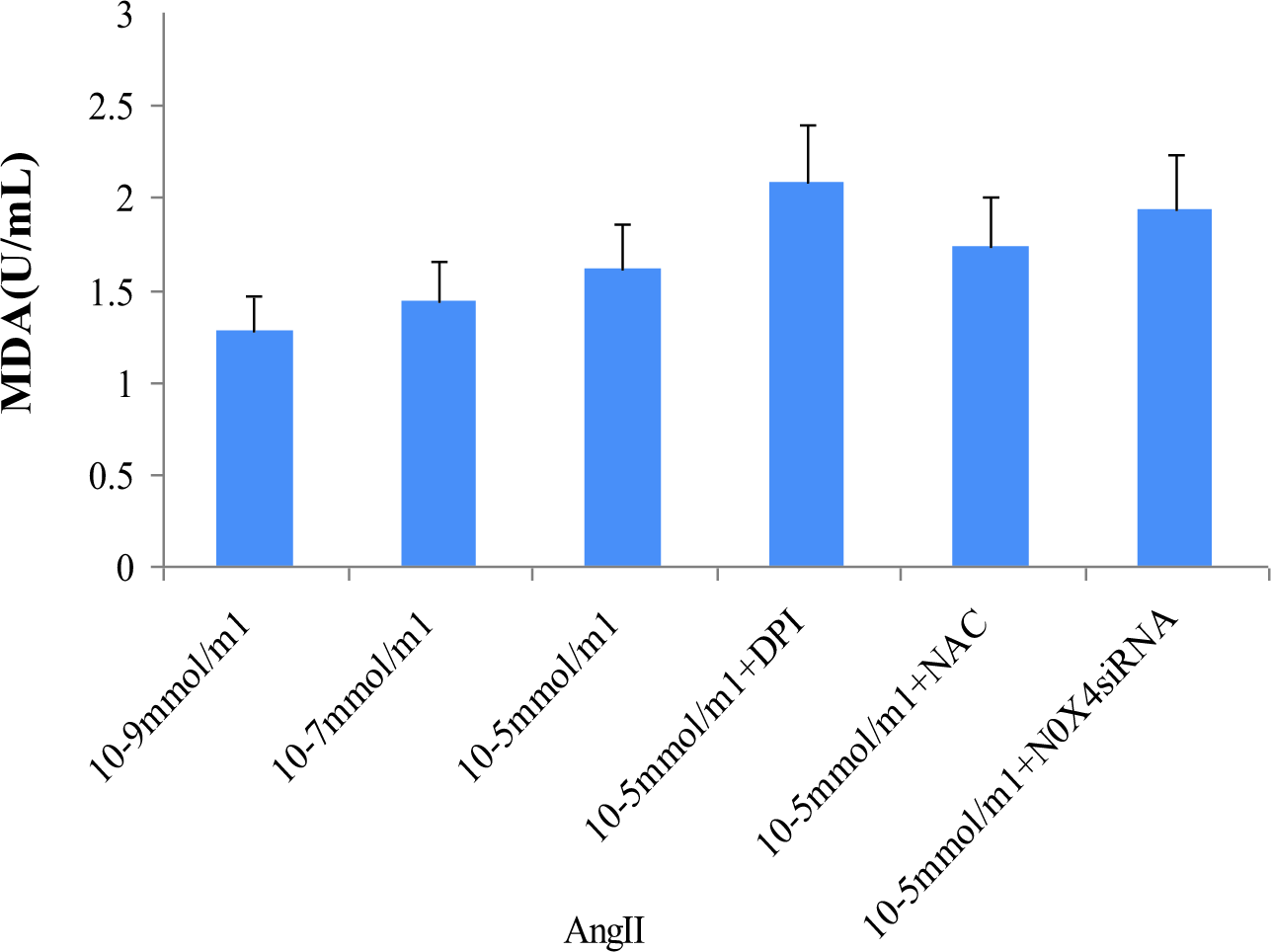
- Contents of MDA in keloid fibroblasts after Angiotensin II treatment

- Contents of MDA and SOD in keloid fibroblasts. Different concentrations of ACEI can significantly inhibit the production of SOD in keloid fibroblasts induced by hydrogen peroxide. It has no obvious effect on MDA. ACEI, Angiotensin-converting enzyme inhibitor; MDA, Malondialdehyde; SOD, Superoxide dismutase
Changes of apoptosis level
We used annexin V-FITC/PI double staining to detect the effects of hydrogen peroxide and angiotensin II treatment on the apoptosis of keloid fibroblasts. Annexin V-FITC/PI labelling was performed 24 hours after treatment. Flow cytometry showed that different concentrations of hydrogen peroxide and angiotensin II treatment could significantly increase the early and late apoptosis rates of keloid fibroblasts. The total apoptosis rate of keloid fibroblasts increased gradually with the increase in hydrogen peroxide treatment concentration.
Hydrogen peroxide (200 µmol/L) induced oxidative stress in keloid fibroblasts. Different concentrations of the angiotensin-converting enzyme inhibitor (10–9, 10–7 and 10–5 mmol/mL) can significantly inhibit the apoptosis of keloid fibroblasts, and their effect is negatively correlated with the concentration of angiotensin-converting enzyme inhibitor [Figure 4].

- Apoptosis of keloid fibroblasts. After keloid fibroblasts were treated with hydrogen peroxide (H2O2) (0, 20, 50, 100, 200 and 500 µmol/L) for 24 hours, they were labelled with annexin V-FITC/PI. The apoptosis rate of keloid fibroblasts was detected by flow cytometry. Different concentrations of hydrogen peroxide treatment can significantly increase the apoptosis of keloid fibroblasts
Expression of nicotinamide adenine dinucleotide phosphate oxidase and collagen I mRNA
The catalytic production of nicotinamide adenine dinucleotide phosphate oxidase (NOX) and the synthesis of extracellular matrix in keloid fibroblasts cause oxidative damage and fibrosis of keloid fibroblasts. After keloid fibroblasts were treated with hydrogen peroxide (0, 20, 50, 100, 200 and 500 µmol/L) and angiotensin II (10–9, 10–7 and 10–5 mmol/mL) for 24 hours, the mRNA levels of NADPH oxidase and collagen I [Figures 5 and 6] showed that different concentrations of hydrogen peroxide and angiotensin II treatment could significantly increase the mRNA expression of NADPH oxidase and collagen I in keloid fibroblasts. The mRNA expression level of collagen I in keloid fibroblasts was the most significant when treated with 200 µmol/L hydrogen peroxide (P < 0.05). Hydrogen peroxide (200 umol/L) induced oxidative stress response in keloid fibroblasts, and different concentrations of angiotensin-converting enzyme inhibitor were used to intervene in keloid fibroblasts, and quantitative fluorescence polymerease chain reaction was used to detect NADPH oxidase and collagen I expression in keloid fibroblasts after intervention [Figure 6]. The introduction of angiotensin-converting enzyme inhibitor (10–9, 10–7 and 10–5 mol/M1) could significantly inhibit the expression of NADPH oxidase and collagen I in keloid fibroblasts, which was negatively correlated with the concentration of angiotensin-converting enzyme inhibitor.

- Expression of NOX4 and collagen I mRNA in keloid fibroblasts. After keloid fibroblasts were treated with hydrogen peroxide (0, 20, 50, 100, 200 and 500 µmol/L) for 24 hours, the mRNA levels of NOX4 and collagen I were detected by fluorescence quantitative PCR. Different concentrations of hydrogen peroxide treatment can significantly increase the mRNA expression of NOX4 and collagen I in keloid fibroblasts. The mRNA expression level of collagen I in keloid fibroblasts was the most significant when treated with 200 µmol/L hydrogen peroxide (P < 0.05) NOX4, Nicotinamide adenine dinucleotide phosphate oxidase; PCR, Polymerase chain reaction

- Expression of NOX4 and collagen I mRNA in keloid fibroblasts. After treating keloid fibroblasts with Ang II (10–9, 10–7 and 10–5 mmol/M1) alone and keloid fibroblasts with DPI (NOX inhibitor), NAC (ROS inhibitor) and NOX4 siRNA for 24 hours, the mRNA levels of NOX4 and collagen I were detected by fluorescence quantitative PCR. Ang II, Angiotensin II; DPI, Diphenyleneiodonium chloride; NOX4, Nicotinamide adenine dinucleotide phosphate oxidase; PCR, Polymerase chain reaction; ROS, Reactive oxygen species
Changes of reactive oxygen species expression in cells
In order to study the effect of hydrogen peroxide treatment on reactive oxygen species active molecules in keloid fibroblasts, a reactive oxygen species fluorescent probe was used to mark the content of reactive oxygen species in cells, and the expression level of reactive oxygen species in cells was detected by flow cytometry and fluorescence microscopy [Figures 7 and 8]. The results showed that different concentrations of hydrogen peroxide treatment could significantly increase the expression level of reactive oxygen species in keloid fibroblasts. The level of reactive oxygen species in cells treated with a high concentration of hydrogen peroxide (100, 200 and 500 µmol/L) was significantly higher than that in cells treated with a low concentration of hydrogen peroxide (20 and 50 µmol/L). Our experiment showed that oxidative stress can induce the production of reactive oxygen species (ROS) in keloid fibroblasts, and there is a correlation between the concentration of hydrogen peroxide treatment and the production level of ROS in keloid fibroblasts. Hydrogen peroxide (200 µmol/L) induced an oxidative stress response in keloid fibroblasts, and intervened keloid fibroblasts with different concentrations of angiotensin-converting enzyme inhibitor. Different concentrations of angiotensin-converting enzyme inhibitor significantly inhibited the production of reactive oxygen species in keloid fibroblasts, and its effect was negatively correlated with the concentration of angiotensin-converting enzyme inhibitor.

- Expression of NOX4 and collagen I mRNA in keloid fibroblasts. The mRNA levels of NOX4 and collagen I were detected by fluorescence quantitative PCR. Different concentrations of ACEI can significantly inhibit the expression of NOX4 and collagen I in keloid fibroblasts induced by hydrogen peroxide. ACEI, Angiotensin-converting enzyme inhibitor; NOX4, Nicotinamide adenine dinucleotide phosphate oxidase; PCR, Polymerase chain reaction

- Molecular level of ROS activity in keloid fibroblasts. After the cells were labelled with ROS fluorescent probe, the positive proportion of ROS expression in keloid fibroblasts was detected by flow cytometry. ROS, Reactive oxygen species

- ROS fluorescence diagram of keloid fibroblasts. Keloid fibroblasts treated with Ang II (0, 10–9, 10–7 and 10–5 mmol/M1) alone and keloid fibroblasts treated with DPI (NOX inhibitor), NAC (ROS inhibitor) and NOX4-siRNA for 24 hours. After labelling the cells with ROS fluorescent probe, the expression of green fluorescence was observed by fluorescence microscope. The specific results of cells in each group are as follows (×400). Ang II, Angiotensin II; DPI, Diphenyleneiodonium chloride; NAC, N-acetylcysteine; NOX4, Nicotinamide adenine dinucleotide phosphate oxidase; ROS, Reactive oxygen species
Discussion
In recent years, the role of oxidative stress response in chronic inflammatory fibrosis of various organs and tissues has attracted more and more attention. A large number of studies have found that the level of oxidative stress in skin keloid tissue is significantly increased and the antioxidants in plasma are significantly reduced,7 –10 suggesting that the imbalance of oxidation/antioxidation may play an important role in skin keloid fibrosis.11 –14 The renin-angiotensin system is an important system for regulating blood pressure in the body, and the newly discovered angiotensin-converting enzyme 2 is the key factor.1 Angiotensin-converting enzyme is a dipeptide carboxyl peptidase which can convert angiotensin I to angiotensin II. Studies have shown that angiotensin II is one of the strongest stimuli causing oxidative stress.10 –12 ,15 Angiotensin-converting enzyme inhibitor can inhibit the conversion of angiotensin I to angiotensin II. The discovery of angiotensin-converting enzyme inhibitor has injected new interest into renin-angiotensin system and opened up a new direction in the research of renin-angiotensin system, oxidative stress, and hypertension.10 ,13 –15 Angiotensin-converting enzyme inhibitor reduces the production of angiotensin I by regulating the metabolism of angiotensin peptides, which increases the activity of nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase) in the body. It leads to increased production of reactive oxygen species in the cardiovascular and renal systems and enhanced oxidative stress in the body.10 ,13 –15 NADPH oxidase activity increased significantly in angiotensin-converting enzyme 2 knockout mice, and an angiotensin II type 1 receptor blocker completely inhibited NADPH oxidase activity in these mice,14 ,15 indicating that angiotensin-converting enzyme inhibitor gene regulation of NADPH oxidase activity may be mediated by blocking angiotensin I-angiotensin II type 1 receptor signal. The angiotensin-converting enzyme inhibitor gene can reduce reactive oxygen species production by antagonizing the effect of angiotensin I, so as to exert a certain antioxidant effect. Recent studies have shown that in mice with chronic heart failure, overexpression of angiotensin-converting enzyme inhibitor in hypothalamic paraoptic nucleus cells can upregulate the activity of nitric oxide synthase in this region and increase the concentration of nitric oxide in cerebrospinal fluid so as to reduce the level of oxidative stress. The knockout of the angiotensin-converting enzyme inhibitor gene in aging mice increases the level of oxidative stress in various brain cells and cause oxidative damage to brain tissue.16 Therefore, this experiment attempted to use hydrogen peroxide to simulate the oxidative stress process of keloid fibroblasts and used angiotensin-converting enzyme inhibitor to inhibit the formation of angiotensin I, so as to protect keloid fibroblasts and reduce the production of reactive oxygen species, thereby reducing oxidative stress.
The existence of local angiotensin and its receptor in skin tissue indicates that there is an independent renin-angiotensin system in the skin. Existing studies have shown that the renin-angiotensin system plays an important role in skin wound repair and later remodelling, which is closely related to the occurrence and development of scars. With the deepening of our understanding of the mechanism of scar formation we can develop new methods and ideas for the prevention and treatment of scars. It is believed that angiotensin-converting enzyme inhibitor and angiotensin II type 1 receptor blockers have broad prospects in the prevention and treatment of skin fibrosis. After keloid oxidative stress pretreatment, cells were exposed to different concentrations of angiotensin-converting enzyme inhibitor for 24 hours. They could significantly inhibit the migration and collagen synthesis of keloid fibroblasts. The expression of NADPH oxidase and collagen I protein, and the expression of reactive oxygen species were downregulated by fluorescence spectrophotometer.17 In previous studies, it has been reported that the process of oxidative stress plays a role in the chronic fibrosis of various organs and tissues. This paper speculates that oxidative stress may also be involved in angiotensin II-induced skin fibrosis (i.e., formation of skin keloids). This experiment studied the mechanism of oxidative stress on keloid fibroblasts, and showed that angiotensin-converting enzyme inhibitor can reduce reactive oxygen species in keloid fibroblasts undergoing oxidative stress. In this experiment, it was detected that the levels of NADPH oxidase, collagen I and reactive oxygen species decreased with the increase of angiotensin-converting enzyme inhibitor concentration. The content of collagen I in keloid fibroblasts reflects the degree of fibrosis, and the levels of nicotinamide adenine dinucleotide phosphate oxidase and reactive oxygen species reflect the degree of cellular oxidative stress. Therefore, through this experiment, we have reason to believe that angiotensin-converting enzyme inhibitor can reduce dermal fibrosis by reducing keloid oxidative stress response, but the specific mechanism remains to be studied.
Limitations of study: We did not carry out the in vivo test for keloid fibroblast so the keloid fibroblast protein molecular level was not performed.
Conclusions
Oxidative stress can lead to increased expression of reactive oxygen species, NADPH oxidase and collagen I in keloid fibroblasts. It also promotes cell apoptosis, suggesting oxidative stress mediates the migration of human keloid fibroblasts and extracellular matrix synthesis. Angiotensin II can induce the expression of NADPH oxidase and the generation of reactive oxygen species in keloid fibroblasts, suggesting that angiotensin II activation of NADPH oxidase may induce reactive oxygen species to mediate the migration of keloid fibroblasts and the synthesis of extracellular matrix. The application of angiotensin-converting enzyme inhibitor after oxidative stress can inhibit the production of NADPH oxidase and reactive oxygen species in keloid fibroblasts and has a certain anti-fibrosis effect.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The most current algorithms for the treatment and prevention of hypertrophic scars and keloids. Plast Reconstr Surg. 2010;125:557-68.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Superoxide and hydrogen peroxide in relation to mammalian cell proliferation. Free Radic Biol Med. 1995;18:775-94.
- [CrossRef] [PubMed] [Google Scholar]
- Distribution of type-1 and type-2 angiotensin receptors in the normal human lung and in lungs from patients with chronic obstructive pulmonary disease. Histochem Cell Biol. 2001;115:117-24.
- [CrossRef] [PubMed] [Google Scholar]
- Angiotensin II and the fibroproliferative response to acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2004;286:L156-64.
- [CrossRef] [PubMed] [Google Scholar]
- Reduction of bleomycin induced lung fibrosis by candesartan cilexetil, an angiotensin II type 1 receptor antagonist. Thorax. 2004;59:31-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cytostatic properties of some angiotensin I converting enzyme inhibitors and of angiotensin II type I receptor antagonists. Curr Pharm Des. 2003;9:751-61.
- [CrossRef] [PubMed] [Google Scholar]
- Genetic deletion of AT2 receptor antagonizes angiotensin II-induced apoptosis in fibroblasts of mouse embryo. Biochem Biophys Res Commun. 1998;250:72-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of angiotensin II receptor signaling during skin wound healing. Am J Pathol. 2004;165:1653-62.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Oxidative stress and hypertension: Current concepts. Curr Hypertens Rep. 2010;12:135-42.
- [CrossRef] [PubMed] [Google Scholar]
- Angiotensin-(1–7)—angiotensin-converting enzyme 2 attenuates reactive oxygen species formation to angiotensin II within the cell nucleus. Hypertension. 2010;55:166-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevention of angiotensin II-mediated renal oxidative stress, inflammation, and fibrosis by angiotensin-converting enzyme 2. Hypertension. 2011;57:314-22.
- [CrossRef] [PubMed] [Google Scholar]
- Angiotensin-converting enzyme 2 suppresses pathological hypertrophy, myocardial fibrosis, and cardiac dysfunction. Circulation. 2010;122:717-28.
- [CrossRef] [PubMed] [Google Scholar]
- Oxidative stress is a critical mediator of the angiotensin II signal in human neutrophils: Involvement of mitogen-activated protein kinase, calcineurin, and the transcription factor NF-kappaB. Blood. 2003;102:662-71.
- [CrossRef] [PubMed] [Google Scholar]
- Redox signaling involving NADPH oxidase-derived reactive oxygen species. Biochem Soc Trans. 2006;34:960-64.
- [CrossRef] [PubMed] [Google Scholar]
- Brain-selective overexpression of human angiotensin-converting enzyme type 2 attenuates neurogenic hypertension. Circ Res. 2010;106:373-82.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Angiotensin-converting enzyme 2: Central regulator for cardiovascular function. Curr Hypertens Rep. 2010;12:170-75.
- [CrossRef] [Google Scholar]
- The role of the renin-angiotensin system and vitamin D in keloid disorder—A review. Front Surg. 2019;6:67.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






